Abstract
An anthrax spore aerosol infection mouse model was developed as a first test of in vivo efficacy of antibiotics identified as active against Bacillus anthracis. Whole-body, 50% lethal dose (LD50) aerosol challenge doses in a range of 1.9 × 103 to 3.4 × 104 CFU with spores of the fully virulent Ames strain were established for three inbred and one outbred mouse strain (A/J, BALB/c, C57BL, and Swiss Webster). The BALB/c strain was further developed as a model for antibiotic efficacy. Time course microbiological examinations of tissue burdens in mice after challenge showed that spores could remain dormant in the lungs while vegetative cells disseminated to the mediastinal lymph nodes and then to the spleen, accompanied by bacteremia. For antibiotic efficacy studies, BALB/c mice were challenged with 50 to 100 LD50 of spores followed by intraperitoneal injection of either ciprofloxacin at 30 mg/kg of body weight (every 12 h [q12h]) or doxycycline at 40 mg/kg (q6h). A control group was treated with phosphate-buffered saline (PBS) q6h. Treatment was begun 24 h after challenge with groups of 10 mice for 14 or 21 days. The PBS-treated control mice all succumbed (10/10) to inhalation anthrax infection within 72 h. Sixty-day survival rates for ciprofloxacin and doxycycline-treated groups were 8/10 and 9/10, respectively, for 14-day treatment and 10/10 and 7/10 for 21-day treatment. Delayed treatment with ciprofloxacin initiated 36 and 48 h postexposure resulted in 80% survival and was statistically no different than early (24 h) postexposure treatment. Results using this mouse model correlate closely with clinical observations of inhalational anthrax in humans and with earlier antibiotic studies in the nonhuman primate inhalational anthrax model.
Bacillus anthracis, the causative agent of anthrax, is primarily a disease of animals. In humans, anthrax usually produces a fatal disease when introduced by inhalation or ingestion of spores (18). Of even greater concern is the potential use of this organism as a biological weapon, as demonstrated in the 2001 bioterrorism-related distribution of anthrax spores by the U.S. mail (8, 9, 35). While that event was limited in scope (with a total of 22 confirmed cases of anthrax, 11 cases of inhalational anthrax, and 5 fatalities), the outbreak pointed out both gaps and successes in the treatment and prophylaxis strategies. In New York City, an antibiotic prophylaxis strategy may have prevented an equal number of inhalational anthrax cases (3, 6). However, the ability to deal with this event might well have been overwhelmed if a larger-scale attack had occurred or the organism was resistant to the antibiotics of choice. The possibility of emerging natural resistance or “engineered” resistance remains an area of great concern (24). For example, although penicillin has long been considered the treatment of choice for anthrax, numerous reports of β-lactamase-producing strains and treatment failures have appeared in the literature (4, 14, 22, 27). Additionally, two open reading frames coding for β-lactamases in the B. anthracis genome have been identified (10, 29). More recently, several reports of B. anthracis resistance to ciprofloxacin, macrolides, and tetracyclines have appeared in the literature (5, 11, 36). It is therefore of great public interest to promote a sound strategy to deal with bioterrorism in general, and B. anthracis in particular, with the added concern for engineered antibiotic resistance. In a biological threat agent setting, it becomes important to assess the spectrum of antibiotics available for prophylaxis and treatment. An important element of such a preparedness strategy is the development of new treatments for individuals potentially exposed to B. anthracis spores. Traditional development of new anti-infection agents begins with an in vitro demonstration of antimicrobial activity and is followed by preclinical animal studies and then by clinical trials with humans. In the case of bioterrorism-related pathogens, ethical considerations and a relative paucity of naturally occurring infections preclude the conducting of controlled human studies.
At present, U.S. Food and Drug Administration (FDA) approval of a drug for use against B. anthracis and other biological warfare threat agents requires the demonstration of efficacy in one or more animal species (17). The current inhalation anthrax animal model for antibiotic testing is the rhesus monkey (19). This species is both expensive and in short supply. Also, this model is currently acceptable only for “postexposure” indications, not for treatment of active disease. The use of a small rodent model decreases the cost and increases the number of animals per test group as well as the number of antibiotics that can be tested at any given time. While no single animal model will yield data adequate for precise application to treatment of human disease, information from several well-defined infection models will allow a greater ability to assess the utility of a given antibiotic for treatment of humans. A small-animal rodent model could serve well in the FDA's “animal rule” testing structure.
Recent reports of small-animal models for anthrax have appeared in the literature. Many of these models have used subcutaneous challenges and have been used primarily for vaccine development studies (7, 25). Two recent reports did involve respiratory route challenges followed by antibiotic treatment, using a guinea pig intranasal challenge model (2) and an irradiated mouse intratracheal challenge model (16). The guinea pig model is limited due to the safety spectrum of antibiotics that can be tested in this model (32). Drawbacks of the irradiated mouse model are the compromised immune status of the animals and the use of an attenuated (capsule-minus) B. anthracis strain. The safety spectrum of antibiotics would also be of concern for any future rabbit model for efficacy against anthrax (32). The best-described model to date is an intranasal or intratracheal challenge mouse model utilizing spores of the fully virulent Ames strain of B. anthracis (28). While there are some small differences in dose and dissemination between the two challenge routes, similarities to human aerosolized infections were observed. The drawback is that neither the intranasal nor the intratracheal challenge route is truly representative of the inhalation of large numbers of spores, as would be expected in any attack. This aspect of the intranasal and intratracheal challenge models brings into question how deeply into the alveolar spaces anthrax spores would be delivered and how this affects dissemination of the vegetative organisms in terms of tissue destination and timing.
