Abstract
Mycobacterium leprae, the causative agent of leprosy, is noncultivable in vitro; therefore, evaluation of antibiotic activity against M. leprae relies mainly upon the mouse footpad system, which requires at least 12 months before the results become available. We have developed an in vitro assay for studying the activities of quinolones against the DNA gyrase of M. leprae. We overexpressed in Escherichia coli the M. leprae GyrA and GyrB subunits separately as His-tagged proteins by using a pET plasmid carrying the gyrA and gyrB genes. The soluble 97.5-kDa GyrA and 74.5-kDa GyrB subunits were purified by nickel chelate chromatography and were reconstituted as an enzyme with DNA supercoiling activity. Based on the drug concentrations that inhibited DNA supercoiling by 50% or that induced DNA cleavage by 25%, the 13 quinolones tested clustered into three groups. Analysis of the quinolone structure-activity relationship demonstrates that the most active quinolones against M. leprae DNA gyrase share the following structural features: a substituted carbon at position 8, a cyclopropyl substituent at N-1, a fluorine at C-6, and a substituent ring at C-7. We conclude that the assays based on DNA supercoiling inhibition and drug-induced DNA cleavage on purified M. leprae DNA gyrase are rapid, efficient, and safe methods for the screening of quinolone derivatives with potential in vivo activities against M. leprae.
Leprosy is a chronic infectious disease which may cause severe disabilities due to damage of the peripheral nerves (29). Since the 1980s, tremendous progress has been made in controlling the disease by intensive implementation of multidrug therapy (MDT); nevertheless, the latest data indicate that about 300,000 new cases of leprosy are still detected every year, mostly in Asia, Latin America, and Africa (35).
By the end of the 1970s, due to long-term monotherapy, dapsone resistance had become a widespread phenomenon (20). In 1981, the World Health Organization introduced MDT, which was composed of rifampin, dapsone, and clofazimine (34). Although the duration of MDT has been reduced to 6 and 12 months for patients with paucibacillary and multibacillary leprosy, respectively, (36), the durations remain too long, and these treatment durations cause a number of operational difficulties, particularly for the direct supervision of drug administration by the patients. Also due to operational reasons, MDT did not completely prevent the emergence of drug resistance; by the end of 1990s, a few multidrug-resistant isolates of Mycobacterium leprae began to occur (5, 24, 25). In order to shorten the duration of MDT treatment, new antimicrobial agents with powerful bactericidal activities against M. leprae must be incorporated into the MDT regimens to significantly improve their efficacies. Within the last 20 years, a number of newer antimicrobial agents, such as the quinolones (e.g., pefloxacin, ofloxacin, sparfloxacin, and moxifloxacin), the macrolides (e.g., clarithromycin), and the tetracyclines (e.g., minocycline), that possess various degrees of bactericidal activity against M. leprae have been identified in mouse experiments and in human trials (18, 19). Among these newer antimicrobial agents, moxifloxacin has been demonstrated to display very powerful bactericidal activity against M. leprae (8) that is virtually identical to that of rifampin (the key component of the current MDT regimens) and has been well tolerated in human trials (26). Therefore, moxifloxacin may become an important component of a future MDT regimen. Because many quinolone derivatives are synthesized every year, it would be possible to identify quinolones with anti-M. leprae activities more potent than that of moxifloxacin if screening for new derivatives for their activities against M. leprae were to continue.
Because M. leprae, the causative agent of leprosy, is noncultivable in vitro, despite a hundred years of efforts (29), the only way to cultivate the leprosy bacillus is through the use of the mouse footpad system (22, 31), which remains the main system used to test the activities of antimicrobial agents against M. leprae. Since M. leprae has the longest doubling time (≈14 days) of all known bacteria, the mouse experiment is time-consuming and requires at least 12 months before the results become available. Therefore, it would be highly desirable to develop an in vitro method which would greatly accelerate progress in identifying more potent quinolones for their activities against M. leprae.
The targets of quinolones are type 2 topoisomerases, which consist of DNA gyrase and topoisomerase IV. These enzymes play a crucial role in the DNA topology regulation by facilitating DNA replication and chromosome segregation during cell division (6). The active form of DNA gyrase is a heterotetramer, GyrA2GyrB2, that catalyzes the negative supercoiling of DNA by wrapping a double-stranded segment around itself, cleaving this DNA in both strands, passing the wrapped DNA through the break, and then resealing the DNA (6). Quinolones inhibit DNA supercoiling by stabilizing the complex between gyrase and the cleaved DNA, interrupting the propagation of the replication fork. This and the permanent breakdown of DNA lead to the death of the bacteria (17). After the complete genome of M. leprae was sequenced (7), interestingly, no gene for topoisomerase IV was found. It is therefore very likely that DNA gyrase is the sole target of quinolones in M. leprae, as in Mycobacterium tuberculosis. Another particularity of M. leprae is the presence of a protein-splicing element, termed intein, in the gyrA gene encoding the GyrA subunit of DNA gyrase.
