Abstract
Preeclampsia is a potentially fatal complication of human pregnancy characterized by hypertension, proteinuria, and edema. Placental oxidative stress is a key element in the pathogenesis of the syndrome and results in the release of a cocktail of factors, including proinflammatory cytokines and apoptotic debris, that in turn cause activation of the maternal endothelium. The intermediary molecular mechanisms underlying this release are unknown, but they represent a potential target for therapeutic interventions. We examined activation of signaling pathways during hypoxia-reoxygenation of villous explants in vitro. Hypoxia-reoxygenation activated the p38 and stress-activated protein kinase mitogen-activated protein kinase (MAPK) and the nuclear factor-κB pathways. Downstream consequences included increased tissue concentrations and secretion of tumor necrosis factor-α and interleukin-1β, increased expression of cyclooxygenase-2, and increased apoptosis. Administration of vitamins C and E to explants blocked activation of the p38 and stress-activated protein kinase MAPK and nuclear factor-κB pathways. Vitamin administration or p38 pathway inhibition also reduced cyclooxygenase-2 expression, tumor necrosis factor-α and interleukin-1β secretion, and the levels of apoptosis. We conclude that oxidative stress is a potent inducer of placental synthesis and release of proinflammatory factors. Most of these effects are mediated through the p38 MAPK and nuclear factor-κB pathways and can be effectively blocked by vitamins C and E in vitro.
Preeclampsia is the most important complication of human pregnancy worldwide and a major contributor to maternal and fetal morbidity and mortality. Despite much research, the pathophysiology remains elusive, although there is strong evidence that generation of placental oxidative stress is a key intermediary event.1,2 The stress is thought to induce the placenta to release a cocktail of factors, including proinflammatory cytokines, antiangiogenic factors, and apoptotic debris, which culminates in an enhanced maternal inflammatory response.3 However, the molecular mechanisms linking oxidative stress to release of these factors are not known. In part, this is due to the constraint that placental tissues are only available for study at the end of pregnancy, when the pathology is well established or secondary pathology may have been superimposed.
Early-onset preeclampsia, the most severe form of the syndrome, has its origins in the first trimester of pregnancy.4 During this period, fetal extravillous trophoblast cells migrate into the endometrium, and their presence is associated with the physiological conversion of the maternal spiral arteries into dilated, flaccid conduits that ensure an inviolable blood supply to the conceptus. Trophoblast invasion is impaired in preeclampsia for a number of possible reasons, but the net result is absent, or severely reduced, conversion of the arteries.5 We recently proposed that the retention of smooth muscle within the vessel walls leads to persistence of vasoreactivity and to intermittent perfusion of the intervillous space.4,6 Consequently, the placental tissues are exposed to fluctuating oxygen concentrations and hence suffer repeated ischemia-reperfusion type injuries. In support of this theory, we and others have demonstrated that villi sampled from normal placentas delivered by caesarean section show increased oxidative stress when subjected to hypoxia-reoxygenation (H/R) compared with controls maintained under hypoxia alone.7 These changes closely mimic those reported in preeclampsia and could be attenuated with desferrioxamine, the electron spin trap α-phenyl-N-tert-butylnitrone,4,7 or carbon monoxide.8 Hypoxia-reoxygenation also proved a potent stimulus for apoptotic changes within the syncytiotrophoblast8,9 and induced secretion of tumor necrosis factor (TNF)-α.10 Although these studies established that hypoxia-reoxygenation is a more physiological stimulus than hypoxia alone for generating the placental changes associated with preeclampsia, they did not explore the signaling pathways involved.
Evidence of the involvement of oxidative stress in the pathogenesis of preeclampsia stimulated several clinical trials to test the prophylactic benefits of antioxidant vitamins C and E in women at risk of preeclampsia. Although a beneficial effect of antioxidants was suggested in a small randomized trial of women at high risk of preeclampsia,11 a recent multicenter randomized clinical trial (VIP trial) showed no benefit in prevention of the disease.12 By contrast, we have previously demonstrated that vitamins can prevent hypoxia-reoxygenation-induced secretion of free fetal DNA from villous explants, suggesting that they can limit trophoblast damage in vitro.13 In view of these conflicting in vivo and in vitro findings, we have identified the signaling pathways activated by acute hypoxia-reoxygenation in vitro and tested the effects of antioxidant vitamins C and E on these pathways and the downstream consequences induced.
Materials and Methods
Materials
Antibodies to the phosphorylated and total forms of p38, stress-activated protein kinase (SAPK), IκB, nuclear factor-κB (NF-κB), Hsp27, TNF-α, cleaved caspase-3, and cleaved caspase-9 were from Cell Signaling Technology (Beverly, MA). Anti-cyclooxygenase (COX)-2 was from Cayman Chemical (Ann Arbor, MI). Anti-4-hydroxy-2-nonenal (HNE) antibody was from Axxora (Nottingham, UK) and anti-Hsp90 from Stressgen Bioreagents Corp. (York, UK). The horseradish peroxidase-conjugated secondary antibodies were from Amersham Biosciences (Buckinghamshire, UK). Alexa 488 and Alexa 568 fluorescently labeled antibodies were from Molecular Probes Invitrogen Detection Technologies (Leiden, The Netherlands), and biotinylated secondary antibodies were from Vector Laboratories (Peterborough, UK). The PD169316 inhibitor was from Calbiochem (San Diego, CA); ascorbic acid, SB202190, and Trolox (water-soluble vitamin E) were from Sigma (Poole, UK). Secreted TNF-α was detected by colorimetric enzyme-linked immunosorbent assay using Quantikine kits from R&D Systems (Oxon, UK).
Explant Culture
Placentas (n = 12) were collected from normal-term singleton pregnancies delivered by elective caesarean section with informed written consent of the patients and permission of the Local Research Ethics Committee. Villous samples were taken midway between the chorionic and basal plates from the periphery of lobules free of visible infarction, calcification, hematoma, or tears. After a brief rinse in ice-cold phosphate-buffered saline, samples were placed into ice-cold transport medium (TCS large vessel endothelial cell basal medium; TCS CellWorks, Milton Keynes, UK) containing 2% fetal bovine serum, heparin, hydrocortisone, human epidermal growth factor, human basic fibroblast growth factor, 25 μg/ml gentamicin, and 50 ng/ml amphotericin B, 1 mmol/L vitamin C, and 1 mmol/L Trolox) that had been equilibrated with 5% O2/90% N2/5% CO2.