While the existing nonhuman primate (NHP) inhalational anthrax model includes an aerosol challenge with B. anthracis, there is a real need for a small-animal, aerosol challenge model with anthrax spores. In this study, we present data obtained from a mouse model (four strains of mice) challenged with fully virulent spores from the Ames strain of B. anthracis. We describe the progress of dissemination of anthrax infection after inhalational challenge in one mouse strain, and we evaluate the efficacy of antibiotic administration for postexposure prophylaxis and disease treatment.
MATERIALS AND METHODS
Bacillus anthracis and spore preparation.
Spores were prepared with the Ames strain of B. anthracis using the medium and growth conditions from Leighton and Doi (26) as described previously (39). Before aerosol challenge, spore preparations were heated at 65°C for 30 min and diluted in sterile water to final concentrations (37).
Bacteria were counted by serially diluting preparations or samples 1:10 in sterile water and plating the appropriate dilutions in triplicate on sheep blood agar plates (SBAP). Plates were incubated at 37°C for 18 h, and colonies were counted.
Aerosol infection.
Challenge aerosols were generated with Ames strain spores and a nebulizer (30). All aerosol procedures were controlled and monitored using the automated bioaerosol exposure system (23) operating with a whole-body rodent exposure chamber. Integrated air samples were obtained from the chamber during each exposure using an all-glass impinger. All-glass impinger samples were processed for aerosol concentration and inhaled dose calculations. Animals received whole-body aerosol exposures and were then observed, and mortality was recorded.
For 50% lethal dose (LD50) determinations, groups of 10 mice were exposed to increasing concentrations of spores by aerosol. Four mouse strains were used for LD50 studies: A/J, C57BL, BALB/c, and Swiss Webster. All mice were females, 6 to 8 weeks old, with an average weight of 20 g. For studies of disease history and antibiotic efficacy, BALB/c mice were challenged by aerosol with approximately 50 times the established LD50 of Ames spores.
For all experimental procedures described herein, the investigators adhered to the guidelines promulgated in the Guide for the Care and Use of Laboratory Animals (33). Our facilities are fully accredited by the American Association for Accreditation of Laboratory Animal Care.
Disease history.
The kinetics of dissemination of spores and vegetative organisms were determined after challenge by collecting blood and tissues at different time points. Six animals per time point were killed by exposure to CO2, and tissue bacterial burdens were determined as follows. Lungs, spleens, and mediastinum regions were aseptically removed, weighed, homogenized in 1 ml of sterile water, and then serially diluted 1:10 in sterile water; 100-μl aliquots were then plated on SBAP. Blood was also collected from the mice and plated to determine the timing of the bacteremia. To determine if anthrax spores were present, aliquots of the tissue homogenates were “heat shocked” for 30 min at 65°C (to kill vegetative organisms but not spores) (37), serially diluted, and plated as described above. SBAP were incubated at 37°C for 18 h, colonies were counted, and counts were standardized to tissue weight.
Pathology.
Three mice per time point from the disease history study were euthanized and necropsied for pathology evaluation. Additionally, dead or euthanized animals from other portions of the studies were separately evaluated. Tissue samples from all major organs/tissues were fixed in 10% neutral buffered formalin, processed, embedded in paraffin, and sectioned (5- to 6-μm-thick sections) for hematoxylin and eosin staining as previously described (40).
Antibiotics.
Intravenous preparations of ciprofloxacin (Bayer, West Haven, CT) and doxycycline (Bedford Labs, Bedford, OH) were reconstituted according to the manufacturers' instructions. Final concentrations were adjusted to provide the desired dose in a volume of 0.2 ml. Both antibiotics and physiological saline were administered intraperitoneally (i.p.).
Antibiotic efficacy.
Postexposure prophylactic antibiotic treatment was initiated 24 h after challenge. Female BALB/c mice in groups of 10 were given doses of ciprofloxacin (30 mg/kg of body weight every 12 h [q12h]), or doxycycline (40 mg/kg q6h) by i.p. injection in a volume of 0.2 ml. Antibiotic groups received treatments for either 14 or 21 days. Control mice received i.p. injections of phosphate-buffered saline (PBS; 0.2 ml q6h). Animals were observed, and mortality was recorded. Surviving mice from each group were euthanized at day 60 postchallenge (46 to 39 days posttreatment), and bacterial and spore burdens were determined for lungs, spleens, and mediastinal regions as described above.
Results of disease treatments were compared to those of prophylaxis experiments by delaying the initial treatment to 36 and 48 h postchallenge based on the disease history findings of onset of bacteremia and organ spread. Doses and schedules were the same as described above for 21 days.
Antibiotic susceptibilities of recovered B. anthracis isolates were determined according to CLSI (formerly NCCLS) methods by microdilution broth assay (31, 34).
Antibiotic pharmacokinetics.
To determine doses for treatments, antibiotics were administered i.p. to three groups of BALB/c mice. Each group was given a single dose of 25, 50, or 100 mg/kg of the antibiotic. Three mice in each dose group were terminally bled after being subjected to deep anesthesia with ketamine, xylazine, and acetylpromazine solution at 30 min, 1 h, 2 h, 4 h, 6 h, and 12 h. The serum antibiotic concentrations were determined according to a modified bioassay using Staphylococcus aureus ATCC 29213 as the indicator organism and compared to a standard curve for that antibiotic in control mouse serum (15). The upper and lower limits of detection were 64 and 0.12 μg/ml, respectively, for ciprofloxacin and 64 and 0.25 μg/ml for doxycycline. The assay variability at the lower limit was plus or minus one twofold dilution. Area under the curve (AUC) for ciprofloxacin and AUC and time above the MIC for doxycycline were used as the criteria for animal dosing after anthrax challenge (12).
