Abstract
Objectives. We describe electronic health data use by the Department of Veterans Affairs (VA) in the month after Katrina, including supporting technologies, the extent and nature of information accessed, and lessons learned.
Methods. We conducted a retrospective study using cross-sectional panels of data collected sequentially over time.
Results. By September 30, 2005, clinical data were accessed electronically for at least 38% (14941 of 39910) of patients cared for prior to Hurricane Katrina by New Orleans–area VA medical facilities. Approximately 1000 patients per day had data accessed during the month following Hurricane Katrina, a rate approximately two thirds of pre-Katrina values. Health care data were transmitted to more than 200 sites in 48 states and to at least 2300 users.
Conclusions. The VA electronic health records supported continuity of care for evacuated veterans after Katrina. Our findings suggest that pharmacy and laboratory computerization alone will not be sufficient for future disaster support systems.
Earlier studies document many benefits of electronic health records, including improved access, formatting, legibility, and organization of patient data for direct care, administration, and research. Electronic health records also assist with timely decision making, improved communication and care coordination, cost control, public health surveillance, population health planning, and clerical task reduction.1–8 One benefit is absent from this lengthy list: health care support during disasters. In this article, we review the use of the Department of Veterans Affairs (VA) electronic health record system in support of evacuee health care in the wake of Hurricane Katrina’s devastation of the city of New Orleans, La.
Metropolitan New Orleans had a population of 1 319589 as of July 1, 2004. Before Hurricane Katrina, the New Orleans VA Medical Center provided care to 39910 veterans, including 2123 who received care primarily at the affiliated outpatient clinics in Baton Rouge and Houma. On average, 1717 patients per weekday were cared for at these 3 facilities between May and July 2005. The New Orleans VA Medical Center is aligned with other VA medical centers in Louisiana, Mississippi, Arkansas, Oklahoma, and Texas in the region known as Veterans Integrated Service Network 16 (VISN 16).
All of the VA medical facilities are extensively computerized, with a long history of using information technology. By 1981, VA developers built a prototype hospital information system using a common database system and common data dictionary9–11 that provided extensive clinical12–21 and administrative22 functionality. The prototype evolved into a suite of applications known as the Decentralized Hospital Computer Program, which was implemented at 169 sites nationwide by 1985.23,24
In 1996, the Decentralized Hospital Computer Program was renamed Veterans Health Information Systems and Technology Architecture (VistA), and the Computerized Patient Record System (CPRS) application was released.25,26 Installation and use of CPRS, which includes provider order entry27–29 and provider-entered electronic progress notes, was mandated in 1999. In 1999 and 2000, the VA implemented bar code medication administration, giving nurses handheld scanners and a bedside computerized medication administration record.30 Because veterans often seek care at several VA sites, VistA developed remote data views to help providers locate and review records stored anywhere in the country. The VA’s organizational culture is to accept and routinely use electronic health records, and today the VA’s leadership in this area is recognized in both the indexed literature31–34 and the lay press.35,36
KATRINA AND THE EVACUATION OF NEW ORLEANS
On August 26, 2005, the National Hurricane Center predicted that Katrina would make landfall southeast of New Orleans, and Louisiana declared a state of emergency. On August 28, a mandatory evacuation was ordered for New Orleans. Approximately 80% of residents evacuated in advance of the storm, and 20000 sought refuge in the Superdome in downtown New Orleans. Hurricane Katrina reached New Orleans on August 29, with sustained winds of 125 miles per hour. Within hours the Industrial and 17th Street canal levees were breached, and portions of the city were under 6 to 10 feet of water. Like much of the city, the VA medical center lost public power and communications and resorted to emergency backup systems. By August 30, more of the city’s protective levees failed, and 80% of the city was under water, including the field level of the Superdome. Rescue and evacuation operations began. By September 2, all 192 New Orleans VA inpatients and 367 staff and family members were evacuated and relocated to other VA medical centers.
Patients from the New Orleans area faced medical care challenges. Tens of thousands of New Orleans evacuees required urgent medical care. More than 200000 had chronic conditions needing ongoing management, the most common reason for care in evacuation centers.37,38 In the rush to evacuate, many left home without documents, medications, and other essentials.39–43 Even those who had their medications with them were separated from their health care providers and, in some instances, their families. Responding clinicians were challenged with assessing unfamiliar and ill evacuees without the benefit of their medical charts. The nation will probably never have complete data on how many evacuees were unable to continue their medical regimens without interruption and what consequences resulted.