Following transport to the laboratory on ice, placental samples were further dissected into small pieces (about 5 mm in diameter) in ice-cold culture medium in a glove box under 10% O2/85% N2/5% CO2. Samples were cultured on individual Costar Netwell (24-mm diameter, 500-μm mesh; Corning Life Sciences, Acton, MA) supports in 4 ml of culture medium per well in six-well plates. Approximately 6 to 10 pieces were added to each well, depending on the experimental requirements. Placental explants were incubated in pregassed medium under: 1) normoxic conditions (controls) (10% O2/85% N2/5% CO2) for 7 hours (n = 6) or 16 hours (n = 6), or 2) subjected to hypoxia (0.5% O2/94.5% N2/5% CO2) for 1 hour and subsequent reoxygenation at normoxia (10% O2/85% N2/5% CO2) for the following 6 hours (n = 6) or 15 hours (n = 6) (H/R treatment). All inserts were transferred into previously pregassed medium after 1 hour of incubation. The p38 inhibitor PD169316 was used at a concentration of 10 μmol/L and SB202190 at 30 μmol/L. Vitamin treatment included the addition of 2 mmol/L ascorbic acid and 1 mmol/L Trolox. In all experimental setups, medium was changed in a glove box under a low O2 environment after the first hour of incubation. The p38 inhibitors and vitamins were added at the beginning of each experiment and also when medium was changed.
Western Blotting
Tissue homogenization to obtain protein lysate and subsequent sodium dodecyl sulfate-polyacrylamide gel electrophoresis and immunoblotting were performed as previously described.13 Proteins were revealed and quantified using Image J software (National Institutes of Health, version 1.36b, http://rsb.info.nih.gov/ij/, accessed Sept 2006). Membranes were reprobed with antibody recognizing β-actin to control for protein loading. The values are expressed as a percentage of the control lysate (100%) for each experiment.
Statistical Analysis
All data are presented as means ± SEM. Statistical analysis was performed using StatView (SAS Institute Inc., Cary, NC). Normalized Western blot measurements were analyzed using repeated measures analysis of variance. Differences between two groups were evaluated using a paired Student’s t-test. In all cases, results were considered significant at P < 0.05.
Colorimetric and Fluorescent Immunohistochemistry
Immunohistochemistry with diaminobenzidine detection was performed according to a protocol described recently.13 For immunofluorescent staining, sections were incubated with primary antibodies overnight as in the colorimetric protocol, washed, and incubated for 1 hour at room temperature with species-specific Alexa 488 or Alexa 568 secondary fluorescent antibodies. Sections were washed in Tris-buffered saline and subsequently mounted in Vectashield mounting medium containing 4,6-diamidino-2-phenylindole (Vector Laboratories). Images were captured using a Leica confocal microscope (LeicaTCS-NT; Leica Instruments GmbH, Wetzlar, Germany).
Results
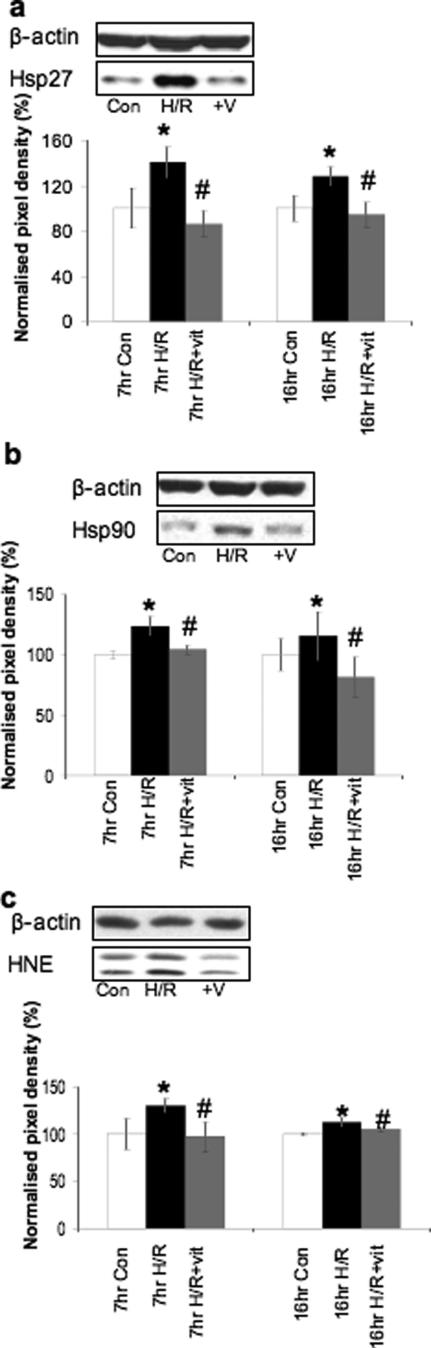
Effect of in Vitro H/R on the Levels of Oxidative Stress
Expression of the heat shock proteins Hsp27 and Hsp90, lipid peroxidation, and the formation of peroxynitrite were used as markers of oxidative stress. H/R strongly increased Hsp27, Hsp90, HNE, and nitrotyrosine concentrations in the explants after 7 and 16 hours of incubation (Figures 1, a–c, and 5, a–c), reflecting an increase of oxidative stress that was localized principally to the syncytiotrophoblast (Figure 5, a–c). The addition of the antioxidant vitamins C and E significantly reduced markers of oxidative stress in H/R-treated samples (Figures 1, a–c, and 5, a–c). All experiments were repeated at least six times.
Figure 1.
In vitro H/R stimulates the expression of oxidative stress markers; simultaneous addition of vitamins suppresses the effects. Protein lysates from placentas cultured under H/R in the presence or absence of vitamins C and E (V) for 7 hours (n = 6) or 16 hours (n = 6) were analyzed for Hsp27 (a), Hsp90 (b), and HNE (c). Representative blots show the 7-hour time point. *P < 0.05 compared with normoxic control; #P < 0.05 compared with H/R treatment.