Statistical analysis.
LD50 analysis was performed by probit analysis with step-down Bonferroni's correction. Antibiotic efficacy was evaluated by Kaplan-Meier and log rank analysis (Mantel-Haenszel test) using the GraphPad Prism statistics program (version 4.0b; GraphPad Software Inc., San Diego, CA).
RESULTS
The LD50 for the four mouse strains were determined by a probit analysis with step-down Bonferroni's correction for post hoc pairwise comparisons and are shown in Table 1.
TABLE 1.
Ames spore aerosol LD50a
| Strain | Dose
|
MTD (h) | ||
|---|---|---|---|---|
| LD50 (CFU) | Lower 95% limit | Upper 95% limit | ||
| A/J | 1,908 | 948 | 3,687 | 51.8 |
| BALB/c | 34,209 | 16,593 | 63,248 | 78.5 |
| C57BL | 28,153 | ND | ND | 69.6 |
| Swiss Webster | 7,878 | 1,033 | 29,957 | 63.8 |
The MTD was calculated from all deaths in the LD50 study. ND, not determined.
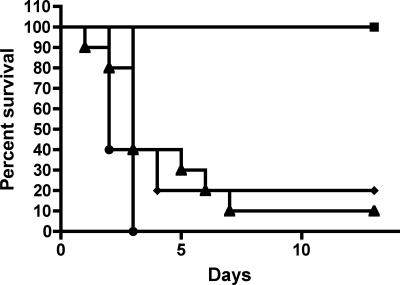
Results of probit analysis showed a significant difference in LD50 between the four strains [χ2(3) = 21.02; P = 0.0001]. Subsequent pairwise probit analyses showed significant differences when results for A/J mice were compared with those for BALB/c mice (P = 0.0006) and when results for A/J mice were compared with those for C57BL mice (P = 0.0125). The difference seen in a comparison between results for BALB/c and Swiss Webster mice was nearly significant (P = 0.0520). No other pairwise comparisons showed statistically significant differences. Figure 1 shows representative Kaplan-Meier plots of the LD50 determinations for the BALB/c mice.
FIG. 1.
Kaplan-Meier survival curves for BALB/c LD50 determination after challenge with escalating doses of B. anthracis (Ames) spores by aerosol. Doses were for “whole body” and expressed as spores/animal. ▪, 2.3 × 102; ♦, 3.7 × 104; ▴, 5.9 × 105; •, 3.7 × 106.
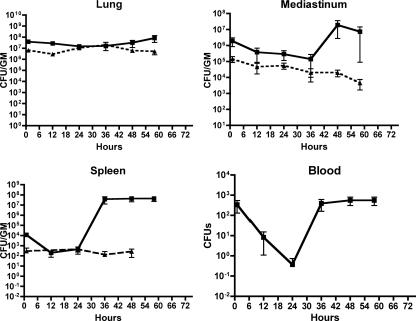
BALB/c mice were further evaluated for the progression of disease and antibiotic treatment with whole-body exposure with spores from the Ames strain of B. anthracis. For lethal doses of anthrax spores, animals were challenged with 50 LD50 using the calculated LD50 (3.4 × 104 CFU/mouse) for this strain. The progression and distribution of vegetative organisms and spores after challenge are shown in Fig. 2. After aerosol challenge with lethal doses of spores, organisms were cultured from the lungs. These organisms were heat shock resistant, indicating that they were ungerminated spores. Between 36 and 48 h into the infection, vegetative organisms appeared in the mediastinum and spleen. Bacteremia was observed as an initial spike followed by a rapid drop off, and it rapidly rose again at 36 h and continued until the mice succumbed (60 to 72 h).
FIG. 2.
Bacterial load disease history of B. anthracis (Ames) in mouse tissues after aerosol challenge. Tissues were collected from BALB/c mice at different time points post-anthrax aerosol challenge (n = 6). ▪, total CFU; ▴, spores. GM, gram of tissue.
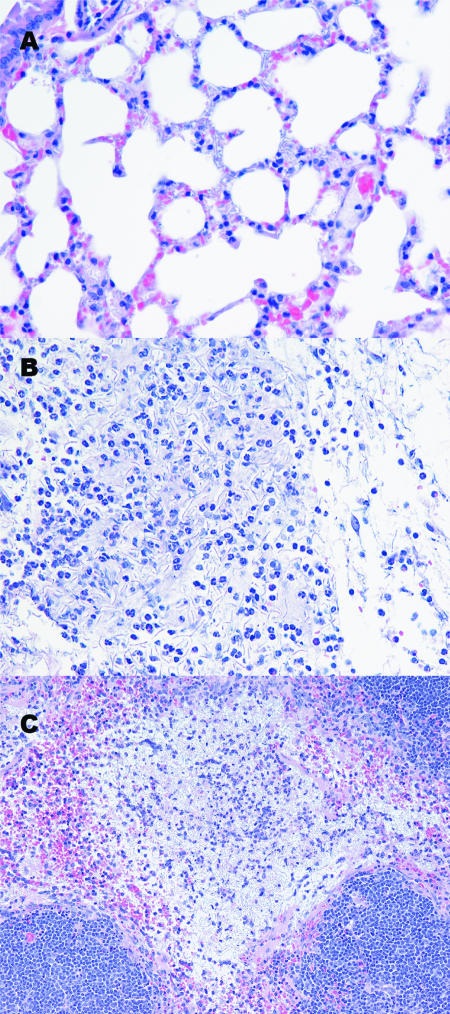
Histopathological changes resulting from anthrax infection were present in all untreated and PBS-treated BALB/c mice. The most common changes were the presence of bacteria in a variety of organs, most notably in alveolar septal capillaries (Fig. 3A), in renal glomerular capillaries, and in hepatic sinusoids. Less commonly found were focally extensive areas of mediastinitis, usually characterized by mild infiltration of polymorphonuclear leukocytes (PMN) and fewer macrophages and lymphocytes (Fig. 3B). These sites of inflammation often, but not always, had bacilli present in various numbers. Approximately one-third of the mice examined had splenic lesions, consisting of myriad bacilli, rarely with accompanying mild infiltrates of PMN, in the red pulp. In the splenic white pulp, there was occasionally moderate lymphoid depletion (Fig. 3C). Finally, in the liver of one mouse, there were multiple foci of hepatocellular degeneration and necrosis (ischemia) with associated tight clusters of bacilli plugging the sinusoids.