The experiences of VA patients and providers stand in stark contrast to those of non-VA evacuees. VA efforts to maintain appropriate and uninterrupted care were supported by nationwide access to comprehensive electronic health record systems. In this article, we describe electronic health data use by the VA in the month after Katrina, including supporting technologies, the extent and nature of information accessed, and lessons learned.
METHODS
Regional Data Warehouse
The VISN 16 data warehouse contains a regularly updated subset of clinical data, extracted from the VistA systems at each of the medical centers in the region, for operational analyses. The data include demographics, in-patient and outpatient medications, visits (including diagnoses), laboratory results, and vital signs. Text-based documents (e.g., progress notes, discharge summaries, and procedure reports) are not included.
On August 30, regional (VISN 16) staff began receiving telephone requests for evacuee-specific data from its data warehouse. Staff initially retrieved data on a case-by-case basis via manual queries. The volume and similarity of requests led regional and national staff to create a call center and to build Web-based interfaces by September 1 that permitted authorized users within the VA’s private, secure, national network to retrieve clinical information without a human intermediary.
VistA “Rehosting”
The VA “rehosted” the New Orleans VistA system, moving its data and programs to a physical computer system in Houston, Tex, a task made relatively easy by the VA’s standard software, hardware, network, and access protocols. On September 2, backup tapes from New Orleans, made on August 30, were delivered to Houston, and all of the patient data was available nationwide within 7 hours. On September 5, additional tapes, including an estimated 900 progress notes, 800 prescriptions, and 2000 outpatient clinic orders on evacuees seen at the VA Baton Rouge Outpatient Clinic on September 1 and 2, were delivered to Houston. Before Katrina, the Baton Rouge clinic relied on the New Orleans VistA system for electronic health record support; on September 2, when the New Orleans system was shut down, electronic health record support for the clinic was transferred to the VistA system at the Alexandria, La, VA medical center.
Health care providers accessed the data on the rehosted New Orleans VistA system using CPRS remote data views and a relatively new tool named VistAWeb. Because logs of remote data views use were not made available for analysis, our data for VistAWeb under-reports the actual benefits achieved by VA.
VistAWeb
Developed at the Ann Arbor, Mich, VA medical center, VistAWeb uses a master patient index and locator for veterans enrolled in the VA health care system and lists their VA sites of care, retrieves data from multiple sites automatically, and presents the user with the integrated results. VistAWeb offers several advantages over CPRS remote data views: better data organization and integration, access to more data types, no date restrictions, and ease of use and installation. VistAWeb gives access to up-to-date data from care at any site, unlike the static data accessible from the regional data warehouse. Thus, on September 16, the VA declared VistAWeb the preferred method for accessing New Orleans veterans’ clinical information.
Consolidated Mail-Out Pharmacy
Patient-specific data were also made available for automated prescription fulfillment. The Mid South VA Consolidated Mail-Out Pharmacy (CMOP) in Murfreesboro, Tenn, serves New Orleans–area veterans. The pharmacy maintains its own VistA system to process outpatient prescriptions, which numbered 19.5 million for 22 facilities in 2005. After Katrina, commercial telecommunication networks to CMOP from Jackson, Miss; Biloxi, Miss; and New Orleans were interrupted, although the VistA systems remained online within their medical centers. Biloxi and Jackson copied the data files to CD and transported them to areas where telecommunications were intact. Prescription transmissions from New Orleans resumed after rehosting. Routine prescription transmissions via commercial telecommunications networks were restored from Jackson within 3 days and from Biloxi within 10 days. CMOP prescriptions were not sent to zip codes that had no US mail or FedEx service.
Our retrospective study used cross-sectional panels of data collected sequentially over time to generate charts showing patterns in electronic health record system use before and after Katrina. We acquired, merged, and de-identified the system use log files for the VISN 16 data warehouse and VistAWeb. Patterns of electronic health data access for New Orleans veterans between August 22 and September 30, 2005, are described.
RESULTS
Between August 29 and September 30, other sites in VISN 16 provided inpatient or outpatient treatment for 4125 New Orleans veteran evacuees (10.3% of 39910 New Or-leans VA patients; Table 1▶). VISN 16 pharmacies filled prescriptions for 14643 patients (37.9%) in this time period. An additional 2435 New Orleans evacuees (6.1%) received inpatient or outpatient treatment at sites outside VISN 16.