In order to measure the activities of new quinolones against M. leprae, we reconstituted in vitro the M. leprae DNA gyrase by expressing the two subunits separately in Escherichia coli as recombinant proteins carrying a poly-His tag and then measured the supercoiling inhibition of M. leprae DNA gyrase and the induction of DNA cleavage arising from stabilization of the cleavage complex by quinolones. We demonstrated that the in vitro activities of quinolones were consistent with the corresponding in vivo activities determined in the mouse footpad model. Therefore, determination of the interaction of quinolones with purified M. leprae DNA gyrase may provide a rapid, efficient, and safe in vitro test for the screening of new quinolones with putative anti-M. leprae activities.
MATERIALS AND METHODS
Reagents.
The following 13 quinolones were provided by their corresponding manufacturers: levofloxacin (Roussel Uclaf); gatifloxacin (Grünenthal, Levallois-Perret, France); ciprofloxacin and moxifloxacin (Bayer Pharma, Puteaux, France); sparfloxacin and pefloxacin (Aventis, Paris, France), nalidixic acid, oxolinic acid, and ofloxacin (Sigma-Aldrich Chimie, Saint Quentin Fallavier, France); temafloxacin (Abbott, Saint Rémy sur Avre, France); sitafloxacin (Daiichi Pharmaceutical, Co., Ltd. Tokyo, Japan); garenoxacin (Bristol-Meyers Squibb, Saint Nazaire, France); and clinafloxacin (Anakena Pharma Marketing, Japan). The oligonucleotide primers were synthesized by MWG (Ebersberg, Germany).
Bacterial strains and plasmids.
The gyrA and gyrB genes were amplified from cosmid B1770 of the M. leprae genome bank, which was kindly provided by S. Cole (7). E. coli DH5α was used as the host for cloning purposes, and the E. coli BL21 codon plus (λDE3) pLysS (Stratagene) was used for protein expression. The pMOS Blue plasmid kit (Amersham Biosciences Europe, Orsay, France) was used to clone the amplified DNA fragments. Plasmid pET-29a (Novagen, Merck Eurolab, Fontenay Sous Bois, France) was used to construct vectors for overexpression of the M. leprae GyrA and GyrB proteins. Supercoiled plasmid pBR322 DNA was provided by Roche Diagnostics (Meylan Cedex, France), and relaxed plasmid pBR322 DNA was obtained from John Innes Enterprises Ltd. (Norwich Research Park, Colney, Norwich, United Kingdom).
Construction of GyrA and GyrB expression vectors.
The intein-containing gyrA and gyrB genes were directly amplified from cosmid B1770, cloned into pMOS Blue, and inserted into pET-29a, as described hereafter. In each of the forward primers used for the amplification step, NdeI sites (CATATG) that overlapped the ATG initiation codon of gyrA and gyrB were engineered. Into each of the reverse primers, a XhoI site was introduced before the stop codon of gyrA and gyrB. The gyrA gene was amplified by using the forward primer (primer LEPSnew) 5′-GCAAATGAGGAACATATGACTGATATCACG-3′ (underlined bases correspond to the NdeI site; the ATG codon is indicated in boldface) and the reverse primer (primer LEPASnew) 5′-ATCACTTTACTCGAGACCGCCGTCGGCGCT (the XhoI site is underlined). The gyrB gene was amplified by using the forward primer (primer MLB2NdeI) 5′-CAAGGAGAGCATTCAGCATATGGCTGCCCAGAGG (the NdeI site is underlined; the ATG initiation codon is in boldface) and the reverse primer (primer MLBSPXhoI) 5′-CGTCGAAAAATGTCTCGAGTAAGTAGACATCCAGGA (the XhoI site is underlined). Cosmid B1770 DNA, which contains the gyrB and gyrA genes of M. leprae, was used as the template in the amplification reaction, which was carried out by using an Expand Long Template PCR system kit (Boehringer Mannheim, Meylan, France) in the presence of 5 mM deoxynucleoside triphosphates and 2.25 mM MgCl2. The amplification conditions were as follows: for gyrA, 10 min of denaturation at 94°C, 30 amplification cycles of 1 min of denaturation at 94°C, 1 min of annealing at 55°C, and 1 min of extension at 68°C; for gyrB, 2 min of denaturation at 94°C, 10 amplification cycles of denaturation at 94°C for 15 s, annealing at 55°C for 30 s, and extension at 68°C for 3 min, followed by 30 cycles of denaturation at 94°C for 15 s, annealing at 60°C for 30 s, and extension at 68°C for 4 min, with a final extension step for 7 min at 68°C. The PCR products obtained (3.7 kb for gyrA-intein and 2 kb for gyrB) were ligated into the pMOS Blue plasmid and transformed into E. coli MosBlue competent cells, according to the manufacturer's instructions. Recombinant plasmids were recovered from the white colonies and digested with NdeI and XhoI, and the DNA fragments obtained were ligated into NdeI-XhoI-cut pET-29a and transformed into E. coli DH5α. The resistant colonies selected on plates containing kanamycin (50 μg/ml) were screened for recombinant clones. The plasmid containing the M. leprae gyrA gene without the intein (plasmid MLA) was obtained by using a Quick Change site-directed mutagenesis kit (Stratagene), according to the manufacturer's instructions. Two primers were employed: primer DELINTEINS (5′-ACCGAGGCTCGGCTTACTCCATTGGCGATG) and primer DELINTEINAS (5′-ATAACGCATCGCTGCCGGTGGGTCATTACC). The absence of intein was checked by DNA sequencing.