FIG. 3.
Hematoxylin and eosin stain of tissues from a female BALB/c mouse aerosol exposed to approximately 50 LD50 of B. anthracis Ames spores, 48 h postexposure. (A) Lung; magnification, ×40. The clear spaces of the alveoli are delimited by alveolar septa, and numerous red blood cells can be seen within the septal capillaries. Also within the capillaries are many anthrax bacilli, usually seen in longitudinal section but also in cross section as small blue dots. (B) Mediastinum; magnification, ×40. In this field, there is a mild pyogranulomatous inflammatory cell infiltrate consisting of PMN and macrophages. Also note the numerous anthrax bacilli in the background. (C) Spleen; magnification, ×20. Centrally within this field, within the splenic red pulp, is a large pale zone consisting mostly of myriad anthrax bacilli. Also in this area is a mild inflammatory cell infiltrate of PMN and macrophages, and many of these cells are necrotic. Bordering this zone, to the bottom and upper right corner, the compacted nuclei of splenic white pulp are evident. Free red blood cells present in the outermost areas of the white pulp (marginal zone) are most likely evidence of mild hemorrhage.
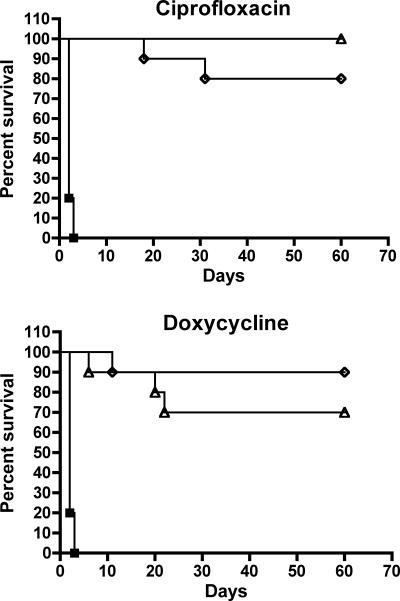
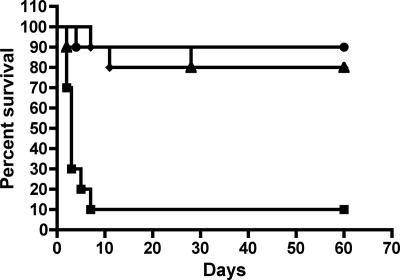
To determine if this infection model was suitable for the evaluation of antibiotic efficacy, we tested ciprofloxacin and doxycycline. These antibiotics have in vitro activity against B. anthracis (MICs for the Ames strain were 0.25 μg/ml [ciprofloxacin] and 0.03 μg/ml [doxycycline]) and demonstrated efficacy in both NHP and humans (9, 19). The final antibiotic doses and schedule were based on the pharmacokinetic data summarized in Table 2 and were those needed to achieve a daily AUC/MIC ratio of 100 for ciprofloxacin and an AUC of greater than 100 with a prolonged time above the MIC for doxycycline (12). As seen in Fig. 4, results of 14- and 21-day treatments with ciprofloxacin were not significantly different from those with doxycycline, but significantly improved survival compared to untreated controls (P < 0.0001) was demonstrated with both treatments. This result was further supported by our inability to culture organisms from the blood, mediastinum, and spleens of the treated surviving animals 60 days postchallenge. Culture results at 60 days, when positive, showed single to a few colonies, and these could be observed only in the lung samples. While there was no significant difference between results of 14- and 21-day treatments, it should be noted that a few deaths did occur among the 14-day groups shortly after the last treatment for both antibiotics. Some additional late deaths occurred in the 21-day doxycycline group but not in the 21-day ciprofloxacin group. Gross pathology of the animals in the 21-day doxycycline group that died or were euthanized during treatment indicated that peritonitis was present, most likely due to this antibiotic. This was previously observed with prolonged i.p. doxycycline treatments. Susceptibility testing of the isolates from the ciprofloxacin and the doxycycline 14- and 21-day treatment groups yielded MICs similar (within one to two dilutions) to those for the original Ames strain, indicating that these isolates were most likely due to residual spores.
TABLE 2.
