Abstract
Objectives. Hurricane Katrina’s impact on public health has been significant and multifaceted, with trauma-related psychological sequelae likely to result in a sizable burden of disease. Data were collected that assessed acute stress disorder (ASD) prevalence and factors related to ASD symptomatology among sheltered evacuees.
Methods. On days 12 to 19 after Katrina, evacuees at a major emergency shelter completed surveys that assessed demographics, Katrina-specific experiences, and ASD symptomatology.
Results. Sixty-two percent of the sample met ASD threshold criterion. Projections based on the predictive power of ASD to posttraumatic stress disorder (PTSD) suggest that 38% to 49% of the sample will meet PTSD criteria 2 years post-disaster. Female gender (odds ratio [OR] = 4.08), positive psychiatric history (OR=5.84), injury (OR=2.75), increased life-threat perception (OR=1.37), and decreased sense of personal control (OR=1.56) were significantly related to ASD. Black race was associated with greater symptom severity (B=7.85, SE[B]=3.50).
Conclusions. Katrina-related trauma and its psychological sequelae will remain a significant public health issue for years to come. The identification of several vulnerability factors related to ASD and PTSD provides a brief sketch of those at greatest risk.
Between late August and September 4, 2005, the Red Cross operated 470 shelters and evacuation centers across the nation to accommodate survivors of Hurricane Katrina.1 More than 386000 evacuees received medical or mental health services from such shelters,2 and survivors remained widely dispersed for significant periods, temporarily residing in all 50 US states and the District of Columbia.3 Common evacuee health care concerns include poor sleep quality,4 depressed immune functioning,5,6 increases in negative health behaviors (e.g., alcohol and cigarette use),7 and elevated relapse rates for pre-existing health conditions.8 Although primary care physicians and other health care providers are often well prepared to manage physical needs in the immediate wake of disaster, their role as sole treatment contact9,10 for the more than 50% of evacuees who will experience persistent and severe psychological consequences is likely less familiar. Given the mental health repercussions of Hurricane Katrina projected to emerge in the coming years, including depression, anxiety, and post-traumatic stress disorder (PTSD),11,12 physician and health care provider familiarity with trauma-related symptoms and differential risk profiles is crucial.
Multiple vulnerability factors have combined in the case of Hurricane Katrina to heighten survivors’ risks of long-term difficulties. The high rate of poverty in New Orleans (close to 28%) amplified disaster impact on individuals through increased exposure, decreased disaster preparedness, and a lack of resources to offset losses.13 Also, the largely Black population of New Orleans bore a disproportionately heavy burden of predisaster chronic disease complicated by inadequate health care access.14 Minority status itself has been shown to increase the risk of PTSD after trauma,13,15 although this effect may be largely because of differential exposure to poverty and violence.16,17 Also, previous disaster research has shown that separation from family18 and relocation19 elevate risk for postdisaster mental health problems. A recent meta-analysis investigating the effects of displacement on mental health outcomes indicated that displaced persons evince worse mental health than nondisplaced comparison groups and that internally displaced persons (displaced within their own country) experience worse outcomes than refugees relocated to other countries. Living in institutional accommodations, as opposed to private housing, and experiencing restricted economic opportunity are also consistently associated with worse mental health.20
After Cyclone Tracy devastated the community of Darwin, Australia, a study of survivors found that evacuees who did not return to the community within 1 year fared worse in terms of somatic complaints, depression, and worry than did both individuals who evacuated but returned and those who had never evacuated during the disaster.21,22 In a recent review of the displacement literature, the authors suggested that the negative effects of forced relocation spring largely from the loss of social ties and support systems.23 With hundreds of thousands of evacuees dislocated all over the country, Hurricane Katrina has set the stage for a public mental health crisis that may unfold for years to come.
In post-Katrina New Orleans, the outlook may be no better for evacuees with the means and desire to return to their communities. A recent New York Times report illustrated the multitude of mental health consequences that have accompanied the disaster and rebuilding.24 The suicide rate in the area tripled in the first 4 months and remains significantly higher than the pre-Katrina rate; substance abuse and mental health needs have reached unprecedented levels; and many feel that the rest of the country has lost interest. Complicating this crisis, more than half of New Orleans’ mental health professionals have relocated elsewhere, and only 60 of the city’s hospital beds are available for psychiatric patients.24
We sampled residents of New Orleans and surrounding parishes who were evacuated to the major Red Cross shelter in Austin, Tex, within the first 2 weeks of the Katrina disaster. Our study is the first, to our knowledge, to examine how demographic and disaster-related experiences predict acute stress symptomatology among Katrina’s evacuees. Acute stress disorder (ASD), a major stress response in the first month posttrauma, or “early PTSD,” was chosen as the mental health outcome of interest because of its use in predicting PTSD up to 2 years postevent.25,26
METHODS
Sampling and Data Collection
Data were collected over 7 days at the Austin Convention Center, which housed approximately 1600 Hurricane Katrina evacuees. Collection was initiated 12 days after Hurricane Katrina made landfall outside New Orleans. Access to the shelter was granted by the City of Austin and Travis County Emergency Medical Services. Survey booths were set up in 4 different locations to increase researcher visibility and to provide a representative sample of the shelter population. Because of the anonymous nature of the data obtained, written informed consent was waived. Information was given in written and verbal form to all of the participants describing the purpose, risks, and benefits of study participation.