Protein overexpression and purification of GyrA and GyrB subunits.
GyrA (MLA) and GyrB (MLB) were overexpressed and purified as described previously (1, 2), with minor modifications. In order to increase the yield of soluble proteins, the induction temperature was reduced to 14°C, with an induction time of 20 h. Since dialysis led to the loss of most of the purified proteins by precipitation, two amino acids (arginine and glutamic acid) were added to the dialysis buffer to prevent the precipitation of MLA and MLB (13). Protein concentrations were measured with a Nanodrop ND-1000 instrument, and the protein fractions were examined by sodium dodecyl sulfate (SDS)-polyacrylamide gel electrophoresis (PAGE).
DNA supercoiling assays.
DNA supercoiling activity was tested with 1 U of purified DNA gyrase (defined as the amount of DNA gyrase that converted 400 ng of relaxed pBR322 to the supercoiled form in 1 h at 30°C). The reaction mixture (total volume, 30 μl) contained the DNA gyrase assay buffer (40 mM Tris-HCl [pH 7.5], 25 mM KCl, 20 mM magnesium acetate, 2 mM spermidine, 4 mM dithiothreitol, 0.1 mg/ml of yeast tRNA, bovine serum albumin [0.36 mg/ml], 3 mM ATP [pH 8.0]) and relaxed pBR322 DNA (0.4 μg) as the substrate. Gyrase proteins were added, and the reaction mixtures were incubated at 30°C for 1 h. The reactions were stopped by the addition of glycerol (50%) containing 0.25% bromophenol blue. The total reaction mixture was subjected to 5 h of electrophoresis at 50 V in a 1% agarose gel in 0.5× TBE (Tris-borate-EDTA, pH 8.3) buffer. The gel was stained with ethidium bromide (0.7 mg/ml). The supercoiling activity was assessed by quantifying the brightness of the bands corresponding to the supercoiled pBR322 DNA with Molecular Analyst software (Bio-Rad).
The inhibitory effects of the quinolones on the recombinant M. leprae DNA gyrase were assessed by determining the concentration of drug required to inhibit the supercoiling activity of the enzyme by 50% (IC50) by following the method described previously (1, 2).
DNA cleavage assays.
DNA cleavage assays were carried out in the buffer used for DNA supercoiling, except that supercoiled pBR322 DNA instead of relaxed pBR322 DNA was used as the substrate. Three hundred nanograms of GyrA and 250 ng of GyrB were mixed in the presence of increasing concentrations of quinolones for 1 h at 30°C. Three microliters of 2% SDS was added to separate the free DNA from the cleaved DNA covalently linked to DNA gyrase, and 3 μl of a 1-mg/ml solution of proteinase K was added to remove the covalently bound GyrA protein. Incubation was continued for 30 min at 37°C. The reactions were stopped as described above for supercoiling. The DNA products were examined by agarose gel electrophoresis, and the drug concentration that resulted in 25% DNA cleavage (CC25) was determined.
RESULTS
Purification and DNA supercoiling activities of recombinant His-tagged GyrA and GyrB proteins from M. leprae.
The M. leprae gyrA and gyrB genes were amplified from cosmid B1770, which contains a gyrB-gyrA contig of M. leprae. The amplified genes were separately inserted in frame downstream of a T7 promoter in a pET29a expression vector, thus resulting in two recombinant plasmids, plasmids MLA (gyrA without the intein region) and MLB (gyrB), which allow the production of proteins with a hexahistidine tag at the C terminus. After expression in E. coli and purification, a 74.5-kDa protein from MLB and a 91.5-kDa protein from MLA were obtained at a concentration of about 0.5 mg/ml (Fig. 1).
FIG. 1.