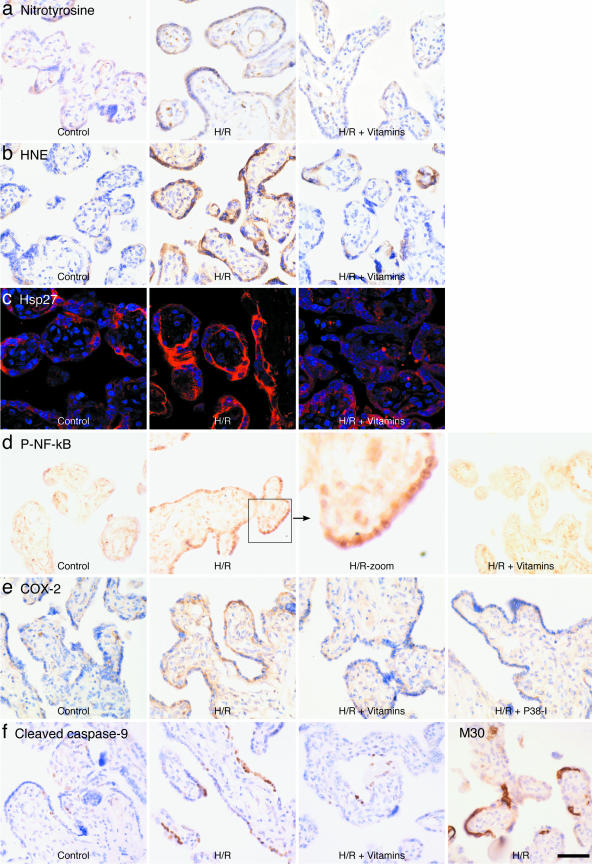
Figure 5.
Immunostaining against nitrotyrosine (a), HNE (b), Hsp27 (c), P-NF-κB (d), COX-2 (e), and cleaved caspase-9 and M30 (f) localized H/R-induced increase in these markers principally to trophoblast. Scale bar = 50 μm.
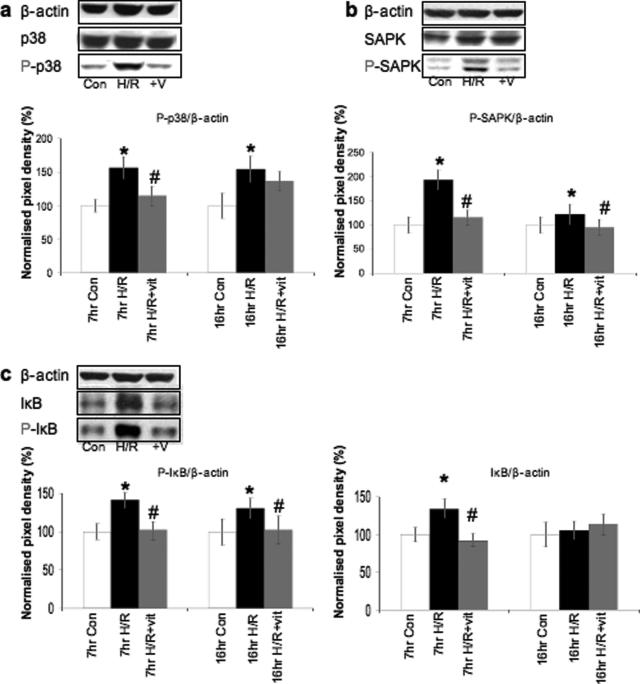
H/R Activates the p38 and SAPK MAPKs and the NF-κB Pathway in Vitro: Effects of Antioxidant Vitamins
H/R stimulated phosphorylation of the p38 and SAPK MAPK pathways after 7 and 16 hours of incubation, whereas total p38 and SAPK levels remained unchanged (Figure 2, a and b). The addition of vitamins suppressed phosphorylation of p38 at 7 hours and that of SAPK stress kinase at both time points (Figure 2, a and b). The p38 pathway has been implicated in the production of proinflammatory cytokines, suggesting a possible role in the regulation of NF-κB activity. Phosphorylation and subsequent degradation of the IκB protein allows NF-κB translocation to the nucleus, where it regulates gene expression. Hence, the phosphorylation status of IκB serves to determine activation of this pathway. H/R greatly elevated phosphorylation of IκB at 7 and 16 hours of incubation (Figure 2c). Total IκB expression was increased in H/R-treated samples after 7 hours of incubation but returned to basal level at 16 hours, reflecting IκB degradation. The addition of vitamins significantly suppressed phosphorylation of IκB by H/R (Figure 2c). Immunohistochemistry demonstrated nuclear translocation of phospho-NF-κB to syncytial nuclei, indicative of activation and involvement in the regulation of gene expression (Figure 5d).
Figure 2.
In vitro H/R activates p38 MAPK, SAPK, and NF-κB pathways; simultaneous addition of vitamins or a p38 inhibitor suppresses the effects of H/R. Protein lysates from placentas cultured under H/R in the presence or absence of vitamins C and E (V) or PD169316 (P-I) for 7 hours (n = 6) or 16 hours (n = 6) were analyzed for P-p38, p38 (a); P-SAPK, SAPK (b); and P-IκB, IκB (c). Representative blots show the 7-hour time point. *P < 0.05 compared with normoxic control; #P < 0.05 compared with H/R treatment.
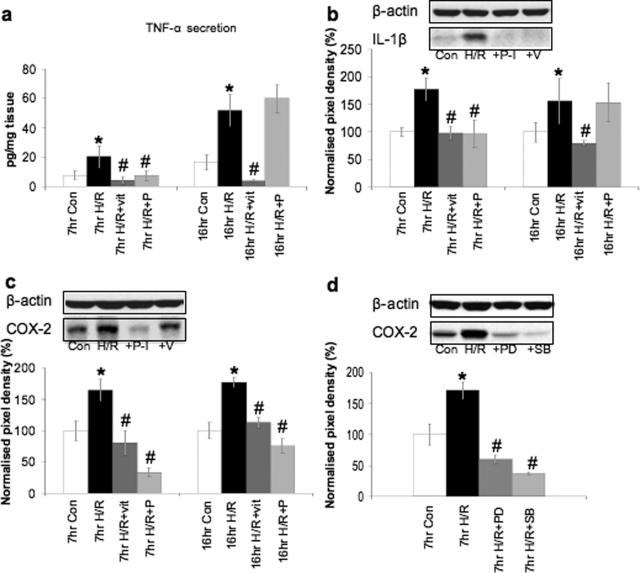
In Vitro H/R-Induced Stimulation of Proinflammatory Cytokines, COX-2, and Apoptosis Can Be Suppressed by Antioxidant Vitamins or p38 Inhibition
NF-κB exerts its effects by regulating genes encoding cytokines, chemokines, adhesion molecules, growth factors, and inducible proinflammatory enzymes such as COX-2. Therefore, the tissue expression of COX-2 and the levels of TNF-α and interleukin (IL)-1β were examined. Vitamins blocked the NF-κB pathway, and their effect on these downstream pathways was thus of interest. The p38 MAPK pathway has also been shown to regulate inflammatory cytokines and COX-2.14,15 To test involvement of this pathway, we used the p38 inhibitors PD169316 and SB202190 in conjunction with H/R. Application of both inhibitors yielded very similar results (Figure 3d), and for simplicity, only data from experiments using PD169316 are shown here.