TABLE 1—
Care Delivery to New Orleans Veteran Evacuees: August 30, 2005–September 30, 2005
| Site Delivering Care | Patients With Inpatient or Outpatient Visits | Patients with Outpatient Medication Fills (With or Without a Visit) | Patients With Any Service |
|---|---|---|---|
| VISN 16 Alexandria, La | 1377 | 4506 | 4692 |
| VISN 16 Biloxi, Miss | 353 | 343 | 427 |
| VISN 16 Fayetteville, NC | 33 | 22 | 32 |
| VISN 16 Houston, Tex | 1054 | 8266 | 8269 |
| VISN 16 Jackson, Miss | 772 | 700 | 828 |
| VISN 16 Little Rock, Ark | 131 | 455 | 489 |
| VISN 16 Muskogee, Okla | 27 | 24 | 26 |
| VISN 16 Oklahoma City, Okla | 21 | 19 | 24 |
| VISN 16 Shreveport, La | 357 | 308 | 337 |
| VISN 16 Total | 4125 | 14 643 | 15 124 |
| All Other VISNs Total | 2435 |
Note. VISN 16 = Veterans Integrated Service Network 16. Before Katrina, the New Orleans Veterans’ Affairs Medical Center and its outpatient clinics provided care to 39 910 veterans.
Between August 31 and September 19, the VISN 16 data warehouse logged 8429 requests for data on 5493 New Orleans VA patients (14% of New Orleans VA patients) made by 1376 users (including clinicians and administrators) at 207 sites, including clinics, in 37 states. Multiple data requests were made for 1456 patients. The busiest day was September 6, when the data warehouse answered 995 requests on 776 patients generated by 321 users at 78 sites in 27 states.
Between August 29 and September 30, VistAWeb logged 59 454 requests for Web pages containing clinical data on 11490 (29%) New Orleans VA patients made by 2298 users from 115 different VistA systems (90% of 128 VistA systems nationwide). The most commonly requested Web pages were various text-based reports, progress notes, and medication lists, followed by patients’ medical problem lists, doctors’ orders, and laboratory test results. Table 2▶ lists the top 10 most commonly requested data types. The busiest day for VistAWeb was September 14, when 4902 requests for clinical data on 1328 patients were generated by 369 users at 54 medical centers.
TABLE 2—
Most Common Types of Data Requested From New Orleans Clinical Records Using VistAWeb: August 27 and September 30, 2005
| Data Type | Requests | Percentage of Total Requests |
|---|---|---|
| Text-based reports, othera | 13 478 | 22.67 |
| Progress note text | 11 672 | 19.63 |
| Text-based notes catalog | 10 417 | 17.52 |
| Medications: inpatient | 7659 | 12.88 |
| Medications: outpatient | 4809 | 8.09 |
| Patients’ medical problem list | 1880 | 3.16 |
| Doctors’ orders | 1499 | 2.52 |
| Lab results: chemistry and hematology | 1283 | 2.16 |
| Discharge summary | 1128 | 1.90 |
| Radiology reports | 1088 | 1.83 |
a “Other ” text-based reports include a wide variety of information, such as demographics, discharge diagnoses, immunizations, and health summaries. Requests for pages performing operational functions, such as system login and patient identification, are not included.
Together, the VISN 16 data warehouse and rehosted VistA system in Houston answered requests for clinical data on 14941 patients (38% of New Orleans VA patients) between August 29 and September 30. Compared with a pre-Katrina daily average of 1717 (May to July 2005), 1652 New Orleans patients had data accessed on September 14 (Figure 1▶). Requests came from 125 medical centers in 48 states (none from North Dakota or Delaware) and the District of Columbia (Figure 2▶). The top 10 states issuing data requests were: Louisiana (32108), Texas (15976), Mississippi (4462), Arkansas (4260), Alabama (2657), Florida (2258), Missouri (2145), Georgia (1528), Tennessee (1395), Michigan (1119), and Wisconsin (1065).
FIGURE 1—
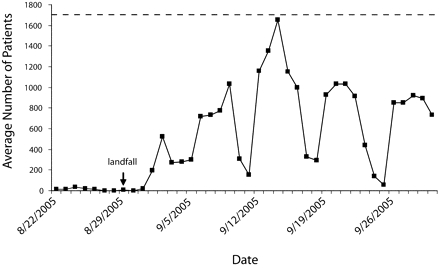
Daily count of the number of unique New Orleans Veterans’ Affairs patients whose electronic health record data were accessed through the Veterans Health Information Systems and Technology Architecture (VistAWeb) or the Veterans Integrated Service Network 16 data warehouse.