SDS-PAGE analysis of purified M. leprae GyrA (MLA) and GyrB (MLB) proteins. The His-tagged proteins were overexpressed in E. coli and purified by nickel resin chromatography, and approximately 8 ng of each protein sample was loaded on an SDS-9% polyacrylamide gel. Following electrophoresis, the proteins were revealed by staining with Coomassie blue. Lane M, marker (sizes in kilodaltons are indicated to the right).
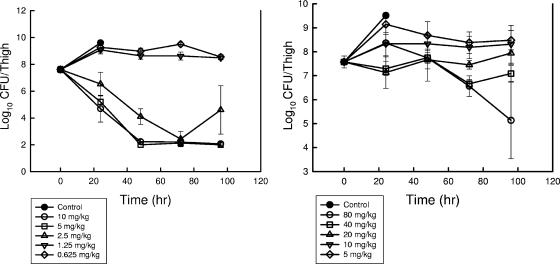
Combinations of the GyrA (MLA) and the GyrB (MLB) subunits were tested for their DNA supercoiling activities. As expected, either the GyrA subunit or the GyrB subunit alone did not induce any detectable activity (Fig. 2). In contrast, the combination of GyrA and GyrB subunits allowed the supercoiling of plasmid pBR322 in the presence of ATP, demonstrating that a functional DNA gyrase was reconstituted (Fig. 2). The specific supercoiling activities of the recombinant M. leprae DNA gyrase was 3.2 × 103 U/mg for GyrA and 2.8 × 103 U/mg for GyrB.
FIG. 2.
M. leprae GyrA and GyrB proteins generate an ATP-dependent DNA supercoiling activity. Relaxed pBR322 (0.4 μg) was incubated with DNA gyrase reconstituted from GyrA (1 U, i.e., 320 ng) and GyrB (1 U, i.e., 300 ng) in the presence of 3 mM ATP. The reactions were stopped, and the DNA products were separated by electrophoresis in a 1% agarose gel. DNA was stained with ethidium bromide and photographed under UV illumination. Lanes: a, supercoiled pBR322 DNA; b, relaxed pBR322 DNA; A, relaxed pBR322 DNA and GyrA (1 U) protein; B, relaxed pBR322 DNA and GyrB (1 U) protein; AB, relaxed pBR322 DNA and both GyrA (1 U) and GyrB (1 U). R and S, relaxed and supercoiled DNA, respectively.
Inhibition of DNA supercoiling by quinolones.
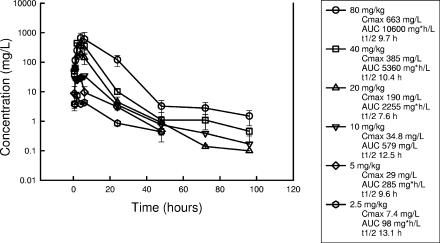
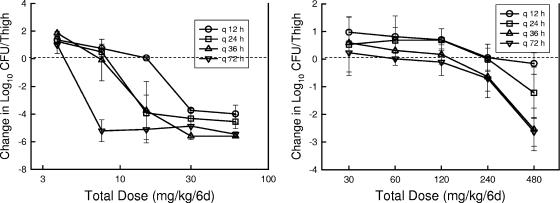
The abilities of 13 quinolones to inhibit 50% of the DNA supercoiling of the M. leprae DNA gyrase were investigated by using 2 U of MLA combined with 2 U of MLB in each test. Each of the quinolones showed a dose-dependent inhibition, and their IC50s ranged from 1 μg/ml (sitafloxacin) to 300 μg/ml (nalidixic acid). The results are summarized in Table 1, and a set of representative data (IC50s, 2, 5, and 7 μg/ml for gatifloxacin, sparfloxacin, and levofloxacin, respectively) is shown in Fig. 3. The 13 quinolones clustered into three groups according to their IC50 values. The quinolones of the first group had IC50s ≤10 μg/ml and included sitafloxacin, gatifloxacin, moxifloxacin, clinafloxacin, ciprofloxacin, garenoxacin, sparfloxacin, levofloxacin, and ofloxacin. The quinolones of the second group, pefloxacin and temafloxacin, showed values >10 μg/ml but <100 μg/ml. The quinolones of the third group, characterized by IC50s ≥100 μg/ml, included oxolinic acid and nalidixic acid.
TABLE 1.