Figure 3.
In vitro H/R activates the tissue production and secretion of inflammatory cytokines and COX-2; the addition of vitamins or the p38 inhibitor suppresses the effects of H/R. a: Supernatants from placentas cultured under H/R in the presence or absence of vitamins C and E (V) or PD169316 (P-I) for 7 hours (n = 6) or 16 hours (n = 6) were analyzed by enzyme-linked immunosorbent assay for the secretion of TNF-α. Data were normalized against wet tissue weights. Corresponding protein lysates were analyzed with IL-1β (b) and COX-2 (c, d). d: Effect of the two p38 inhibitors, PD169316 (PD) and SB202190 (SB), was comparable. Representative blots show the 7-hour time point. *P < 0.05 compared with normoxic controls; #P < 0.05 compared with H/R.
Secretion of TNF-α from the explants into the supernatant was measured at 7 and 16 hours by enzyme-linked immunosorbent assay. H/R caused a significant increase in TNF-α secretion, which increased with time (Figure 3a). The addition of vitamins powerfully suppressed this effect at both time points. The p38 inhibitor suppressed TNF-α secretion at 7 hours but had no effect at 16 hours (Figure 3a). Tissue production of IL-1β (Figure 3b) and TNF-α (data not shown) was also stimulated by H/R. The addition of vitamins prevented the H/R stimulation of IL-1β after 7- and 16-hour incubation. PD169316 only reduced tissue concentrations of IL-1β at 7 hours and had no effect at 16 hours (Figure 3b). Secretion of IL-1β was not measured. H/R-induced tissue production of TNF-α increased in a similar manner as that of IL-1β (not shown). H/R also stimulated a significant increase in COX-2 protein concentrations at both time points compared with normoxic controls, and this was localized mainly to the trophoblast (Figures 3c and 5e). Again, this increase was suppressed by vitamins and p38 kinase inhibitors at 7 and 16 hours (Figures 3, c and d, and 5e).
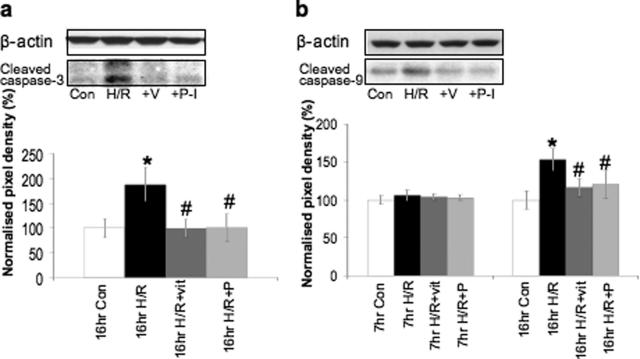
H/R stimulated the activation of molecules required for apoptosis in the placental explants as seen by an increase in the concentrations of cleaved caspase-3 (Figure 4a) and cleaved caspase-9 at 16 hours (cleavage of caspase-3 was undetectable at 7 hours) (Figure 4b). During apoptosis cytokeratins within trophoblast cells are cleaved by active caspase-3 to yield a specific product detected by the M30 antibody.16 M30 staining confirmed an increase in trophoblast apoptosis following H/R (Figure 5f). Crucially, both PD169316 and vitamins C and E significantly reduced cleavage of both caspases to control levels in placental explants subjected to H/R and reduced the incidence of M30 staining (Figures 4, a–b, and 5f).
Figure 4.
In vitro H/R stimulates apoptosis; the addition of vitamins or the p38 inhibitor suppress the effects of H/R. Protein lysates from placentas cultured under H/R in the presence or absence of vitamins C and E (V) or PD169316 (P-I) for 7 hours (n = 6) or 16 hours (n = 6) were analyzed for cleaved caspase-3 (undetectable at 7 hours) (a) and cleaved caspase-9 (b). Representative blots show the 16-hour time point. *P < 0.05 compared with normoxic control; #P < 0.05 compared with H/R treatment.
Discussion
The aim was to investigate the acute effects of oxidative stress on the human placenta to understand the pathophysiology of the placental changes that underlie preeclampsia. We have demonstrated that placental explants challenged with hypoxia-reoxygenation in vitro show a marked increase in the levels of oxidative stress and activation of the p38 and SAPK MAPK and the NF-κB pathways. The addition of the antioxidant vitamins C and E effectively suppressed concentrations of markers of oxidative stress, levels of apoptosis, and secretion of TNF-α and IL-1β induced by H/R at 7 and 16 hours. They also suppressed the levels of COX-2 and inhibited the phosphorylation of p38, SAPK, and IκB. A p38 inhibitor was used to evaluate the effect of the p38 pathway on the downstream effects of H/R. Inhibition of p38 effectively suppressed H/R-induced COX-2 expression at 7 and 16 hours and the level of apoptosis-associated markers at 16 hours. However, it only suppressed TNF-α and IL-1β expression and secretion at 7 hours and had no effect after 16 hours of culture. We used the pharmacological inhibitor of p38, PD169316, to address these questions. Similar results were obtained using a second pharmacological inhibitor of p38 signaling, SB202190. Both pharmacological agents are frequently used to block the p38 pathway. However, it should be noted that the specificity of the two p38 kinase inhibitors, PD169316 and SB202190, is questionable as they can also inhibit JNK/SAPK and may also inhibit other upstream kinases.17 We are aware of these difficulties, and we used both inhibitors at the lowest possible doses. However, we cannot exclude nonspecific effects of these inhibitors. We performed parallel experiments, in which explants were challenged with 1 mmol/L hydrogen peroxide (H2O2) under normoxic conditions for 7 or 16 hours. Remarkably, H/R and H2O2 treatments resulted in the same changes listed above, and the addition of vitamins was just as effective in suppressing H2O2-induced effects. For simplicity, only H/R effects are presented in this article.
The addition of vitamins to H/R-treated samples suppressed most effects of H/R in vitro. Vitamins C and E act in concert to scavenge reactive oxygen species, with vitamin C being required to recycle vitamin E. In agreement with our results, vitamin C has been reported to suppress TNF-α-induced nuclear translocation of NF-κB, NF-κB-dependent reporter transcription, and IκBα phosphorylation in human cell lines and primary endothelial cells.18 In another study, the addition of vitamins C and E inhibited intracellular reactive oxygen species production and activation of the NF-κB, PKR, eIF-2α, protein kinase C, and p38 MAPK pathways.19 Intracellular vitamin C has been shown to protect human umbilical vein endothelial cells from H/R-induced apoptosis, preventing loss of mitochondrial membrane potential, the release of cytochrome c, and activation of caspase-9 and caspase-3 during H/R.20 It would thus seem that the beneficial effects of vitamins in our system are mediated through inhibition of NF-κB by vitamin C.