Instruments
The research instrument was a structured survey consisting of demographic and background questions, a lifetime trauma history questionnaire, Katrina-specific items, and the Acute Stress Disorder Scale (ASDS). Survey completion required approximately 15 minutes, and interviews were offered to visually impaired or low-literacy participants. A total of 175 surveys were distributed, of which 132 were completed sufficiently for analysis (75%). Twelve percent of the surveys were administered in interview format; responses did not differ significantly by format.
Demographic variables were assessed using items adapted from the US Census Report. Participants were asked to write in their age and parish of residence. For all other demographic items, participants were asked to check the appropriate box. Categories assessed were race/ethnicity, gender, marital status, household income, pre-Katrina employment status, receipt of public assistance, level of education, number of children, and self- or physician-diagnosed mental health problems.
Previous exposure to trauma was assessed with the Traumatic Events Questionnaire.27 The Traumatic Events Questionnaire assesses experiences with 9 stressors defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition,25 as criterion A1 for PTSD as being of sufficient intensity to elicit posttraumatic stress symptoms. For each event endorsed, respondents indicate how many times the event occurred (1, 2, 3 or more).
Katrina-specific items were constructed based on previous disaster research and media reports of the evolving situation in New Orleans and evacuation shelters.28 Katrina-specific items assessed exposure to stressors (number of days waited for evacuation; experience of injury, illness, or the exacerbation of a pre-existing health problem; seeing dead bodies; death of relative or loved one; separation from family members; and loss of home or vehicle) by asking participants to what extent they had experienced each stressor, and assessed perceived impact of stressors by asking participants to rate on a scale of 0 (not at all) to 6 (extremely) the statements regarding their disaster-related perceptions (preparation for Katrina, perceived stressfulness of evacuation, perceived life threat during Katrina, and perceived control over present circumstances).
ASD symptoms were assessed with the ASDS,29 a self-report inventory consisting of 19 items based on criteria for ASD as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.25 Based on previous research, between 72% and 83% of those who develop ASD go on to meet criteria for PTSD at 6 months posttrauma30,31 and between 63% and 80% at 2 years posttrauma.26,32 Validation studies revealed that an ASDS cutoff score of 56 correctly identified 91% of people who developed subsequent PTSD and 93% who did not.33 Therefore, this cutoff was adopted as the threshold score for this study. Participants exceeding this threshold were classified as having levels of acute stress symptoms indicative of high risk for subsequent PTSD.29,34 Analyzed as a continuous outcome (number and severity of symptoms endorsed), the ASDS serves as a measure of current trauma-related distress, distinct from its prognostic significance.35 ASDS total score was, therefore, analyzed as a measure of symptom severity. The ASDS has been shown to possess good reliability and validity in previous studies and has good sensitivity (95%) and specificity (83%) for identifying ASD compared with clinical interviews.29 In the present study, the ASDS showed high internal reliability (Cronbach α = .92).
Social and occupational functional impairment was assessed using a 5-item self-report scale. Participants were asked to rate on a scale of 0 (not at all) to 4 (extremely) the degree to which Katrina had interfered with the ability to experience companionship, social support and community, intimacy, overall personal achievement, and achievement in career or work. The scale showed good internal reliability in the present sample (Cronbach α = .80).
Statistical Analysis
Logistic regression was used to predict an above-threshold score on the ASDS. First, bivariate odds ratios for ASD were calculated for demographic and background variables (age, race/ethnicity, gender, marital status, income level, receipt of public assistance, employment status, education, parish of residence, psychiatric history, and previous trauma exposure), as well as for Katrina-specific variables (experiences of injury, illness, exacerbation of a pre-existing health problem, exposure to corpses, death of a relative or loved one, separation from family, and property loss). A multivariate logistic regression model was created using significant bivariate predictors (P < .05) chosen for both theoretical soundness and noncollinearity. Next, to identify variables associated with severity of acute stress symptoms, bivariate correlations were calculated between ASDS total score and the above demographic, background, and Katrina-specific variables. ASDS total score was regressed on those bivariate predictors found to be both significant (P < .05) and independent from other predictors (variance inflation factor ≤ 1.5) in a multivariate linear regression model. The first and second authors carried out all of the analyses.