Note. Dotted lines indicate the average number of patients per day May–July 2005 (n = 1717).
FIGURE 2—
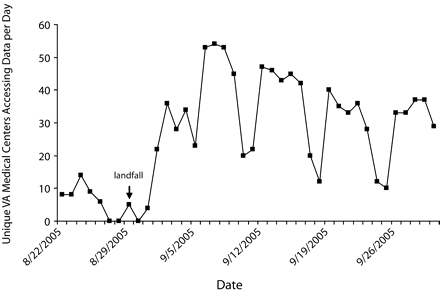
Daily count of the number of unique Veterans Affairs Medical Centersa accessing data on New Orleans Veteran’s Affairs patients through Veterans Health Information Systems and Technology Architecture Web or the Veterans Integrated Service Networks 16 data warehouse.
aClinics and campuses counted as parent Veterans’ Affairs medical center.
Before Katrina, New Orleans–area veterans had 75 292 prescriptions filled by the Mid South CMOP in July and 71 513 in August. In September, after the hurricane, CMOP filled 27 567 prescriptions generated by the rehosted system, and an additional 14 643 prescriptions were filled at other VISN 16 sites.
DISCUSSION
Hurricane Katrina separated hundreds of thousands of New Orleans evacuees from their health care providers and their medical charts. For those who were ill or under treatment, this was a major disruption in care.
The outcome was different for enrolled veterans. Their complete electronic clinical records were available from the rehosted VistA system to authorized users with access to VA’s secure network. By the end of September, VA providers had accessed clinical data for 38% (14941 of 39910) of New Orleans VA medical center patients. Approximately 1000 patients per day had data accessed during midweek peaks, a rate approximately two thirds of pre-Katrina values. The maximal rate of 1652 patients per day nearly equals pre-Katrina values. Health care data were transmitted to more than 2300 users at more than 200 VA sites of care in 48 states and the District of Columbia. These data were used to provide continuity of care documented by records of inpatient stays, outpatient visits, and prescription refills for displaced veterans (Table 1▶).
Significantly, progress notes and other text-based reports were requested more often than prescriptions, followed by patients’ medical problem lists, doctors’ orders, and laboratory test results, in that order. Although pharmacy and laboratory computerization is common in US health care settings,44 our findings suggest that these modalities alone will not be sufficient for future disaster support systems. Access to a full electronic health record system will be critical.
The VA was able to meet immediate patient care data needs and provide continuity of operations using its electronic health record system and derivative data, although VistA was never designed to provide seamless support for large-scale disasters. Moreover, after the Katrina experience, VA staff implemented new methods to ensure uninterrupted availability to VistA data; these new techniques, which combine routine backups and continuous data feeds to remote rehost sites, were used within weeks in preparation for hurricanes Rita and Wilma.
The inability of 3 sites that were up and running but without national network connections to transmit routine prescription data underscored the criticality of data communications to maintaining operations. To prevent such service interruptions in the future, the VA has contracted for satellite network access as an additional option in its contingency plans for large-scale disasters. We also learned that reviews of privacy regulations and statutes are needed to develop protective yet flexible “break-the-glass” provisions to allow for timely disaster responses outside of normal operations.
In a parallel effort to make evacuees’ medication and allergy information available nationwide via a secure Internet Web site, KatrinaHealth.org was launched by private companies, nonprofit organizations, government bodies, and community pharmacies. Despite its start-up status, the partners overcame organizational and technical barriers to create a database of 7 million prescriptions for 1 million persons from 150 zip codes accessible by approximately 25000 (approximately 50%) pharmacies as of September 22.45 By mid-October, the Web site had received more than 2000 inquiries from clinicians nationwide, a considerable number given the time constraints for system development and user education.46
The VA and KatrinaHealth.org initiatives are not directly comparable. The VA’s single organizational structure and staff were already experienced in the use of a fully featured electronic health record system, which permitted the VA response to be well underway by August 31 and its system reached its peak use on September 14. In contrast, KatrinaHealth.org made its first broad call to action on September 3, implemented a workable technical solution, and made prescription data available by September 22. The authors believe that both initiatives will stand as historical markers of the value and importance of sharable electronic health information.