Vitamin E is known to inhibit the p38 MAPK pathway in smooth muscle cells and to prevent activation of NADPH oxidase in monocyte mitochondria, resulting in lower levels of intracellular reactive oxygen species.21 α-Tocopherol also inhibits protein kinase C activation necessary for smooth muscle cell activation22,23 and prevents human platelet aggregation via a protein kinase C-dependent mechanism.24 In addition, vitamin E down-regulates the expression of intercellular cell adhesion molecule-1 and vascular cell adhesion molecule-1 in endothelial cells,25 and inhibits cyclooxygenase activity in macrophages from aged mice by reducing peroxynitrite production.26,27 These effects of vitamin E, namely p38 and COX-2 inhibition and reduced peroxynitrite formation, are in agreement with the findings of our study.
Inhibitors of the p38 pathway (PD169316 and SB202190) were equally effective in suppressing apoptosis and COX-2 expression and to some degree that of the proinflammatory cytokines. The p38 pathway has been implicated in the posttranscriptional regulation of TNF-α, IL-1, and COX-2 mRNAs.14,15 In our study, placental explants subjected to oxidative stress showed increased secretion or tissue levels of TNF-α and IL-1β. The function of these cytokines in normal pregnancy and delivery is not fully established. TNF-α, IL-1, and IL-6 have been detected in human amniotic fluid during pregnancy and labor28,29 and in preterm labor in the presence of chorioamnionitis.30 These cytokines activate the prostaglandin biosynthetic pathway primarily via induction of COX-2. Investigations in a number of cell types have demonstrated that IL-1β-induced COX-2 expression involves activation of members of the NF-κB family of transcription factors and the SAPK, ERK1/2, and p38 MAPK cascades.31,32,33 There is therefore the possibility of developing an autocrine feed-forward system. In human amnion cells harvested after labor, there is an increased constitutive activity of NF-κB, which functions to increase the COX-2 expression and seems to contribute to the “functional” progesterone withdrawal through an interaction with the progesterone receptor.34 Inhibition of the p38 MAPK pathway significantly suppressed H/R-induced COX-2 expression at 7 and 16 hours, but it only suppressed TNF-α and IL-1β secretion at 7 hours and had no effect at 16 hours, suggesting that inflammatory cytokine regulation is not dependent on p38 signaling alone or that the inhibitors were overwhelmed in the longer cultures. Vitamin treatment significantly reduced NF-κB activation, and that was associated with significantly reduced levels of COX-2 and inflammatory cytokines at 7 and 16 hours. These results confirm that both p38 and NF-κB pathways are involved in stimulating COX-2 expression and TNF-α and IL-1β secretion. They also raise the possibility that placental oxidative stress may play a role in initiating or augmenting uterine contractions during labor. Our findings may be applicable to other cell types, particularly decidual and placental macrophages that also contribute to the production of inflammatory cytokines and may play a role in mediating labor contractions.35,36,37
Although a beneficial effect of antioxidants was suggested in a small randomized trial where women at risk of preeclampsia were supplemented with vitamins C and E,11 a recent multicenter randomized clinical trial (VIP trial) showed no benefit in prevention of the disease.12 The reasons for the disparity between our results and the in vivo data are not clear but may reflect differences in cellular concentrations or accessibility of the vitamins. Questions also arise as to whether supplementing with vitamins from 14 to 20 weeks is early enough in pregnancy to prevent the onset of the disease. It has been shown that oral dosing with vitamin C (200 mg/day) maintains a plasma concentration between 10 and 160 μmol/L.38 However, intracellular concentrations of ascorbic acid can range between 1.4 and 3.4 mmol/L,39 and so we used vitamin C concentrations of 1 to 2 mmol/L in our study. Vitamin C (2 mmol/L) was found to be the most effective in reducing the effects of H/R. Plasma concentrations of vitamins C in the VIP trial were around 100 to 130 μmol/L in the supplemented group, which are considerably lower, but the intracellular concentrations achieved in placental tissues are not known. The daily doses of vitamins C and E used in the trial were below the maximum daily tolerable intake recommended by the Institute of Medicine of the United States,40 although it should be noted that the UK population studied already consumed considerable amounts of supplements in their diet. Consequently, additional intake may not have had much effect. This possibility could be addressed soon by two ongoing trials involving supplementation with antioxidant vitamins in developing nations where dietary deficiency is more likely (a multicenter World Health Organization trial and a trial in Brazil).
In the VIP trial, α-tocopherol was used as a vitamin E supplement. Vitamin E consists of four tocopherol homologues, and among them only α-tocopherol has been used in clinical studies.41 Recent evidence demonstrated that γ-tocopherol has several specific pharmacological properties such as anti-inflammatory and antiproliferative effects in addition to its antioxidative effects.42,43 γ-Tocopherol, but not α-tocopherol, reduces the neointima proliferation in insulin resistance independently of its effects on superoxide production.44 The metabolic differences between different tocopherols may therefore need to be considered when studying the in vivo effects of vitamin E.
A recent Australian trial also found no benefits of vitamin C and E supplementation in the prevention of preeclampsia.45 This trial was conducted on healthy nulliparous women who had a low risk of preeclampsia. The VIP trial focused on high-risk patients who are more likely to develop preeclampsia. As a consequence, the study population was very heterogeneous, including women with chronic hypertension, diabetes, renal disease, previous preeclampsia, obesity, antiphospholipid syndrome, and multiple pregnancies. Preventative intervention could thus have a varying effect on the different subgroups involved. The study group in the previous successful small trial11 was notably more homogeneous, with women being recruited on the basis of abnormal two-stage uterine artery Doppler screening, which has a high predictive value for preeclampsia.46 More trials are currently in progress in the United States, Canada, Mexico, and Brazil.47,48
An analogous situation has been reported in the field of cardiovascular pathology. Strong evidence exists that oxidative stress is pivotally involved in the pathogenesis of atherosclerosis. Many in vitro, cellular, and animal studies show convincing evidence of the protective effects of vitamin E against a variety of types of oxidative stress.49 α-Tocopherol has been shown to reduce atherosclerotic lesions,50 smooth muscle cell proliferation,51 and platelet adherence and aggregation52 in animal models. It can also improve endothelial function in humans.53 Several cohort studies suggested reduced cardiovascular risk in persons taking vitamin E supplements.54,55,56 However, these initial hopeful reports were followed by the negative results of almost all large randomized trials that failed to confirm a role for vitamin E supplementation in cardiovascular prevention.41 The most recent trial additionally showed that not only does long-term vitamin E supplementation fail to prevent cancer or major cardiovascular complications, it may increase the risk for heart failure.57
Several important conclusions can be drawn on the basis of our findings. First, the acute stress of hypoxia-reoxygenation in vitro leads to the same placental changes that characterize what has previously been considered the more chronic stress of preeclampsia. These findings provide support for our hypothesis that intermittent perfusion of the placenta, secondary to reduced trophoblast invasion, initiates the placental changes that stimulate preeclampsia. Second, we were able to prevent the changes in vitro using the antioxidant vitamins C and E and to some extent by blocking the p38 MAPK pathway. Our findings suggest that devising strategies to minimize placental oxidative stress is still a worthwhile target in the prevention of preeclampsia.