Structural features and concentrations of quinolones inhibiting M. leprae DNA gyrase activity and M. leprae growtha
| Quinolone | R-1 | R-6 | R-7 | N- or C-8 | In vitro studies
|
Mouse MIC (mg/kg/day)c from in vivo studies | ||
|---|---|---|---|---|---|---|---|---|
| IC50 (μg/ml) | CC25 (μg/ml) | MGIb | ||||||
| Sitafloxacin | Fluorinated cyclopropyl | F | Pyrrolidine | C-Cl | 1 | 0.5 | ND | 25d |
| Gatifloxacin | Cyclopropyl | F | Piperazine | C-OCH3 | 2 | 1 | ND | ND |
| Moxifloxacin | Cyclopropyl | F | Azabicyclo | C-OCH3 | 2 | 2 | ND | 150e |
| Clinafloxacin | Cyclopropyl | F | Pyrrolidine | C-Cl | 3 | 0.6 | ND | ND |
| Ciprofloxacin | Cyclopropyl | F | Piperazine | C-H | 3.5 | 2.5 | 32 | >150f |
| Garenoxacin | Cyclopropyl | H | Azabicyclo | C-OCHF2 | 3.5 | 3 | ND | ND |
| Sparfloxacin | Cyclopropyl | F | Piperazine | C-F | 5 | 1 | ND | 15g |
| Levofloxacin | Bridge C-1-C-8 | F | Piperazine | Bridge C-1-C-8 | 7 | 3 | ND | ND |
| Ofloxacin | Bridge C-1-C-8 | F | Piperazine | Bridge C-1-C-8 | 10 | 10 | 20 | 150h |
| Pefloxacin | Ethyl | F | Piperazine | C-H | 23 | 40 | 29 | >300g |
| Temafloxacin | Difluorophenyl | F | Piperazine | C-H | 26 | 11 | 29 | 50g |
| Oxolinic acid | Ethyl | Bridge C-6-C-7 | Bridge C-6-C-7 | H | 170 | No | ND | ND |
| Nalidixic acid | Ethyl | H | CH3 | N | 300 | No | ND | ND |
ethyl, C2H5; cyclopropyl, c-C3H5; difluororophenyl, 2′,4-F-C3H5; No, not observed; ND, not determined.
MGI, mean growth index from days 11 to 18 at 5 μg/ml of drug determined with the BACTEC 460 system against M. leprae (10).
Dosage of quinolones given to mice infected with leprosy leading to a fully bactericidal effect (>99% of the M. leprae organisms were killed) even 9 months after the completion of therapy, expressed as mg of drug per kg of mouse body weight per day.
Datum from Dhople et al. (9).
Datum from Consigny et al. (8).
Datum from Guelpa-Lauras et al. (15).
Data from Gelber et al. (11).
Datum from Grosset et al. (14).
FIG. 3.
DNA supercoiling activity of M. leprae DNA gyrase is sensitive to inhibition by gatifloxacin (GAT), sparfloxacin (SPX), and levofloxacin (LVX). Relaxed pBR322 (0.4 μg) was incubated with DNA gyrase reconstituted from GyrA (2 U, i.e., 600 ng) and GyrB (2 U, i.e., 700 ng) in the absence or in the presence of gatifloxacin, sparfloxacin, or levofloxacin. The reactions were stopped, and the DNA products were analyzed by electrophoresis in a 1% agarose gel. Lane a, relaxed pBR322 DNA; R and S, relaxed and supercoiled DNA, respectively.
Analysis of the structure-activity relationship indicated that the most active quinolones shared several structural features: (i) a substituted carbon at position 8; (ii) a cyclopropyl group at N-1; (iii) a fluorine at C-6, except for garenoxacin, which has a difluoromethoxy substituent at C-8; and (iv) a substituent ring at C-7. None of the two quinolones of the third group displayed any of the four structural features mentioned above. As expected, ofloxacin was twofold less active than levofloxacin, because ofloxacin is a racemic mixture of the inactive R isomer and the active l isomer, levofloxacin.
DNA cleavage activity of M. leprae DNA gyrase in the presence of quinolones.
The enhancement of supercoiled pBR322 DNA cleavage by the M. leprae gyrase in the presence of each of the 13 quinolones was measured. A representative set of results obtained with moxifloxacin, gatifloxacin, and ofloxacin is presented in Fig. 4. As shown in Table 1, the CC25s were ≤10 μg/ml for sitafloxacin, gatifloxacin, moxifloxacin, clinafloxacin, ciprofloxacin, garenoxacin, sparfloxacin, levofloxacin, and ofloxacin. The CC25 of temafloxacin was 11 μg/ml, and that of pefloxacin was 40 μg/ml. Little or no enhancement of DNA cleavage was observed in presence of nalidixic acid or oxolinic acid. From a structure-activity point of view, the cluster of quinolones based on the DNA cleavage test was very similar to that based on the DNA supercoiling test. In addition, the results indicate that the presence of a fluorine at position 6 or a piperazinyl ring at C-7 is important for DNA cleavage since classical quinolones were unable to stimulate it.
FIG. 4.