Limitations
CPRS remote data views has been available for several years and was likely the primary method of data retrieval for some clinicians. Our use estimates did not include this source and understate total electronic health record system use. Because of this understatement, it is difficult to assess the number of veterans who did not receive care from our data set. Our estimates may include data used in routine care for nondisplaced veterans at 2 outlying clinics. If we exclude all 2123 outpatient clinic patients from our analysis, the result is an electronic health record system evacuee data access rate of 34%.
VistAWeb and the VISN16 data warehouse applications track different information about requestors and their locations. The data warehouse records the specific physical location of the requestor, whether it be a parent medical center, a campus, or an outpatient clinic, whereas VistAWeb logs only the requesting site’s parent medical center (i.e., supporting VistA electronic health record system “site”). Because campuses and community outpatient clinics are usually geographically separate from their parent medical center, our estimate of the total number of sites requesting data on New Orleans evacuees is low. We did not merge the requestor data sets for the data warehouse and VistAWeb because of differences in tracked information. The number of VistAWeb users represents a lower limit of the total users. VISN 16 data warehouse users were presented with a sorted table of all available results (e.g., laboratories, medications, or diagnoses) for a chosen veteran. Thus, our data type analysis is limited to VistAWeb requests. Some VistAWeb text-based reports contain data types that overlap with other categories of requested pages; for example, a health summary text-based report may contain progress notes, laboratory test results, and other data. Quantification of the impact of this overlap is not possible with available data.
Conclusions
Fulfilling health care needs without adequate medical charts is difficult under any circumstance. Although the nation may never again see a mass evacuation of a major city, smaller evacuations, such as ones because of brush fires, do occur with some regularity. Moreover, individuals move about the country in great numbers during changes in residence, business trips, and vacations. When these “displaced” persons seek medical care, it is usually in the absence of their medical charts.
Our findings suggest that medications and laboratory results, although among the most commonly available,44 may not be sufficient. More complete electronic health records are a step in the right direction but not the only step. The capability to provide secure data sharing among different electronic health record systems is also necessary. Ultimately, shared electronic health record system data should be fully usable by both clinicians and computer systems, that is, truly interoperable. For example, shared medication data should be incorporated directly into the receiving site’s automated drug–drug interaction checking systems on receipt. This requires investment in and commitment to data standards and interoperability. Through these and other steps, the country can improve health care delivery on a daily basis and be better prepared for future disasters.
Acknowledgments
The Department of Veterans Affairs provided funding for the projects described in this article.
The authors wish to thank Veterans Affairs staff around the country for their remarkable efforts to provide healthcare to displaced veterans. Care providers, ancillary health professionals, technical staff, and support staff and leadership overcame numerous obstacles and truly gave of themselves in this time of crisis.
The authors also wish to thank Robert Lynch, Charles Gephart, Michael Truett, Francisco Vazquez, Bill Falbe, and Marcia Pickard, each from the Department of Veterans Affairs, for their uncompensated contributions of administrative, technical, and material support. They also acknowledge the compensated editorial assistance of Judy Douglas in the preparation of this article.
Human Participant Protection The institutional review board of Vanderbilt University and the Veterans Affairs Tennessee Valley Healthcare System Research and Development Committee approved this study.
Peer Reviewed
Contributors S. H. Brown contributed conception and design, data acquisition, analysis and interpretation of data, drafting and critical revision of the article, and statistical analysis. L. F. Fischetti contributed conception and design, analysis and interpretation of data, and drafting and critical revision of the article. G. Graham contributed analysis and interpretation of data and critical revision of the article. J. Bates contributed data acquisition, analysis and interpretation of data, and critical revision of the article. A. E. Lancaster contributed data acquisition, analysis and interpretation of data, and critical revision of the article. D. McDaniel contributed conception and design, and drafting and critical revision of the article. J. Gillon contributed data acquisition, analysis and interpretation of data, and critical revision of the article. M. Darbe contributed data acquisition, analysis and interpretation of data, and critical revision of the article. R. M. Kolodner contributed conception and design, analysis and interpretation of data, and drafting and critical revision of the article.