RESULTS
Description of Sample
Participants were 132 adult evacuees (56% men and 44% women; mean age, 43 y; range, 20–80 y) from New Orleans and surrounding parishes. The sample was 74.2% Black, 16.7% non-Hispanic White, 3% multiracial, 1.7% Hispanic, and 2.4% “other.” Eighty-one percent reported a high school diploma or higher, with 22% having completed college or an advanced degree. Thirty-seven percent of participants reported an annual income of less than US $10 000, with 45% reporting between US $10 000 and US $30 000, and 18% reporting an income greater than US $30000. Sixty-seven percent of all participants reported a previous psychiatric condition (depression, 33%; anxiety, 20%; bipolar disorder, 8%; schizophrenia, 4%; PTSD, 3%), with the distribution of diagnoses evincing a similar pattern across income levels.
Of those participants in the lowest income group (less than US $10000), 78% were Black, 17.1% were non-Hispanic White, 2.4% were Asian, and 2.4% were multiracial. The rate of employment in at least part-time work was 57% for this group, as was the rate of enrollment in a public assistance or disability program. Fifty-four percent of these participants had a positive psychiatric history. Of those participants in the highest income group (more than US $30000), 50% were Black, 45% were non-Hispanic White, and 5% were multiracial. Ninety-five percent of these participants were employed either part-or full-time, with 10% receiving a form of public assistance or disability. Similar to the lowest income group, 55% of these participants reported a positive psychiatric history.
Katrina-Specific Experiences and Perceptions
Nearly all participants (95%) waited multiple days to be evacuated from the New Orleans area (mean = 3.99; SD= 2.78), resulting in high levels of traumatic exposure and loss. Systematic differences existed in wait times, with Black participants waiting a mean of 4.73 days (SD= 2.42) for evacuation compared with 2.86 days (SD= 2.85) for White participants (t [109] = 2.83; P< .01). Figure 1▶ presents rates of particular types of Katrina-specific trauma and loss experienced by participants. The majority reported sustaining minor-to-severe injuries (62.6%) and mild-to-severe illness (71%) in the hurricane or evacuation process, whereas a sizeable minority (40%) reported the exacerbation of a pre-existing health condition (e.g., hypertension or back problems). Slightly more than 63% reported being directly exposed to corpses during the disaster. Fourteen percent of participants suffered the death of a relative or loved one, and the vast majority (81.5%) was separated from at least 1 family member for 1 day or more because of Katrina. Property loss was also prevalent and severe, with 69.5% of participants having lost their home, and 48% reporting vehicle loss. Sixty-six percent of participants who lost property lacked any form of property insurance.
FIGURE 1—
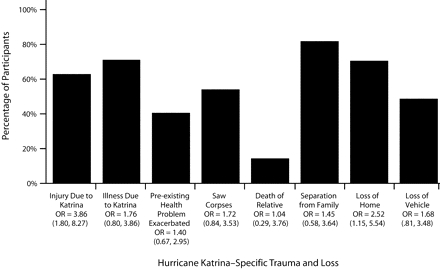
Percentage of participants who experienced Hurrican Katrina–specific trauma and loss and bivariate odds ratios (ORs; with 95% confidence intervals [CIs]) for associated acute stress disorder.
Figure 2▶ presents data on participants’ Katrina-related perceptions. On a scale of 0 (not at all about to prepare) to 6 (totally prepared), participants perceived themselves as having been unable to prepare for Hurricane Katrina (mean = 2.21; SD = 2.18). On a scale of 0 (not stressful) to 6 (extremely stressful), participants saw the evacuation as very stressful (mean = 4.66; SD = 1.87). Slightly more than half of participants (51.6%) felt a moderate-to-severe degree of life threat during the disaster, and 62% felt no-to-moderate control over the present, (mean = 2.9; SD = 2.30, with 0 being no control and 6 being total control).
FIGURE 2—
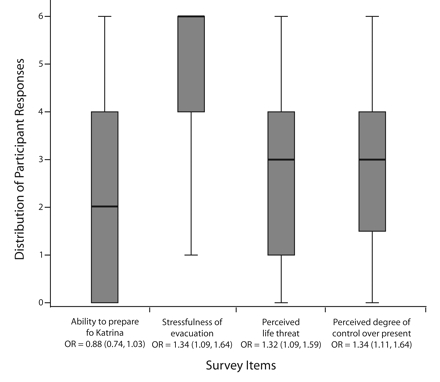
Hurricane Katrina–specific perceptions and bivariate odds ratios (ORs; with 95% confidence intervals [CIs]) for associated acute stress disorder. Note. Scale: 0 (not at all) to 6 (extremely).