Quinolone-mediated DNA cleavage by M. leprae DNA gyrase. Supercoiled pBR322 DNA (0.4 μg) was incubated with the M. leprae GyrA (300 ng) and GyrB (250 ng) proteins in the presence of ATP and of moxifloxacin (MXF), gatifloxacin (GAT), or ofloxacin (OFX) at the indicated concentration (in μg/ml). After addition of SDS and proteinase K, the DNA samples were analyzed by electrophoresis in 1% agarose. Lane a, supercoiled pBR322 DNA; R, N, and S, relaxed, nicked, and supercoiled DNA, respectively.
DISCUSSION
The inability to cultivate M. leprae in cell-free medium is a serious handicap for leprosy research, particularly for the screening of new drugs with anti-M. leprae activities. The results of the present study indicate that tests with purified M. leprae DNA gyrase as the target are useful in vitro systems for evaluation of the activities of quinolones against M. leprae. Based on the findings of our previous study on the expression and purification of M. tuberculosis DNA gyrase (1), we overproduced and purified the His-tagged GyrA and GyrB subunits of M. leprae and obtained a functional M. leprae DNA gyrase after reconstitution. It must be pointed out that one characteristic of the gyrA gene of M. leprae is the presence of an intein inserted close to the tyrosine residue of the active site (Tyr130). Inteins are proteins removed from host protein sequences during the posttranslational maturation process (23); their roles remain unclear. Heterologous expression and physiological studies of intein-containing genes require either posttranslational splicing in the heterologous host or the accurate excision of the intein-coding region of the gene before expression. Such technical difficulties explain the rarity of investigations of such genes (12, 16, 21, 32). After numerous failures to obtain efficient M. leprae intein splicing in E. coli (data not shown), we have successfully excised the intein-coding region of gyrA before expression and obtained a homogeneous purified protein, i.e., GyrA without intein, which showed an expected size of 91.5 kDa. Association of this protein with GyrB permitted the reconstitution of an active gyrase protein. As shown recently with M. tuberculosis (1) and also with various other bacteria (4, 27), addition of a poly-His tag to the GyrA and GyrB subunits did not hamper the DNA gyrase activity or the interaction with quinolones.
The activities of the quinolones were evaluated by two different assays: inhibition of DNA supercoiling and induction of DNA cleavage. We observed that both DNA supercoiling inhibition and DNA cleaved complex formation occurred in a dose-dependent manner, and 9 of the 13 quinolones tested displayed high levels of activity against M. leprae DNA gyrase, with IC50s and CC25s ≤10 μg/ml. The results of the quinolone structure-activity relationship analysis based on M. leprae DNA gyrase were highly concordant with those based on M. tuberculosis DNA gyrase (1). In brief, a substituted carbon at position 8, substitution of C-1 by a cyclopropyl, a fluor at position 6, and a substituent ring at C-7 of the quinolone are associated with stronger activities against the DNA gyrases of both M. tuberculosis and M. leprae.
The DNA cleavage assay was thought to be more relevant than the supercoiling inhibition assay for measurement of the activity of a gyrase inhibitor (3, 33). However, it seems that this conclusion does not apply to M. tuberculosis, as the effective quinolone concentrations measured by the DNA cleavage assay were slightly different from those measured by the supercoiling assay (range, twofold lower to twofold higher) and were less correlated with the concentrations inhibiting M. tuberculosis growth (1). In the case of M. leprae, except for pefloxacin, the effective quinolone concentrations that induced DNA cleavage were found to be two- to sixfold lower than those that inhibited the supercoiling activity, a ratio close to that found for E. coli DNA gyrase (3, 33). Among the 13 quinolones tested in the present study, the anti-M. leprae activities of sitafloxacin (9), moxifloxacin (8), ciprofloxacin (15), sparfloxacin (10, 11), ofloxacin (10, 14, 28), pefloxacin (11, 14, 15), and temafloxacin (11) were tested either in the mouse footpad system or in various in vitro systems. The ranking of the activities of these quinolones based on the inhibition of DNA supercoiling and the induction of DNA cleavage was similar to that based on the activities against M. leprae in the mouse footpad system or in in vitro assays (Table 1). For example, moxifloxacin is highly active at inhibiting M. leprae DNA gyrase and is also by far the most active quinolone against M. leprae in the mouse footpad system (8); on the other hand, ofloxacin is less active at inhibiting the DNA gyrase and is also significantly less bactericidal than moxifloxacin in the mouse (8). Despite good in vitro activity against the purified enzyme, ciprofloxacin is poorly active in vivo, probably due to unfavorable pharmacokinetics (15) and the lack of an intracellular killing ability (30).
In conclusion, we have succeeded in purifying M. leprae DNA gyrase, which is the sole target of quinolones in this particular microorganism. On the basis of measurement of the interaction between quinolones and the purified M. leprae DNA gyrase, we have developed two simple assays for the rapid investigation of the quinolone structure-activity relationship and the screening of new quinolone derivatives for their anti-M. leprae activities. These assays thus allow the testing of a great number of quinolone derivatives with the mouse footpad system, which is time-consuming, labor intensive, and expensive, to be avoided. We propose that only those quinolones with IC50s below 10 μg/ml be considered for further testing in the mouse footpad system.