Pharmacokinetic parameters
| Antibiotic and dose (mg/kg) | Cmax (μg/ml)a | AUC (0 to 6 h; μg·h/ml) | Trough (6 h; μg/ml) |
|---|---|---|---|
| Ciprofloxacin | |||
| 25 | 6.6 | 6.6 | 1 |
| 50 | 10.7 | 14.1 | 1.83 |
| 100 | 20 | 37.7 | 1.67 |
| Doxycycline | |||
| 25 | 4 | 13.7 | 1.33 |
| 50 | 6.7 | 23.4 | 1.67 |
| 100 | 12 | 57.2 | 6 |
Cmax, maximum concentration of drug in serum.
FIG. 4.
Postexposure antibiotic prophylaxis. Treatment was initiated 24 h after challenge. Female BALB/c mice received ciprofloxacin at 30 mg/kg q12h or doxycycline at 40 mg/kg q6h, and control mice received PBS q6h. Ciprofloxacin and doxycycline treatments significantly improved survival compared to untreated controls (P < 0.0001). ▪, control; ⋄, 14-day treatment; ▵, 21-day treatment.
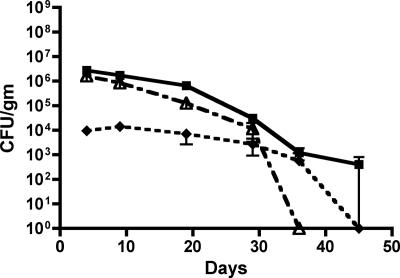
A follow-up experiment for the disease history study evaluated bacterial loads in tissues throughout a 21-day ciprofloxacin treatment and posttreatment. Figure 5 shows that heat-resistant B. anthracis remains in the lung tissue for a prolonged period, beyond the 14- and 21-day treatments, indicating that spores were still present. No organisms were cultured from the blood or spleens at any time point in this experiment.
FIG. 5.
Bacterial loads in tissues throughout ciprofloxacin treatment and posttreatment. Tissues were collected from BALB/c mice at different time points post-anthrax aerosol challenge and throughout a 21-day ciprofloxacin treatment and posttreatment phase. Heat-resistant B. anthracis was cultured from the lung tissue for a prolonged period beyond the treatment phase of 21 days, indicating that spores were still present. Blood or spleen samples were negative for colony growth in this experiment (n = 3). ♦, mediastinum; ▪, lung; ▵, lung spores.
The survival of animals after challenge with a delayed treatment, to correspond to a point where anthrax had begun to disseminate into the blood and tissues, is shown in Fig. 6. Ciprofloxacin treatment started at either 36 or 48 h postchallenge was still able to successfully treat animals compared to the control (P was <0.001 or <0.0002, respectively).
FIG. 6.
Disease treatment by delay of treatment. Female BALB/c mice were given 30 mg/kg doses of ciprofloxacin q12h, and control mice received injections of PBS q12h for 21 days. Disease treatment compared to prophylaxis was performed by delaying the initial treatment to 36 and 48 h postchallenge. By 36 h (P < 0.001) or 48 h (P < 0.0002), mice in the postchallenge groups survived significantly longer than those in the control group. ▪, control; ♦, ciprofloxacin group 24 h postexposure; ▴, ciprofloxacin group 36 h PE; •, ciprofloxacin group 48 h postexposure.
DISCUSSION
Due to the difficulty of developing reliable therapeutic regimens directed against agents of bioterrorism, such as B. anthracis, the FDA has provided draft guidance (17, 38) regarding demonstration of the effectiveness of a drug or therapy by recommending the use of the rhesus monkey as a disease and treatment model for inhalational anthrax (postexposure), as described by Friedlander et al. (19) for ciprofloxacin, doxycycline, and penicillin G. While the rhesus monkey model is arguably the best animal model for the final evaluation of drugs for use against B. anthracis, the expense and number of animals required to screen new drugs probably precludes the use of this animal. Thus, only in vitro data, the results from different animal species studies, and the pharmacokinetics of the drugs of interest in humans can be applied to the identifying doses and administration schedules that would provide effective therapy to individuals naturally or intentionally exposed to such agents. A small-animal model, such as the mouse model, would fill that “gap” in efficacy testing.
The three inbred mouse strains tested in this study were chosen based on their susceptibility differences as previously observed with a subcutaneous B. anthracis challenge (39). Note that, in addition to the different challenge route, a slightly less virulent B. anthracis strain, Vollum 1B, was used in those studies and may account for some of the sensitivity differences. Clearly, the A/J mouse strain is more sensitive and has a shorter mean time to death (MTD) than BALB/c and C57BL mouse strains. These data are similar to the observations of Lyons et al. (28), who studied an intranasal challenge model. Adding the outbred Swiss Webster stock provided a slightly intermediate pattern that is between those for the A/J and BALB/c and C57BL mouse strains.
The disease history reported here for inhalational anthrax was significantly different than those in previous reports of intranasal and intratracheal mouse anthrax models (28). This may be due to several factors. First is the fact that for the intranasal and intratracheal challenges, spores are introduced as a liquid suspension versus the drier single-spore aerosol. This in turn may affect how deep into the lungs each challenge method is able to distribute the organism. Aerosols are expected to deliver spores deeper and in larger numbers to the alveoli, while the intranasal and intratracheal routes most likely deposit the majority of spores at the level of the bronchioles where there may be increased germination (28). This is in stark contrast to the aerosol model where, clearly, spores remain dormant in the lung tissue. The number of dormant spores found in the lungs in our mouse studies is consistent with published NHP data and human cases. This is why a long duration of antibiotic treatment is required, until the number of spores is reduced to the point that germination does not result in disease or immunity is secured via vaccination. This difference may be due to the fact that, for the intranasal and intratracheal models, the spores are introduced as a liquid suspension that results in an environment that would promote germination (R. Lyons, personal communication). The other possibility is that the observation of germinated bacteria may simply be a reseeding via the capillary bed from the emerging bacteremia. This possibility can be seen in the small rise in heat-sensitive bacterial counts in the 48- and 60-hour lung tissue loads as observed in Fig. 2. The fact that germination in the lung tissue was a relatively minor event is further supported by observation of the slow decline of heat-resistant organisms in the lungs under ciprofloxacin treatment (Fig. 5). This observation, as well as the movement of organisms from lung to mediastinum and spleen with a delayed bacteremia, as shown in Fig. 2, is consistent with observations of human inhalational anthrax.