References
- 1.Barnett GO. Computers in patient care. N Engl J Med. 1968;279:1321–1327. [DOI] [PubMed] [Google Scholar]
- 2.Bleich HL, Beckley RF, Horowitz GL, et al. Clinical computing in a teaching hospital. N Engl J Med. 1985;312:756–764. [DOI] [PubMed] [Google Scholar]
- 3.McDonald CJ, Tierney WM. Computer-stored medical records. Their future role in medical practice. JAMA. 1988;259:3433–3440. [PubMed] [Google Scholar]
- 4.Shortliffe EH, Tang PC, Detmer DE. Patient records and computers. Ann Intern Med. 1991;115: 979–981. [DOI] [PubMed] [Google Scholar]
- 5.Rootenberg JD. Computer-based patient records: the next generation of medicine? JAMA. 1992;267: 168–169. [DOI] [PubMed] [Google Scholar]
- 6.Barnett GO, Jenders RA, Chueh HC. The computer-based clinical record—where do we stand? Ann Intern Med. 1993;119:1046–1048. [DOI] [PubMed] [Google Scholar]
- 7.Powsner SM, Wyatt JC, Wright P. Opportunities for and challenges of computerisation. Lancet. 1998; 352:1617–1622. [DOI] [PubMed] [Google Scholar]
- 8.Tang PC, LaRosa MP, Gorden SM. Use of computer-based records, completeness of documentation, and appropriateness of documented clinical decisions. J Am Med Inform Assoc. 1999;6:245–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson ME. Introduction to programmerless systems development in mumps. In: Proceedings of the Fourth Annual Symposium on Computer Applications in Medical Care; November 2–5, 1980; Washington, DC.
- 10.Bush IE. New methods of developing large information systems. In: Proceedings of the Fifth Annual Symposium on Computer Applications in Medical Care; November 1–4, 1981; Washington, DC.
- 11.Ivers MT. End user application development—observations in VA medical centers. In: Proceedings of the Fifth Annual Symposium on Computer Applications in Medical Care; November 1–4, 1981; Washington, DC.
- 12.Corrigan GE. Robotics in the diagnostic medical laboratory. In: Proceedings of the Fifth Annual Symposium on Computer Applications in Medical Care; November 1–4, 1981; Washington, DC.
- 13.Dayhoff RE. Computer applications in laboratory medicine. In: Proceedings of the Fifth Annual Symposium on Computer Applications in Medical Care; November 1–4, 1981; Washington, DC.
- 14.Dayhoff RE, Ledley RS, Park C, Dudley AW. A new instrument for computerized surgical pathology. In: Proceedings of the Fifth Annual Symposium on Computer Applications in Medical Care; November 1–4, 1981; Washington, DC.
- 15.Ginsburg RE, Tatarczuk JR, Roy GR. An anatomic pathology system using the file manager. In: Proceedings of the Fifth Annual Symposium on Computer Applications in Medical Care; November 1–4, 1981; Washington, DC.
- 16.Forrey AW, Metcalf RW. A prototype standalone nutritive analysis and database system. In: Proceedings of the Fifth Annual Symposium on Computer Applications in Medical Care; November 1–4, 1981; Washington, DC.
- 17.Johnson ME. Pulmonary testing laboratory application. In: Proceedings of the Fourth Annual Symposium on Computer Applications in Medical Care; November 2–5, 1980; Washington, DC.
- 18.Dickie KJ. Computers in the pulmonary service. In: Proceedings of the Fourth Annual Symposium on Computer Applications in Medical Care; November 2–5, 1980; Washington, DC.
- 19.Bates MJE. Mental health I. In: Proceedings of the Fifth Annual Symposium on Computer Applications in Medical Care; November 1–4, 1981; Washington, DC.
- 20.Hammond KW, Munnecke T. A computer-assisted interactive treatment planning system for mental health. In: Proceedings of the Fifth Annual Symposium on Computer Applications in Medical Care; November 1–4, 1981; Washington, DC.
- 21.Lushene RE. Development of a psychological assessment system. In: Proceedings of the Fifth Annual Symposium on Computer Applications in Medical Care; November 1–4, 1981; Washington, DC.
- 22.Timson GF. Month-at-a-glance ambulatory scheduling system. In: Proceedings of the Fifth Annual Symposium on Computer Applications in Medical Care; November 1–4, 1981; Washington, DC.
- 23.McGuire JF, Cooper RM. The Veterans Administration’s approach to hospital automation. In: Proceedings of the sixth annual Symposium on Computer Applications in Medical Care; October 23–26, 1983; Baltimore, Md.