Acknowledgments
We thank Géraldine Falzone and Xiao Su Pan for technical assistance and L. M. Fisher for advice on cloning strategies. Special thanks go to Baohong Ji, who substantially improved the intelligibility of the manuscript.
This work was supported by grants from INSERM (EMI 0004), the University of Paris (UPRES 1541), the Foundation Raoul Follereau, and the Association Claude Bernard.
Footnotes
Published ahead of print on 26 February 2007.
REFERENCES
- 1.Aubry, A., X. S. Pan, L. M. Fisher, V. Jarlier, and E. Cambau. 2004. Mycobacterium tuberculosis DNA gyrase: interaction with quinolones and correlation with antimycobacterial drug activity. Antimicrob. Agents Chemother. 481281-1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aubry, A., N. Veziris, E. Cambau, C. Truffot-Pernot, V. Jarlier, and L. M. Fisher. 2006. Novel gyrase mutations in quinolone-resistant and -hypersusceptible clinical isolates of Mycobacterium tuberculosis: functional analysis of mutant enzymes. Antimicrob. Agents Chemother. 50104-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barrett, J. F., J. I. Bernstein, H. M. Krause, J. J. Hilliard, and K. A. Ohemeng. 1993. Testing potential gyrase inhibitors of bacterial DNA gyrase: a comparison of the supercoiling inhibition assay and “cleavable complex” assay. Anal. Biochem. 214313-317. [DOI] [PubMed] [Google Scholar]
- 4.Blanche, F., B. Cameron, F. X. Bernard, L. Maton, B. Manse, L. Ferrero, N. Ratet, C. Lecoq, A. Goniot, D. Bisch, and J. Crouzet. 1996. Differential behaviors of Staphylococcus aureus and Escherichia coli type II DNA topoisomerases. Antimicrob. Agents Chemother. 402714-2720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cambau, E., E. Perani, I. Guillemin, P. Jamet, and B. Ji. 1997. Multidrug-resistance to dapsone, rifampicin, and ofloxacin in Mycobacterium leprae. Lancet 349103-104. [DOI] [PubMed] [Google Scholar]
- 6.Champoux, J. J. 2001. DNA topoisomerases: structure, function, and mechanism. Annu. Rev. Biochem. 70369-413. [DOI] [PubMed] [Google Scholar]
- 7.Cole, S. T., K. Eiglmeier, J. Parkhill, K. D. James, N. R. Thomson, P. R. Wheeler, N. Honore, T. Garnier, C. Churcher, D. Harris, K. Mungall, D. Basham, D. Brown, T. Chillingworth, R. Connor, R. M. Davies, K. Devlin, S. Duthoy, T. Feltwell, A. Fraser, N. Hamlin, S. Holroyd, T. Hornsby, K. Jagels, C. Lacroix, J. Maclean, S. Moule, L. Murphy, K. Oliver, M. A. Quail, M. A. Rajandream, K. M. Rutherford, S. Rutter, K. Seeger, S. Simon, M. Simmonds, J. Skelton, R. Squares, S. Squares, K. Stevens, K. Taylor, S. Whitehead, J. R. Woodward, and B. G. Barrell. 2001. Massive gene decay in the leprosy bacillus. Nature 4091007-1011. [DOI] [PubMed] [Google Scholar]
- 8.Consigny, S., A. Bentoucha, P. Bonnafous, J. Grosset, and B. Ji. 2000. Bactericidal activities of HMR 3647, moxifloxacin, and rifapentine against Mycobacterium leprae in mice. Antimicrob. Agents Chemother. 442919-2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dhople, A. M., and K. Namba. 2003. In-vitro activity of sitafloxacin (DU-6859a), either singly or in combination with rifampin analogs, against Mycobacterium leprae. J. Infect. Chemother. 912-15. [DOI] [PubMed] [Google Scholar]
- 10.Franzblau, S. G., and K. E. White. 1990. Comparative in vitro activities of 20 fluoroquinolones against Mycobacterium leprae. Antimicrob. Agents Chemother. 34229-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gelber, R. H., A. Iranmanesh, L. Murray, P. Siu, and M. Tsang. 1992. Activities of various quinolone antibiotics against Mycobacterium leprae in infected mice. Antimicrob. Agents Chemother. 362544-2547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gleason, F. K., and N. E. Olszewski. 2002. Isolation of the gene for the B12-dependent ribonucleotide reductase from Anabaena sp. strain PCC 7120 and expression in Escherichia coli. J. Bacteriol. 1846544-6550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Golovanov, A. P., G. M. Hautbergue, S. A. Wilson, and L. Y. Lian. 2004. A simple method for improving protein solubility and long-term stability. J. Am. Chem. Soc. 1268933-8939. [DOI] [PubMed] [Google Scholar]