Prevalence and Clinical Significance of ASD
ASDS scores ranged from 19 (lowest possible) to 95 (highest possible; mean = 61.10; SD = 19.23), with 62% of the total sample meeting ASD threshold criterion. Table 1▶ presents, by demographic group, the percentage of participants meeting the criterion. Scores on the functional impairment measure ranged from 5 (lowest possible) to 20 (highest possible; mean = 13.36; SD = 4.69). Higher ASDS scores were related to a higher degree of functional impairment (r = 0.25; P < .05). Based on the predictive power of ASD leading to PTSD, our data suggest that between 38% and 49% of the total sample of evacuees will meet criteria for chronic PTSD at 2 years post-Katrina.30,31,36
TABLE 1—
Demographic Associations With ASD Threshold Scores and Symptom Severity
| Variable (Pre-Katrina) | No. (Group %) Meeting ASD Threshold | Bivariate OR (95% CI) for ASD | ASDS Score Mean (SD) | ASDS Total Score Bivariate Correlation |
|---|---|---|---|---|
| Age, y | −.22* | |||
| 18–35 | 25 (76) | 2.30 (.80, 6.61) | 68.21 (18.64) | |
| 36–50 | 34 (64) | 1.32 (.54, 3.21) | 61.72 (16.85) | |
| ≥51 | 19 (58) | Reference | 57.24 (19.20) | |
| Race/ethnicity | .27** (Black) | |||
| Black | 62 (70) | 2.30 (.89, 5.94) | 64.88 (18.49) | |
| Hispanic or multiethnic | 5 (56) | 1.25 (.26, 5.94) | 54.44 (11.59) | |
| Non-Hispanic White | 11 (50) | Reference | 52.68 (20.50) | |
| Gender | .29** | |||
| Female | 42 (79) | 3.39 (1.50, 7.68) | 67.77 (18.35) | |
| Male | 36 (53) | Reference | 56.78 (18.55) | |
| Marital status | −.06 (Married/cohabitating) | |||
| Married or cohabitating | 19 (68) | 1.33 (.52,3.43) | 63.21 (17.59) | |
| Divorced or widowed | 22 (73) | 1.74 (.67,4.52) | 62.73 (18.65) | |
| Single | 38 (61) | Reference | 61.38 (19.33) | |
| Household income, US $ | −.08 | |||
| <10 000 | 27 (64) | .77 (.25,2.43) | 62.69 (18.51) | |
| 10 000–19 999 | 27 (77) | 1.45 (.42,5.00) | 65.26 (17.61) | |
| 20 000–30 000 | 6 (38) | .26 (.06,1.04) | 53.00 (16.61) | |
| >30 000 | 14 (70) | Reference | 61.45 (20.65) | |
| Public assistance | .13 | |||
| Yes | 33 (72) | 1.49 (.67, 3.31) | 65.40 (17.18) | |
| No | 46 (63) | Reference | 60.41 (19.21) | |
| Employment status | .03 | |||
| Employed | 57 (66) | 1.12 (.49, 2.60) | 62.65 (18.67) | |
| Unemployed | 21 (64) | Reference | 61.42 (18.48) | |
| Education | −.21* | |||
| < High school diploma | 18 (78) | 2.25 (.63, 7.99) | 69.39 (17.93) | |
| Some high school | 24 (62) | 1.00 (.36, 2.77) | 60.82 (17.53) | |
| Some college | 21 (64) | 1.09 (.38, 3.16) | 63.73 (19.00) | |
| ≥College degree | 16 (62) | Reference | 55.00 (18.64) | |
| Parish | .19* | |||
| Orleans | 72 (66) | 2.34 (.91, 6.25) | 62.72 (18.76) | |
| Other | 9 (45) | Reference | 52.25 (19.84) | |
| Psychiatric history | .13 | |||
| Yes | 44 (72) | 2.17 (1.04, 4.53) | 63.74 (19.16) | |
| No | 37 (54) | Reference | 58.74 (19.13) | |
| Previous trauma history | −.07 | |||
| 0 criterion A1 eventsa | 9 (64) | Reference | 66.86 (17.21) | |
| 1–3 criterion A1 events | 16 (59) | .81 (.21, 3.07) | 60.67 (20.93) | |
| 4–7 criterion A1 events | 22 (69) | 1.22 (.33, 4.60) | 62.19 (15.19) | |
| ≥8 criterion A1 events | 26 (63) | .96 (.27, 3.41) | 60.68 (20.11) |
Note. ASD = acute stress disorder; OR = odds ratio; CI = confidence interval; SD = standard deviation; ASDS = acute stress disorder scale.
aCriterion A1 refers to the category of stressors that may be used to diagnose posttraumatic stress disorder.25
* P < .05; **P < .01.
Demographic and Katrina-Specific Predictors of ASD
Univariate logistic regression analysis was used to examine associations between demographic and Katrina-specific variables and ASD (Table 1▶). Demographic characteristics were treated as categorical variables; disaster-specific variables were treated as either categorical (e.g., seeing dead bodies and death of family members) or continuous (e.g., degree of perceived life threat and perceived control over present).
To compare the unique importance of each risk factor for ASD, a multivariate logistic model was generated (Table 2▶) that included potential predictors that evinced significant (P < .05) associations at the bivariate level. The model was significant (χ2[5] = 41.39; P < .001) and included 5 independent predictors of ASD: perception of peridisaster life threat (OR = 1.37; 95% confidence interval [CI] = 1.08, 1.75), female gender (OR = 4.08; 95% CI = 1.45, 11.48), experience of Katrina-related injury (OR = 2.75; 95% CI = 1.05, 7.11), decreased perceived control over the present (OR = 1.56; 95% CI = 1.16, 2.09), and positive psychiatric history (OR = 5.84; 95% CI = 1.92, 17.80).