The results of the histopathological examination of both untreated and PBS-treated BALB/c mice generally corroborated the culture data from this study and indicate that this mouse strain was uniformly infected by whole-body aerosol exposure to a lethal dose of B. anthracis.
In many respects, our findings agree with those of Lyons et al. (28) with regard to many of the histopathological changes present in most affected tissues. However, those authors describe pulmonary lesions in their mice after either intranasal or intratracheal instillation of the infectious inoculum. With the exception of the perivascular inflammation associated with large pulmonary vessels in a few mice, the pulmonary lesions they found consisted of distension of alveolar septal capillaries with bacilli, minimal to no parenchymal inflammation, and some very subtle changes in the bronchiolar epithelium. In contrast, we considered the presence of bacilli within alveolar (or glomerular) capillaries to be bacteremia until the bacilli emerged from the capillaries, eliciting a host cell response. With regard to the pulmonary parenchymal changes alluded to by Lyons et al. (28), we have found, after examining the mice in this study and many hundreds of other mice exposed by whole-body aerosol to lethal doses of B. anthracis, that true pulmonary lesions in the mouse are exceedingly rare. This is also the finding for human inhalational anthrax. Likewise, the pathological changes in the bronchiolar epithelium described by Lyons et al. (28) are changes we failed to observe in mice exposed to whole-body aerosol. We speculate that the bronchiolar epithelial changes described by Lyons et al. may have resulted from the liquid medium they used in their inocula alone or in combination with the organism.
The lack of true pulmonary lesions in the mouse does not detract from its similarities to other species with regard to anthrax-induced histopathological changes. In a retrospective study of inhalation anthrax in the rhesus monkey (20), a very low incidence of pulmonary lesions was observed, and the majority of those lesions were due to bacilli breaking out of alveolar septal capillaries (secondary pulmonary lesions). In contrast, Gleiser et al. (21), in a similar study in 1963, found a much higher incidence of pulmonary lesions in the monkeys in their study. Unlike the monkeys in the retrospective study, most if not all of the monkeys in the study by Gleiser et al. had lung mite (Pneumonyssus simicola) nodules (small granulomas). Those authors believed that the pulmonary lesions represented sites where lung mite nodules had been superinfected by B. anthracis and therefore were primary pulmonary lesions.
Because of the whole-body exposure of anthrax spores in these studies and particularly because of the fastidious preening exhibited by mice, we were especially vigilant for evidence of primary (by ingestion) gastrointestinal infection in these animals. There was no evidence of this. Findings in previous studies of NHPs and reviews of human cases of inhalational anthrax (20) suggest that primates exhibit resistance to primary gastrointestinal infection. Our findings in this study, coupled with experience in examining many whole-body-exposed mice, suggest that mice are similarly resistant.
In one of the most complete presentations of human inhalational anthrax, Abramova et al. (1) reported autopsy findings in 42 patients who succumbed to inhalational anthrax after an accidental release of anthrax spores in Sverdlovsk (former Soviet Union) in 1979. These authors found focal primary pulmonary anthrax lesions in 11/42 cases, and each of these was associated with a Ghon (preexisting tuberculous) focus. There are, therefore, indications in anthrax studies of species other than mice that pulmonary lesions are not a common finding unless there is preexisting pulmonary disease.
The BALB/c mouse strain was evaluated as the antibiotic efficacy model for several reasons. This strain had a consistently achievable lethal dose in the aerosol system and a mean time to death amenable to both postexposure prophylaxis and disease treatment studies as observed in the history study. In this model, ciprofloxacin and doxycycline were able to protect animals both postexposure and when B. anthracis had begun to spread significantly in the blood and tissues, at 36 and 48 h postchallenge, respectively. Ciprofloxacin and doxycycline are both drugs for which efficacy is associated with the AUC. In the case of B. anthracis and the spore population, there may also be a time above MIC (Δt/MIC) component (13). This could be due in part to the fact that the spore population, being metabolically inactive, is never exposed to the AUC and instead may germinate between treatments at antibiotic levels near or below the MIC. This, in turn, could result in the selection of resistance, especially where there is a greater time between doses. Note that there were some deaths when the treatment was stopped at 14 days and that bacterial isolates from these animals had slightly elevated MICs. In addition, for the 14-day treatments, there were more posttreatment deaths in the ciprofloxacin group (q12h) than in the doxycycline group (q6h). While there was no statistical significance between 14 and 21 days of treatment (P was 0.2907 for doxycycline and 0.1464 for ciprofloxacin), we consistently observed deaths with the termination of treatment in subsequent experiments. This postexposure treatment survival/failure seems to correlate with a spore load in the lungs of 104 CFU/g of tissue (Fig. 5). We presume that above this level, a sufficient number of spores to achieve infection is maintained and that once the spore level drops, the immune system is able to provide sufficient protection to prevent disseminated disease. The post-14-day treatment deaths and the lung spore load data we observed with ciprofloxacin treatment verify the need for extended antibiotic courses to ensure near-100% protection rates for prophylaxis. Data for both ciprofloxacin and doxycycline closely match those observed previously with the NHP model (19).