Acknowledgments
We are grateful to the staff of the Delivery Unit, Rosie Hospital, Cambridge, for their help in obtaining the placental samples.
Footnotes
Address reprint requests to Professor Graham J. Burton, Department of Physiology, Development and Neuroscience, Downing Street, Cambridge CB2 3EG, UK. E-mail: gjb2@cam.ac.uk.
Supported by Wellcome Trust grant 069027/Z/02/Z.
D.S.C.-J. and G.J.B. contributed equally to this work.
References
- Roberts JM, Hubel CA. Is oxidative stress the link in the two-stage model of pre-eclampsia? Lancet. 1999;354:788–789. doi: 10.1016/S0140-6736(99)80002-6. [DOI] [PubMed] [Google Scholar]
- Redman CW, Sargent IL. Latest advances in understanding preeclampsia. Science. 2005;308:1592–1594. doi: 10.1126/science.1111726. [DOI] [PubMed] [Google Scholar]
- Roberts JM. Endothelial dysfunction in preeclampsia. Semin Reprod Endocrinol. 1998;16:5–15. doi: 10.1055/s-2007-1016248. [DOI] [PubMed] [Google Scholar]
- Burton GJ, Hung T-H. Hypoxia-reoxygenation: a potential source of placental oxidative stress in normal pregnancy and preeclampsia. Fetal Maternal Med Rev. 2003;14:97–117. [Google Scholar]
- Brosens JJ, Pijnenborg R, Brosens IA. The myometrial junctional zone spiral arteries in normal and abnormal pregnancies: a review of the literature. Am J Obstet Gynecol. 2002;187:1416–1423. doi: 10.1067/mob.2002.127305. [DOI] [PubMed] [Google Scholar]
- Burton GJ, Jauniaux E. Placental oxidative stress: from miscarriage to preeclampsia. J Soc Gynecol Investig. 2004;11:342–352. doi: 10.1016/j.jsgi.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Hung T-H, Skepper JN, Burton GJ. In vitro ischemia-reperfusion injury in term human placenta as a model for oxidative stress in pathological pregnancies. Am J Pathol. 2001;159:1031–1043. doi: 10.1016/S0002-9440(10)61778-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bainbridge SA, Belkacemi L, Dickinson M, Graham CH, Smith GN. Carbon monoxide inhibits hypoxia/reoxygenation-induced apoptosis and secondary necrosis in syncytiotrophoblast. Am J Pathol. 2006;169:774–783. doi: 10.2353/ajpath.2006.060184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung T-H, Skepper JN, Charnock-Jones DS, Burton GJ. Hypoxia-reoxygenation: a potent inducer of apoptotic changes in the human placenta and possible etiological factor in preeclampsia. Circ Res. 2002;28:1274–1281. doi: 10.1161/01.res.0000024411.22110.aa. [DOI] [PubMed] [Google Scholar]
- Hung T-H, Charnock-Jones DS, Skepper JN, Burton GJ. Secretion of tumor necrosis factor-alpha from human placental tissues induced by hypoxia-reoxygenation causes endothelial cell activation in vitro: a potent mediator of the inflammatory response in preeclampsia. Am J Pathol. 2004;164:1049–1061. doi: 10.1016/s0002-9440(10)63192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chappell LC, Seed PT, Briley AL, Kelly FJ, Lee R, Hunt BJ, Parmar K, Bewley SJ, Shennan AH, Steer PJ, Poston L. Effect of antioxidants on the occurrence of pre-eclampsia in women at increased risk: a randomised trial. Lancet. 1999;354:810–816. doi: 10.1016/S0140-6736(99)80010-5. [DOI] [PubMed] [Google Scholar]
- Poston L, Briley AL, Seed PT, Kelly FJ, Shennan AH. Vitamin C and vitamin E in pregnant women at risk for pre-eclampsia (VIP trial): randomised placebo-controlled trial. Lancet. 2006;367:1145–1154. doi: 10.1016/S0140-6736(06)68433-X. [DOI] [PubMed] [Google Scholar]
- Tjoa M-L, Cindrova-Davies T, Spasic-Boskovic O, Bianchi DW, Burton GJ. Trophoblastic oxidative stress and the release of cell-free feto-placental DNA. Am J Pathol. 2006;169:400–404. doi: 10.2353/ajpath.2006.060161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S, Boehm J, Lee JC. p38 MAP kinases: key signalling molecules as therapeutic targets for inflammatory diseases. Nat Rev Drug Discov. 2003;2:717–726. doi: 10.1038/nrd1177. [DOI] [PubMed] [Google Scholar]
- Lee JC, Laydon JT, McDonnell PC, Gallagher TF, Kumar S, Green D, McNulty D, Blumenthal MJ, Heys JR, Landvatter SW, Strickler JE, McLaughlin MM, Siemens IR, Fisher SM, Livi GP, White JR, Adams JL, Young PR. A protein kinase involved in the regulation of inflammatory cytokine biosynthesis. Nature. 1994;372:739–746. doi: 10.1038/372739a0. [DOI] [PubMed] [Google Scholar]
- Kadyrov M, Kaufmann P, Huppertz B. Expression of a cytokeratin 18 neo-epitope is a specific marker for trophoblast apoptosis in human placenta. Placenta. 2001;22:44–48. doi: 10.1053/plac.2000.0616. [DOI] [PubMed] [Google Scholar]
- Schlezinger JJ, Emberley JK, Sherr DH. Activation of multiple mitogen-activated protein kinases in pro/pre-B cells by GW7845, a peroxisome proliferator-activated receptor gamma agonist, and their contribution to GW7845-induced apoptosis. Toxicol Sci. 2006;92:433–444. doi: 10.1093/toxsci/kfl003. [DOI] [PubMed] [Google Scholar]
- Cárcamo J, Pedraza A, Borquez-Ojeda O, Golde D. Vitamin C suppresses TNF-α-induced NF-κB activation by inhibiting IκBα phosphorylation. Biochemistry. 2002;41:12995–13002. doi: 10.1021/bi0263210. [DOI] [PubMed] [Google Scholar]