TABLE 2—
Multivariate Logistic Regression Model Predicting Acute Stress Disorder
| Multivariate OR (95% CI) | |
|---|---|
| Degree of life threat | 1.37 (1.08, 1.75) |
| Gender: female | 4.08 (1.45, 11.48) |
| Injured | 2.75 (1.05, 7.11) |
| Perceived degree of control over present | 1.56 (1.16, 2.09) |
| Positive psychiatric history | 5.84 (1.92, 17.80) |
Notes. DV: ASDS ≥ 56; χ2(5) = 41.39; P < .001.
Demographic and Katrina-Specific Predictors of ASD Symptom Severity
Bivariate correlations were used to assess relationships between demographic and Katrina-specific variables with degree of acute stress symptomatology as measured by the ASDS total score (Table 1▶). Age, income level (4 levels), and education (4 levels), were analyzed as continuous. Race/ethnicity and parish residence were each coded as dichotomous using 1/0 (i.e., 1= Black, 0 = other; 1= Orleans, 0 = other). All of the other variables were analyzed consistent with the above univariate analysis.
To compare the unique importance of each independent variable found to be significant (P < .05) at the bivariate level, a multivariate regression model was generated (Table 3▶). The model explained a significant proportion of the variance in acute stress symptom severity (R2 [adjusted] = .31; F5,109 = 11.02; P < .001) and yielded 4 significant predictors. Black race/ethnicity (B = 7.85, SE[B] = 3.50, P< .05), perception of peridisaster life threat (B = 2.29, SE[B] = 0.73, P<.01), female gender (B=8.68, SE[B]=3.02, P < .01), and the experience of Katrina-related injury (B = 7.35, SE[B] = 3.15, P < .05) were all positively related to symptom severity. Perception of control over the present was not statistically significant (B = −1.43, SE[B] = 0.75, P < .08) but was retained in the model for theoretical purposes. Participants excluded from regression analyses because of missing values were compared with participants included on relevant predictors and ASDS score using t tests for mean comparisons; no systematic differences were found.
TABLE 3—
Multiple Linear Regression Models Predicting Acute Stress Disorder Severity
| B | SE (B) | |
|---|---|---|
| Race/ethnicity: Black | 7.85** | 3.50 |
| Degree of life threat | 2.29*** | 0.73 |
| Gender: female | 8.68*** | 3.02 |
| Injured | 7.35** | 3.15 |
| Perceived degree of control over present | −1.43* | 0.75 |
Notes. DV: ASDS total score; R2(adjusted) = .31; F5,109 = 11.02; P < .001.
*P < .08; **P < .05; ***P < .01.
DISCUSSION
Our data converge with media reports of Katrina’s devastation and illustrate the severity of loss and trauma experienced by survivors (Figures 1▶ and 2▶). The PTSD projections based on our findings are consistent with PTSD rates after other major disasters, such as 34.3% after the Oklahoma City bombing,37 36% after Hurricane Andrew,11 44% after the Buffalo Creek Dam collapse and flooding,16 and 53% after the Australian bushfires.38
Poor prognosis was related to previous psychiatric history, female gender, Katrina-related physical injury, and perceived life threat, all of which have been shown previously to have robust relationships with post-disaster PTSD.12,37,39–41 Predictors of acute stress symptom severity were similar to those of threshold criterion, with Black race/ethnicity emerging as an additional predictor of distress (Table 3▶). A study of Hurricane Andrew survivors found PTSD rates of 23% among Blacks and 15% among Whites,13 although the relationship of minority status to stress response remains somewhat equivocal.13,16 Black participants in our sample were both more severely exposed and had lower mean income levels than White participants, which suggests that racial status likely conferred vulnerability on survivors through a complex interaction of factors that has been referred to as “the sociopolitical ecology of disaster.”42 Recent data also show that a greater percentage of Black residents of southern Louisiana lost jobs, health insurance, and community ties than did White residents, further increasing their vulnerability.43
One surprising finding is that previous trauma exposure did not predict acute stress response in Katrina survivors. Given the predictive relationship of ASD to PTSD, these results appear contradictory to previous findings that link previous trauma to increased risk of PTSD.44–46 The possibility exists, however, that the immediate disaster-specific trauma was so pervasive and severe in the wake of Katrina that effects of previous trauma on mental health functioning were temporarily overwhelmed. Trauma history may yet emerge as a determinant of PTSD symptomatology at a later time point.
This study has a number of limitations, including the use of a nonrandom sampling method and self-report measures. However, the high degree of correspondence on both demographic and event-related data between our sample and the Harvard School of Public Health Poll47 random sample of 680 evacuees, as well as that of the 2006 South Louisiana Recovery Survey conducted by the Louisiana Recovery Authority,43 suggests that our sample is representative of the larger population of Katrina survivors who were evacuated to emergency out-of-state shelters. Also, the severity of self-reported symptoms was related to self-reported functional impairment in our sample, suggesting clinical significance of ASD symptoms.