The anthrax aerosol mouse model has many characteristics in common with human inhalational anthrax, but there are also differences. No animal model will perfectly match the human course of any disease, but a combination of models may answer many of the questions. In the case of disease such as inhalational anthrax and other potential biothreat agents, animal models will continue to be our only means of assessing therapies and vaccines. This mouse model was developed to serve as such a screening tool and was recently extended to explore pharmacokinetic and pharmacodynamic parameters for fluoroquinolones as it relates to NHP and human dosing in anthrax treatment (13).
Acknowledgments
The opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the U.S. Army.
The research described herein was sponsored by the Defense Threat Reduction Agency, project no. 02-4-2C-013.
Footnotes
Published ahead of print on 12 February 2007.
REFERENCES
- 1.Abramova, F. A., L. M. Grinberg, O. V. Yampolskaya, and D. H. Walker. 1993. Pathology of inhalational anthrax in 42 cases from the Sverdlovsk outbreak of 1979. Proc. Natl. Acad. Sci. USA 90:2291-2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Altboum, Z., Y. Gozes, A. Barnea, A. Pass, M. White, and D. Kobiler. 2002. Postexposure prophylaxis against anthrax: evaluation of various treatment regimens in intranasally infected guinea pigs. Infect. Immun. 70:6231-6241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blank, S., L. C. Moskin, and J. R. Zucker. 2003. An ounce of prevention is a ton of work: mass antibiotic prophylaxis for anthrax, New York City, 2001. Emerg. Infect. Dis. 9:615-622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bradaric, N., and V. Punda-Polic. 1992. Cutaneous anthrax due to penicillin-resistant Bacillus anthracis transmitted by an insect bite. Lancet 340:306-307. [DOI] [PubMed] [Google Scholar]
- 5.Brook, I., T. B. Elliott, H. I. Pryor II, T. E. Sautter, B. T. Gnade, J. H. Thakar, and G. B. Knudson. 2001. In vitro resistance of Bacillus anthracis Sterne to doxycycline, macrolides and quinolones. Int. J. Antimicrob. Agents 18:559-562. [DOI] [PubMed] [Google Scholar]
- 6.Brookmeyer, R., and N. Blades. 2002. Prevention of inhalational anthrax in the U.S. outbreak. Science 295:1861. [DOI] [PubMed] [Google Scholar]
- 7.Brossier, F., M. Levy, and M. Mock. 2002. Anthrax spores make an essential contribution to vaccine efficacy. Infect. Immun. 70:661-664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. 2001. Update: investigation of anthrax associated with intentional exposure and interim public health guidelines. Morb. Mortal. Wkly. Rep. 50:889-897. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. 2001. Investigation of bioterrorism-related anthrax and interim guidelines for exposure management and antimicrobial therapy. Morb. Mortal. Wkly. Rep. 50:909-919. [PubMed] [Google Scholar]
- 10.Chen, Y., F. C. Tenover, and T. M. Koehler. 2004. β-Lactamase gene expression in a penicillin-resistant Bacillus anthracis strain. Antimicrob. Agents Chemother. 48:4873-4877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choe, C., S. Bouhaouala, I. Brook, T. Elliott, and G. Knudson. 2000. In vitro development of resistance to ofloxacin and doxycycline in Bacillus anthracis Sterne. Antimicrob. Agents Chemother. 44:1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Craig, W. A. 2002. Pharmacodynamics of antimicrobials: general concepts and applications, p. 1-22. In C. H. Nightingale, T. Murakawa, and P. G. Ambrose (ed.), Antimicrobial pharmacodynamics in theory and clinical practice. Marcel Dekker, Inc., New York, NY.
- 13.Deziel, M. R., H. Heine, A., Louie, M. Kao, W. R. Byrne, J. Basset, L. Miller, K. Bush, M. Kelly, and G. L. Drusano. 2005. Effective antimicrobial regimens for use in humans for therapy of Bacillus anthracis infections and postexposure prophylaxis. Antimicrob. Agents Chemother. 49:5099-5106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doganay, M., and N. Aydin. 1991. Antimicrobial susceptibility of Bacillus anthracis. Scand. J. Infect. Dis. 23:333-335. [DOI] [PubMed] [Google Scholar]
- 15.Edberg, S. C. 1986. The measurement of antibiotics in human body fluids: techniques and significance, p. 382-399. In V. Lorian (ed.), Antibiotics in laboratory medicine, 2nd ed. Williams and Wilkins, Baltimore, MD.