- Tan PH, Sagoo P, Chan C, Yates JB, Campbell J, Beutelspacher SC, Foxwell BMJ, Lombardi G, George AJT. Inhibition of NF-κB and oxidative pathways in human dendritic cells by antioxidative vitamins generates regulatory T cells. J Immunol. 2005;174:7633–7644. doi: 10.4049/jimmunol.174.12.7633. [DOI] [PubMed] [Google Scholar]
- Dhar-Mascareño M, Carcamo JM, Golde DW. Hypoxia-reoxygenation-induced mitochondrial damage and apoptosis in human endothelial cells are inhibited by vitamin C. Free Radic Biol Med. 2005;38:1311–1322. doi: 10.1016/j.freeradbiomed.2005.01.017. [DOI] [PubMed] [Google Scholar]
- Cachia O, Benna JE, Pedruzzi E, Descomps E, Gougerot-Pocidalo MA, Leger CL. α-Tocopherol inhibits the respiratory burst in human monocytes: attenuation of p47phox membrane translocation and phosphorylation. J Biol Chem. 1998;273:32801–32805. doi: 10.1074/jbc.273.49.32801. [DOI] [PubMed] [Google Scholar]
- Boscoboinik D, Szewczyk A, Azzi A. Alpha-tocopherol (vitamin E) regulates vascular smooth muscle cell proliferation and protein kinase C activity. Arch Biochem Biophys. 1991;286:264–269. doi: 10.1016/0003-9861(91)90039-l. [DOI] [PubMed] [Google Scholar]
- Boscoboinik D, Szewczyk A, Hensey C, Azzi A. Inhibition of cell proliferation by alpha-tocopherol: role of protein kinase C. J Biol Chem. 1991;266:6188–6194. [PubMed] [Google Scholar]
- Freedman JE, Farhat JH, Loscalzo J, Keaney JF., Jr Alpha-tocopherol inhibits aggregation of human platelets by a protein kinase C-dependent mechanism. Circulation. 1996;94:2434–2440. doi: 10.1161/01.cir.94.10.2434. [DOI] [PubMed] [Google Scholar]
- Cominacini L, Garbin U, Pasini AF, Davoli A, Campagnola M, Contessi GB, Pastorino AM, Lo Cascio V. Antioxidants inhibit the expression of intercellular cell adhesion molecule-1 and vascular cell adhesion molecule-1 induced by oxidized LDL on human umbilical vein endothelial cells. Free Radic Biol Med. 1997;22:117–127. doi: 10.1016/s0891-5849(96)00271-7. [DOI] [PubMed] [Google Scholar]
- Beharka AA, Wu D, Serafini M, Meydani SN. Mechanism of vitamin E inhibition of cyclooxygenase activity in macrophages from old mice: role of peroxynitrite. Free Radic Biol Med. 2002;32:503–511. doi: 10.1016/s0891-5849(01)00817-6. [DOI] [PubMed] [Google Scholar]
- Wu D, Hayek MG, Meydani S. Vitamin E and macrophage cyclooxygenase regulation in the aged. J Nutr. 2001;131:382S–388S. doi: 10.1093/jn/131.2.382S. [DOI] [PubMed] [Google Scholar]
- Santhanam U, Avila C, Romero R, Viguet H, Ida N, Sakurai S, Sehgal PB. Cytokines in normal and abnormal parturition: elevated amniotic fluid interleukin-6 levels in women with premature rupture of membranes associated with intrauterine infection. Cytokine. 1991;3:155–163. doi: 10.1016/1043-4666(91)90037-e. [DOI] [PubMed] [Google Scholar]
- Romero R, Mazor M, Sepulveda W, Avila C, Copeland D, Williams J. Tumor necrosis factor in preterm and term labor. Am J Obstet Gynecol. 1992;166:1576–1587. doi: 10.1016/0002-9378(92)91636-o. [DOI] [PubMed] [Google Scholar]
- Romero R, Brody DT, Oyarzun E, Mazor M, Wu YK, Hobbins JC, Durum SK. Infection and labor. III. Interleukin-1: a signal for the onset of parturition. Am J Obstet Gynecol. 1989;160:1117–1123. doi: 10.1016/0002-9378(89)90172-5. [DOI] [PubMed] [Google Scholar]
- Newton R, Kuitert LME, Bergmann M, Adcock IM, Barnes PJ. Evidence for involvement of NF-κB in the transcription control of COX-2 gene expression by IL-1β. Biochem Biophys Res Commun. 1997;237:28–32. doi: 10.1006/bbrc.1997.7064. [DOI] [PubMed] [Google Scholar]
- Guan ZH, Buckman SY, Miller BW, Springer LD, Morrison AR. Interleukin-1 beta-induced cyclooxygenase-2 expression requires activation of both c-jun NH2-terminal kinase and p38 MAPK signal pathways in rat renal mesangial cells. J Biol Chem. 1998;273:28670–28676. doi: 10.1074/jbc.273.44.28670. [DOI] [PubMed] [Google Scholar]
- LaPointe MC, Isenovic E. Interleukin-1β regulation of inducible nitric oxide synthase and cyclooxygenase-2 involves the p42/44 and p38 MAPK signalling pathways in cardiac myocytes. Hypertension. 1999;33:276–282. doi: 10.1161/01.hyp.33.1.276. [DOI] [PubMed] [Google Scholar]
- Allport VC, Pieber D, Slater DM, Newton R, White JO, Bennett PR. Human labour is associated with nuclear factor-κB activity which mediates cyclo-oxygenase-2 expression and is involved with the “functional progesterone withdrawal.”. Mol Hum Reprod. 2001;7:581–586. doi: 10.1093/molehr/7.6.581. [DOI] [PubMed] [Google Scholar]
- Mackler AM, Iezza G, Akin MR, McMillan P, Yellon SM. Macrophage trafficking in the uterus and cervix precedes parturition in the mouse. Biol Reprod. 1999;61:879–883. doi: 10.1095/biolreprod61.4.879. [DOI] [PubMed] [Google Scholar]
- Kim JS, Romero R, Cushenberry E, Kim YM, Erez O, Nien JK, Yoon BH, Espinoza J, Kim CJ: Distribution of CD14+ and CD68+ macrophages in the placental bed and basal plate of women with preeclampsia and preterm labor. Placenta 2006 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Lyall F. Priming and remodelling of human placental bed spiral arteries during pregnancy: a review. Placenta. 2005;26(Suppl A):S31–S36. doi: 10.1016/j.placenta.2005.02.010. [DOI] [PubMed] [Google Scholar]