Despite the limitations, we believe that this study has important implications regarding mental health consequences of Hurricane Katrina. Our findings indicate that a large percentage of evacuees are likely suffering from PTSD, with few resources (e.g., financial, health care, or social) on which to draw. Individuals with limited financial resources or existing health problems are some of society’s most vulnerable in a disaster situation, both in terms of initial exposure and ability to recoup. For instance, whereas 54.4% of individuals without a previous psychiatric history met criteria for ASD, the prevalence was 77.8% for individuals with a history of an anxiety disorder and 71.4% for those with a history of depression. Thus, the management of complex disaster situations like Hurricane Katrina poses a significant challenge to the existing United States health care system and to mental health care professionals in particular.48 The lack of an adequate mental health care structure, as was evident in New York after September 11, 2001, continues to be a national problem.49 Accessibility of existing services to displaced people, who are often economically disadvantaged and of a different ethnic or socioeconomic background than service providers, is also a concern.50
Although the role of mental health care professionals in providing accessible and respectful services with an awareness of specific risk factors that increase survivors’ vulnerability is crucial, the statement, “the well-being of this population will depend on what happens not in individuals’ mental space, but in their social, economic and political lives,”51(p386–387) applies to Katrina’s victims. Helping individuals to achieve a measure of self-determination in the period of rebuilding is a strategy that has the power to influence prognoses in the difficult years to come, yet such self-determination can only be realized with adequate access to health care, permanent housing, and a social net to prevent postdisaster downward drift of the most vulnerable survivors. Although some evidence of healthcare reform in Louisiana exists,52 calls for universal health insurance have been nearly forgotten since the outraged cries heard in the immediate postdisaster period.53 Despite our seemingly short memory for this disaster, one thing remains certain: whether through the mitigation or exacerbation of distress, society’s long-term response will inevitably impact the mental health trajectory of many of Katrina’s evacuees for years to come.54,55
Acknowledgments
Edward M. Racht, Medical Director, and Jeff Brockman, Clinical Commander and Coordinator, of the City of Austin and the Travis County Emergency Medical Services provided invaluable facilitation of data collection. Stephanie Milan and Jeanne Slattery provided helpful comments on a previous version of this article without compensation.
Human Participant Protection The study was approved by the University of Connecticut institutional review board.
Peer Reviewed
Contributors M.A. Mills originated the study, supervised all aspects of its implementation, and led the writing. D. Edmondson co-led study conceptualization, design, writing, and completed the analyses. C.L. Park assisted with study design and implementation. All of the authors helped to conceptualize ideas, interpret findings, and review drafts of the article.
References
- 1.American Red Cross. One week after Katrina’s Gulf Coast assault, the American Red Cross is setting a record relief pace. Available at: http://www.redcross.org/pressrelease/0,1077,0_489_4553,00.html. Accessed October 10, 2005.
- 2.American Red Cross. American Red Cross projects Hurricane Katrina most costly relief effort in history. Available at: http://www.redcross.org/pressrelease/0,1077,0_314_4640,00.html. Accessed November 4, 2005.
- 3.Department of Homeland Security. Government response activities during the first three weeks of the recovery effort. Available at: http://www.dhs.gov/interweb/assetlibrary/katrina.htm. Accessed October 10, 2005.