- 16.Elliott, T. B., I. Brook, R. A. Harding, S. S. Bouhaouala, M. O. Shoemaker, and G. B. Knudson. 2002. Antimicrobial therapy for Bacillus anthracis-induced polymicrobial infection in 60Co γ-irradiated mice. Antimicrob. Agents Chemother. 46:3463-3471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Federal Register. 2002. New drug and biological drug products; evidence needed to demonstrate effectiveness of new drugs when human efficacy studies are not ethical or feasible. Fed. Regist. 67:37988-37998. [PubMed] [Google Scholar]
- 18.Friedlander, A. M. 2000. Anthrax: clinical features, pathogenesis, and potential biological warfare threat. Curr. Clin. Top. Infect. Dis. 20:335. [PubMed] [Google Scholar]
- 19.Friedlander, A. M., S. L. Welkos, M. L. M. Pitt, J. W. Ezzell, P. L. Worsham, K. J. Rose, B. E. Ivins, J. R. Lowe, G. B. Howe, P. Mikesell, and W. B. Lawrence. 1993. Postexposure prophylaxis against experimental inhalation anthrax. J. Infect. Dis. 167:1239-1242. [DOI] [PubMed] [Google Scholar]
- 20.Fritz, D. L., N. K. Jaax, W. B. Lawrence, K. J. Davis, M. L. M. Pitt, J. W. Ezzell, and A. M. Friedlander. 1995. Pathology of experimental inhalation anthrax in the rhesus monkey. Lab. Investig. 73:691-702. [PubMed] [Google Scholar]
- 21.Gleiser, C. A., C. C. Berdjis, H. A. Hartman, and W. S. Gochenour. 1963. Pathology of experimental respiratory anthrax in Macaca mulatta. Br. J. Exp. Pathol. 44:416-426. [PMC free article] [PubMed] [Google Scholar]
- 22.Gold, H. 1955. Anthrax: a report of one hundred seventeen cases. Arch. Intern. Med. 96:387-396. [DOI] [PubMed] [Google Scholar]
- 23.Hartings, J. M., and C. J. Roy. 2004. The automated bioaerosol exposure system: preclinical platform development and a respiratory dosimetry application with nonhuman primates. J. Pharmacol. Toxicol. Meth. 49:39-55. [DOI] [PubMed] [Google Scholar]
- 24.Inglesby, T. V., T. O'Toole, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. M. Friedlander, J. Gerberding, J. Hauer, J. Hughes, J. McDade, M. T. Osterholm, G. Parker, T. M. Perl, P. K. Russell, and K. Tonat. 2002. Anthrax as a biological weapon, 2002: updated recommendations for management. JAMA 287:2236-2252. [DOI] [PubMed] [Google Scholar]
- 25.Ivins, B. E., S. L. Welkos, G. B. Knudson, and S. F. Little. 1990. Immunization against anthrax with aromatic compound-dependent (Aro−) mutants of Bacillus anthracis and with recombinant strains of Bacillus subtilis that produce anthrax protective antigen. Infect. Immun. 58:303-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leighton, T. J., and R. H. Doi. 1971. The stability of messenger ribonucleic acid during sporulation in Bacillus anthracis. J. Biol. Chem. 246:3189-3195. [PubMed] [Google Scholar]
- 27.Lightfoot, N. F., R. J. D. Scott, and P. C. B. Turnbull. 1990. Antimicrobial susceptibility of Bacillus anthracis. Salisbury Med. Bull. 68(Suppl.):95-98. [Google Scholar]
- 28.Lyons, C. R., J. Lovchik, J. Hutt, M. F. Lipscomb, E. Wang, S. Heninger, L. Berliba, and K. Garrison. 2004. Murine pulmonary anthrax: kinetics of dissemination, histopathology, and mouse strain susceptibility. Infect. Immun. 72:4801-4809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Materon, I. C., M. Queenan, T. M. Koehler, K. Bush, and T. Palzkill. 2003. Biochemical characterization of β-lactamases Bla1 and Bla2 from Bacillus anthracis. Antimicrob. Agents Chemother. 47:2040-2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.May, K. R. 1973. The Collison nebulizer: description, performance and applications. J. Aerosol Sci. 4:235-243. [Google Scholar]
- 31.Mohammed, M. J., C. K. Marston, T. Popovic, R. S. Weyant, and F. C. Tenover. 2002. Antimicrobial susceptibility of Bacillus anthracis: comparison of results obtained by using the National Committee for Clinical Laboratory Standards broth microdilution reference and Etest agar gradient diffusion methods. J. Clin. Microbiol. 40:1902-1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morris, T. H. 1995. Antibiotic therapeutics in laboratory animals. Lab. Anim. 29:16-36. [DOI] [PubMed] [Google Scholar]
- 33.National Research Council. 1996. Guide for the care and use of laboratory animals. National Academy Press, Washington, DC.
- 34.NCCLS/CLSI. 2006. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 7th ed., vol. 23, no. 2. Approved standard M7-A7. NCCLS/CLSI, Wayne, PA.
- 35.Pile, J. C., J. D. Malone, E. M. Eitzen, and A. M. Friedlander. 1998. Anthrax as a potential biological warfare agent. Arch. Intern. Med. 158:429-434. [DOI] [PubMed] [Google Scholar]
- 36.Price, L. B., A. Volger, T. Pearson, J. D. Busch, J. M. Schupp, and P. Keim. 2003. In vitro selection and characterization of Bacillus anthracis mutants with high-level resistance to ciprofloxacin. Antimicrob. Agents Chemother. 47:2362-2365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Russell, A. D. 1982. The destruction of bacterial spores, p. 30-77. Academic Press, New York, NY.
- 38.U.S. Food and Drug Administration. 2002. Draft guidance for industry, inhalational anthrax (post-exposure)—development of antimicrobial drugs. CDER, U.S. Food and Drug Administration, Washington, DC.
- 39.Welkos, S. L., T. J. Keener, and P. H. Gibbs. 1986. Differences in susceptibility of inbred mice to Bacillus anthracis. Infect. Immun. 51:795-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zaucha, G. M., L. M. Pitt, J. Estep, B. E. Ivins, and A. M. Friedlander. 1998. The pathology of experimental anthrax in rabbits exposed by inhalation and subcutaneous inoculation. Arch. Pathol. Lab. Med. 122:982-992. [PubMed] [Google Scholar]