- Hediger MA. New view at C. Nat Med. 2002;8:445–446. doi: 10.1038/nm0502-445. [DOI] [PubMed] [Google Scholar]
- Levine M, Wang Y, Padayatty SJ, Morrow J. A new recommended dietary allowance of vitamin C for healthy young women. Proc Natl Acad Sci USA. 2001;98:9842–9846. doi: 10.1073/pnas.171318198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine Dietary reference intakes for vitamin C, E, selenium and carotenoids. Washington DC: National Academy Press,; The Panel on Dietary Antioxidants and Related Compounds. 2006 [Google Scholar]
- Vivekananthan DP, Penn MS, Sapp SK, Hsu A, Topol EJ. Use of antioxidant vitamins for the prevention of cardiovascular disease: meta-analysis of randomised trials. Lancet. 2003;361:2017–2023. doi: 10.1016/S0140-6736(03)13637-9. [DOI] [PubMed] [Google Scholar]
- Jiang Q, Elson-Schwab I, Courtemanche C, Ames BN. Gamma-tocopherol and its major metabolite, in contrast to alpha-tocopherol, inhibit cyclooxygenase activity in macrophages and epithelial cells. Proc Natl Acad Sci USA. 2000;97:11494–11499. doi: 10.1073/pnas.200357097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gysin R, Azzi A, Visarius T. Gamma-tocopherol inhibits human cancer cell cycle progression and cell proliferation by down-regulation of cyclins. FASEB J. 2002;16:1952–1954. doi: 10.1096/fj.02-0362fje. [DOI] [PubMed] [Google Scholar]
- Takahashi K, Komaru T, Takeda S, Takeda M, Koshida R, Nakayama M, Kokusho Y, Kawakami Y, Yamaguchi N, Miyazawa T, Shimokawa H, Shirato K. Gamma-tocopherol, but not alpha-tocopherol, potently inhibits neointimal formation induced by vascular injury in insulin resistant rats. J Mol Cell Cardiol. 2006;41:544–554. doi: 10.1016/j.yjmcc.2006.06.010. [DOI] [PubMed] [Google Scholar]
- Rumbold AR, Crowther CA, Haslam RR, Dekker GA, Robinson JS. Vitamins C and E and the risks of preeclampsia and perinatal complications. N Engl J Med. 2006;354:1796–1806. doi: 10.1056/NEJMoa054186. [DOI] [PubMed] [Google Scholar]
- Carbillon L. Vitamin C and vitamin E in pregnant women at risk of pre-eclampsia. Lancet. 2006;368:198–200. doi: 10.1016/S0140-6736(06)69030-2. [DOI] [PubMed] [Google Scholar]
- Romero R, Garite TJ. Unexpected results of an important trial of vitamins C and E administration to prevent preeclampsia. Am J Obstet Gynecol. 2006;194:1213–1214. doi: 10.1016/j.ajog.2006.04.007. [DOI] [PubMed] [Google Scholar]
- Fraser WD, Audibert F, Bujold E, Leduc L, Xu H, Boulvain M, Julien P. The vitamin E debate: implications for ongoing trials of pre-eclampsia prevention. BJOG. 2005;112:684–688. doi: 10.1111/j.1471-0528.2005.00675.x. [DOI] [PubMed] [Google Scholar]
- Pryor WA. Vitamin E and heart disease: basic science to clinical intervention trials. Free Radic Biol Med. 2000;28:141–164. doi: 10.1016/s0891-5849(99)00224-5. [DOI] [PubMed] [Google Scholar]
- Verlangieri AJ, Bush MJ. Effects of d-alpha-tocopherol supplementation on experimentally induced primate atherosclerosis. J Am Coll Nutr. 1992;11:131–138. [PubMed] [Google Scholar]
- Meydani M. Vitamin E. Lancet. 1995;345:170–175. doi: 10.1016/s0140-6736(95)90172-8. [DOI] [PubMed] [Google Scholar]
- Steiner M. Influence of vitamin E on platelet function in humans. J Am Coll Nutr. 1991;10:466–473. doi: 10.1080/07315724.1991.10718173. [DOI] [PubMed] [Google Scholar]
- Skyrme-Jones RA, O’Brien RC, Berry KL, Meredith IT. Vitamin E supplementation improves endothelial function in type I diabetes mellitus: a randomized, placebo-controlled study. J Am Coll Cardiol. 2000;36:94–102. doi: 10.1016/s0735-1097(00)00720-8. [DOI] [PubMed] [Google Scholar]
- Stephens NG, Parsons A, Schofield PM, Kelly F, Cheeseman K, Mitchinson MJ. Randomised controlled trial of vitamin E in patients with coronary disease: Cambridge Heart Antioxidant Study (CHAOS). Lancet. 1996;347:781–786. doi: 10.1016/s0140-6736(96)90866-1. [DOI] [PubMed] [Google Scholar]
- Motoyama T, Kawano H, Kugiyama K, Hirashima O, Ohgushi M, Tsunoda R, Moriyama Y, Miyao Y, Yoshimura M, Ogawa H, Yasue H. Vitamin E administration improves impairment of endothelium-dependent vasodilation in patients with coronary spastic angina. J Am Coll Cardiol. 1998;32:1672–1679. doi: 10.1016/s0735-1097(98)00447-1. [DOI] [PubMed] [Google Scholar]
- Steiner M, Glantz M, Lekos A. Vitamin E plus aspirin compared with aspirin alone in patients with transient ischemic attacks. Am J Clin Nutr. 1995;62:1381S–1384S. doi: 10.1093/ajcn/62.6.1381S. [DOI] [PubMed] [Google Scholar]
- Lonn E, Bosch J, Yusuf S, Sheridan P, Pogue J, Arnold JM, Ross C, Arnold A, Sleight P, Probstfield J, Dagenais GR. Effects of long-term vitamin E supplementation on cardiovascular events and cancer: a randomized controlled trial. JAMA. 2005;293:1338–1347. doi: 10.1001/jama.293.11.1338. [DOI] [PubMed] [Google Scholar]