- 4.Shariat S, Mallonee S, Kruger E, Farmer K, North C. A prospective study of long-term health outcomes among Oklahoma City bombing survivors. J Oklahoma State Med Assoc. 1999;92:178–186. [PubMed] [Google Scholar]
- 5.Inoue-Sakurai C, Maruyama S, Morimoto K. Post-traumatic stress and lifestyles are associated with natural killer cell activity in victims of the Hanshin-Awaji earthquake in Japan. Prev Med. 2000;31:467–473. [DOI] [PubMed] [Google Scholar]
- 6.Ironson G, Wynings C, Schneiderman N, et al. Posttraumatic stress symptoms, intrusive thoughts, loss, and immune function after Hurricane Andrew. Psychosom Med. 1997;59:128–141. [DOI] [PubMed] [Google Scholar]
- 7.Smith DW, Christiansen EH, Vincent R, Hann NE. Population effects of the bombing of Oklahoma City. J Okla State Med Assoc. 1999;92:193–198. [PubMed] [Google Scholar]
- 8.Lutgendorf SK, Antoni MH, Ironson G, et al. Physical symptoms of chronic fatigue syndrome are exacerbated by the stress of Hurricane Andrew. Psychosom Med. 1995;57:310–323. [DOI] [PubMed] [Google Scholar]
- 9.Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK. The de facto US mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993;50: 85–94. [DOI] [PubMed] [Google Scholar]
- 10.Robinson WD, Geske JA, Prest LA, Barnacle R. Depression treatment in primary care. J Am Board Fam Pract. 2005;18:79–86. [DOI] [PubMed] [Google Scholar]
- 11.David D, Mellman TA, Mendoza LM, Kulick-Bell R, Ironson G, Schneiderman N. Psychiatric morbidity following Hurricane Andrew. J Trauma Stress. 1996;9: 607–612. [DOI] [PubMed] [Google Scholar]
- 12.Goenjian AK, Steinberg AM, Najarian LM, Fairbanks LA, Tashjian M, Pynoos RS. Prospective study of posttraumatic stress, anxiety, and depressive reactions after earthquake and political violence. Am J Psychiatry. 2000;157:911–916. [DOI] [PubMed] [Google Scholar]
- 13.Perilla JL, Norris FH, Lavizzo EA. Ethnicity, culture, and disaster response: identifying and explaining ethnic differences in PTSD six months after Hurricane Andrew. J Soc Clin Psychol. 2002;21:20. [Google Scholar]
- 14.Greenough PG, Kirsch TD. Hurricane Katrina. Public health response—assessing needs. N Engl J Med. 2005;353:1544. [DOI] [PubMed] [Google Scholar]
- 15.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995; 52:1048–1060. [DOI] [PubMed] [Google Scholar]
- 16.Green BL, Grace MC, Lindy JD, Gleser GC, Leonard A. Risk factors for PTSD and other diagnoses in a general sample of Vietnam veterans. Am J Psychiatry. 1990;147:729–733. [DOI] [PubMed] [Google Scholar]
- 17.MacDonald C, Chamberlain K, Long N. Race, combat, and PTSD in a community sample of New Zealand Vietnam War veterans. J Trauma Stress. 1997; 10:117–124. [DOI] [PubMed] [Google Scholar]
- 18.Armenian HK, Morikawa M, Melkonian AK, et al. Loss as a determinant of PTSD in a cohort of adult survivors of the 1988 earthquake in Armenia: implications for policy. Acta Psychiatr Scand. 2000;102: 58–64. [DOI] [PubMed] [Google Scholar]
- 19.Najarian LM, Goenjian AK, Pelcovitz D, Mandel F, Najarian B. The effect of relocation after a natural disaster. J Trauma Stress. 2001;14:511–526. [DOI] [PubMed] [Google Scholar]
- 20.Porter M, Haslam N. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: a meta-analysis. JAMA. 2005;294:602–612. [DOI] [PubMed] [Google Scholar]
- 21.Milne G. Cyclone Tracy: I. Some consequences of the evacuation for adult victims. Aust Psychol. 1977; 12:39. [Google Scholar]
- 22.Milne G. Cyclone Tracy: II. The effects on Darwin children. Aust Psychol. 1977;12:55. [Google Scholar]
- 23.Steinglass P, Gerrity E. Forced displacement to a new environment. In: Noshpitz JD, Coddington RD, eds. Stressors and the Adjustment Disorders. New York, NY: Wiley; 1990:399–417.
- 24.Saulny S. A legacy of the storm: depression and suicide. The New York Times. Available at: http://www.nytimes.com/2006/06/21/us/21depress.html. Accessed June 21, 2006.
- 25.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association; 1994.
- 26.Harvey AG, Bryant RA. Acute stress disorder: a synthesis and critique. Psychol Bull. 2002;128: 886–902. [DOI] [PubMed] [Google Scholar]
- 27.Vrana S, Lauterbach D. Prevalence of traumatic events and post-traumatic psychological symptoms in a nonclinical sample of college students. J Traumatic Stress. 1994;7:289. [DOI] [PubMed] [Google Scholar]
- 28.Schuster MA, Stein BD, Jaycox LH, et al. A national survey of stress reactions after the September 11, 2001, terrorist attacks. N Engl J Med. 2001;345:1507. [DOI] [PubMed] [Google Scholar]
- 29.Bryant RA, Moulds ML, Guthrie RM. Acute Stress Disorder Scale: a self-report measure of acute stress disorder. Psychol Assess. 2000;12:61–68. [PubMed] [Google Scholar]
- 30.Brewin CR, Andrews B, Rose S, Kirk M. Acute stress disorder and posttraumatic stress disorder in victims of violent crime. Am J Psychiatry. 1999;156: 360–366. [DOI] [PubMed] [Google Scholar]