- 24.Ivers MT, Timson GF, von Blankensee H, Whitfield G, Keltz PD, Pfeil CN. Large scale implementation of compatible hospital computer systems within the Veterans Administration. In: Proceedings of the sixth annual Symposium on Computer Applications in Medical Care; October 23–26, 1983; Baltimore, Md.
- 25.Anderson CL, Meldrum KC. The VA computerized patient record—a first look. In: Proceedings of the Symposium on Computer Applications in Medical Care; November 5–9, 1994; Washington, DC. [PMC free article] [PubMed]
- 26.Meldrum K, Volpp B, Vertigan R. Department of Veterans Affairs’ computerized patient record system. Proc AMIA Symp. 1999;1–2:1214. [Google Scholar]
- 27.Payne TH. The transition to automated practitioner order entry in a teaching hospital: the VA Puget Sound experience. Proc AMIA Symp. 1999:589–593. [PMC free article] [PubMed]
- 28.Murff HJ, Kannry J. Physician satisfaction with two order entry systems. J Am Med Inform Assoc. 2001;8:499–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lovis C, Chapko MK, Martin DP, et al. Evaluation of a command-line parser-based order entry pathway for the Department of Veterans Affairs electronic patient record. J Am Med Inform Assoc. 2001;8: 486–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johnson CL, Carlson RA, Tucker CL, Willette C. Using BCMA software to improve patient safety in Veterans Administration Medical Centers. J Health Inf Manage. 2002;16:46–51. [PubMed] [Google Scholar]
- 31.Morgan MW. The VA advantage: the gold standard in clinical informatics. Health Pap. 2005;5: 26–29. [DOI] [PubMed] [Google Scholar]
- 32.Anderson M. Lessons learned from the Veterans Health Administration. Health Pap. 2005;5:30–37. [DOI] [PubMed] [Google Scholar]
- 33.Ramirez B, Nazaretian M. Quality, value, accountability and information as transforming strategies for patient-centred care: a commentary from an international perspective. Health Pap. 2005;5:52–55. [DOI] [PubMed] [Google Scholar]
- 34.Stewart M. Can a healthcare system be transformed? Lessons from the past decade at the Veterans Health Administration. Health Pap. 2005;5:56–59. [DOI] [PubMed] [Google Scholar]
- 35.Boodman S. No end to errors. Washington Post. December 3, 2002:HE01.
- 36.Rundle R. In the drive to mine medical data, VHA is the unlikely leader. Wall Street Journal. December 10, 2001;1.
- 37.Townsend FF. The federal response to Hurricane Katrina lessons learned. In: White House Assistant to the President for Homeland Security and Counterterrorism. Washington, DC: US Government Printing Office; 2006.
- 38.Centers for Disease Control and Prevention. Morbidity surveillance after Hurricane Katrina—Arkansas, Louisiana, Mississippi, and Texas, September. 2005. MMWR Morb Mortal Wkly Rep. 2006;55:727–731. [PubMed] [Google Scholar]
- 39.Check E. Hurricane Katrina: left behind. Nature. 2005;437:467. [DOI] [PubMed] [Google Scholar]
- 40.Henderson GS. Hurricane Katrina. Finding supplies. N Engl J Med. 2005;353:1542. [DOI] [PubMed] [Google Scholar]
- 41.Henderson GS. Hurricane Katrina. Triaging tragedy. N Engl J Med. 2005;353:1551. [DOI] [PubMed] [Google Scholar]
- 42.Bower A. Katrina’s lingering medical nightmare. Time. Sepember 22, 2005.
- 43.Select Bipartisan Committee to Investigate the Preparation for and Response to Hurricane Katrina. A Failure of Initiative. Final Report of the Select Bipartisan Committee to Investigate the Preparation for and Response to Hurricane Katrina. Washington, DC: US Government Printing Office; 2006.
- 44.Poon EG, Jha AK, Christino M, et al. Assessing the level of healthcare information technology adoption in the United States: a snapshot. BMC Med Inform Decis Mak. 2006;6:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.KatrinaHealth.org. KatrinaHealth Press Conference. September 22, 2005. Available at: http://katrinahealth.org/Katrina_Health_09_22_05.wma. Accessed Feburary 16, 2006.
- 46.Brewin B. Diaspora dispatches. Available at: http://govhealthit.com/article91419-11-14-05-Print. Accessed March 20, 2007.