- 31.Bryant RA, Harvey AG. Relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. Am J Psychiatry. 1998;155:625–629. [DOI] [PubMed] [Google Scholar]
- 32.Harvey AG, Bryant RA. The relationship between acute stress disorder and posttraumatic stress disorder: a 2-year prospective evaluation. J Consult Clin Psychol. 1999;67:985–988. [DOI] [PubMed] [Google Scholar]
- 33.Bryant RA, Harvey AG. New DSM-IV diagnosis of acute stress disorder. Am J Psychiatry. 2000;157: 1889–1891. [DOI] [PubMed] [Google Scholar]
- 34.Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V. Nationwide longitudinal study of psychological responses to September 11. JAMA. 2002;288: 1235. [DOI] [PubMed] [Google Scholar]
- 35.Bryant RA, Harvey AG, Guthrie RM, Moulds ML. A prospective study of psychophysiological arousal, acute stress disorder, and posttraumatic stress disorder. J Abnorm Psychol. 2000;109:341–344. [PubMed] [Google Scholar]
- 36.Bryant RA, Harvey AG. Delayed-onset posttraumatic stress disorder: a prospective evaluation. Aust NZ J Psychiatry. 2002;36:205–209. [DOI] [PubMed] [Google Scholar]
- 37.North CS, Nixon SJ, Shariat S, et al. Psychiatric disorders among survivors of the Oklahoma City bombing. JAMA. 1999;282:755. [DOI] [PubMed] [Google Scholar]
- 38.McFarlane AC. Posttraumatic morbidity of a disaster: A study of cases presenting for psychiatric treatment. J Nerv Ment Dis. 1986;174:4. [DOI] [PubMed] [Google Scholar]
- 39.Smith EM, North CS, McCool RE, Shea JM. Acute postdisaster psychiatric disorders: identification of persons at risk. Am J Psychiatry. 1990;147:202–206. [DOI] [PubMed] [Google Scholar]
- 40.Maes M, Mylle J, Delmeire L, Altamura C. Psychiatric morbidity and comorbidity following accidental man-made traumatic events: incidence and risk factors. Eur Arch Psychiatry Clin Neurosci. 2000;250:156–162. [DOI] [PubMed] [Google Scholar]
- 41.Briere J, Elliott D. Prevalence, characteristics, and long-term sequelae of natural disaster exposure in the general population. J Traumatic Stress. 2000;13: 661–679. [DOI] [PubMed] [Google Scholar]
- 42.Fothergill A, Peek LA. Poverty and disasters in the United States: a review of recent sociological findings. Nat Hazards. 2004;32:89. [Google Scholar]
- 43.Rather R. 2006 South Louisiana Recovery Survey: citizen and civic leader research summary of findings. Baton Rouge, La; Louisiana Recovery Authority; 2006.
- 44.Resnick HS, Yehuda R, Pitman RK, Foy DW. Effect of previous trauma on acute plasma cortisol level following rape. Am J Psychiatry. 1995;152:1675–1677. [DOI] [PubMed] [Google Scholar]
- 45.Zaidi LY, Foy DW. Childhood abuse experiences and combat-related PTSD. J Trauma Stress. 1994;7: 33–42. [DOI] [PubMed] [Google Scholar]
- 46.Koopman C, Classen C, Spiegel D. Predictors of posttraumatic stress symptoms among survivors of the Oakland/Berkeley, Calif., firestorm. Am J Psychiatry. 1994;151:888–894. [DOI] [PubMed] [Google Scholar]
- 47.Washington Post/Kaiser Family Foundation/Harvard School of Public Health. Survey of Hurricane Katrina Evacuees. Available at: http://www.kff.org/newsmedia/7401.cfm. Accessed October 10, 2005.
- 48.de Jong J, Komproe I, van Ommeren M. Terrorism, human-made and natural disasters as a professional and ethical challenge to psychiatry. Int Psychiatry. 2003;1:8–9. [PMC free article] [PubMed] [Google Scholar]
- 49.Herman DB, Susser ES. The World Trade Center attack: mental health and treatment implications. Int Psychiatry. 2003;1:2–4. [PMC free article] [PubMed] [Google Scholar]
- 50.de Jong J. Public mental health and culture: Disasters as a challenge to Western mental health care models, the self, and PTSD. In: Wilson JP, Drozdek B, eds. Broken Spirits: The Treatment of Traumatized Asylum Seekers, Refugees, War and Torture Victims. New York, NY: Brunner-Routledge; 2004:159–178.
- 51.Almedom AM, Summerfield D. Mental well-being in settings of “complex emergency”: an overview. J Biosoc Sci. 2004;36:381–388. [DOI] [PubMed] [Google Scholar]
- 52.International UP. La. board OK’s post-Katrina health change. Available at: http://www.upi.com/HealthBusiness/view.php. Accessed June 19, 2006.
- 53.Kristof N. Medicine’s sticker shock. New York Times. October 2, 2005;4:13. [Google Scholar]
- 54.Koopman C, Classen C, Spiegel D. Multiple stressors following a disaster and dissociative symptoms. In: Fullerton CS, Ursono RJ, eds. Posttraumatic Stress Disorder: Acute and Long-Term Responses to Trauma and Disaster. Washington, DC: American Psychiatric Press; 1997:21–35.
- 55.Norris FH, Kaniasty K. Received and perceived social support in times of stress: a test of the social support deterioration deterrence model. J Pers Soc Psychol. 1996;71:498. [DOI] [PubMed] [Google Scholar]