- 14.Grosset, J. H., C. C. Guelpa-Lauras, E. G. Perani, and C. Beoletto. 1988. Activity of ofloxacin against Mycobacterium leprae in the mouse. Int. J. Lepr. Other Mycobact. Dis. 56259-264. [PubMed] [Google Scholar]
- 15.Guelpa-Lauras, C. C., E. G. Perani, A. M. Giroir, and J. H. Grosset. 1987. Activities of pefloxacin and ciprofloxacin against Mycobacterium leprae in the mouse. Int. J. Lepr. Other Mycobact. Dis. 5570-77. [PubMed] [Google Scholar]
- 16.Guhan, N., and K. Muniyappa. 2002. Mycobacterium tuberculosis RecA intein possesses a novel ATP-dependent site-specific double-stranded DNA endonuclease activity. J. Biol. Chem. 27716257-16264. [DOI] [PubMed] [Google Scholar]
- 17.Hooper, D. C. 2000. Mechanisms of action and resistance of older and newer fluoroquinolones. Clin. Infect. Dis. 31(Suppl. 2):S24-S28. [DOI] [PubMed] [Google Scholar]
- 18.Ji, B. 2000. Prospects for chemotherapy of leprosy. Indian J. Lepr. 72187-198. [PubMed] [Google Scholar]
- 19.Ji, B., and J. H. Grosset. 1990. Recent advances in the chemotherapy of leprosy. Lepr. Rev. 61313-329. [DOI] [PubMed] [Google Scholar]
- 20.Ji, B. H. 1985. Drug resistance in leprosy—a review. Lepr. Rev. 56265-278. [PubMed] [Google Scholar]
- 21.Klabunde, T., S. Sharma, A. Telenti, W. R. Jacobs, Jr., and J. C. Sacchettini. 1998. Crystal structure of GyrA intein from Mycobacterium xenopi reveals structural basis of protein splicing. Nat. Struct. Biol. 531-36. [DOI] [PubMed] [Google Scholar]
- 22.Levy, L., and B. Ji. 2006. The mouse foot-pad technique for cultivation of Mycobacterium leprae. Lepr. Rev. 775-24. [PubMed] [Google Scholar]
- 23.Liu, X. Q. 2000. Protein-splicing intein: genetic mobility, origin, and evolution. Annu. Rev. Genet. 3461-76. [DOI] [PubMed] [Google Scholar]
- 24.Maeda, Y., M. Makino, D. C. Crick, S. Mahapatra, S. Srisungnam, T. Takii, Y. Kashiwabara, and P. J. Brennan. 2002. Novel 33-kilodalton lipoprotein from Mycobacterium leprae. Infect. Immun. 704106-4111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matsuoka, M., Y. Kashiwabara, and M. Namisato. 2000. A Mycobacterium leprae isolate resistant to dapsone, rifampin, ofloxacin and sparfloxacin. Int. J. Lepr. Other Mycobact. Dis. 68452-455. [PubMed] [Google Scholar]
- 26.Owens, R. C., Jr., and P. G. Ambrose. 2005. Antimicrobial safety: focus on fluoroquinolones. Clin. Infect. Dis. 41(Suppl. 2):S144-S157. [DOI] [PubMed] [Google Scholar]
- 27.Pan, X. S., and L. M. Fisher. 1999. Streptococcus pneumoniae DNA gyrase and topoisomerase IV: overexpression, purification, and differential inhibition by fluoroquinolones. Antimicrob. Agents Chemother. 431129-1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pattyn, S. R. 1991. Anti-Mycobacterium leprae activity of several quinolones studied in the mouse. Int. J. Lepr. Other Mycobact. Dis. 59613-617. [PubMed] [Google Scholar]
- 29.Scollard, D. M., L. B. Adams, T. P. Gillis, J. L. Krahenbuhl, R. W. Truman, and D. L. Williams. 2006. The continuing challenges of leprosy. Clin. Microbiol. Rev. 19338-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shandil, R. K., R. Jayaram, P. Kaur, S. Gaonkar, B. L. Suresh, B. N. Mahesh, R. Jayashree, V. Nandi, S. Bharath, and V. Balasubramanian. 2007. Moxifloxacin, ofloxacin, sparfloxacin, and ciprofloxacin against Mycobacterium tuberculosis: evaluation of in vitro and pharmacodynamic indices that best predict in vivo efficacy. Antimicrob. Agents Chemother. 51576-582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shepard, C. C. 1960. Acid-fast bacilli in nasal excretions in leprosy, and results of inoculation of mice. Am. J. Hyg. 71147-157. [DOI] [PubMed] [Google Scholar]
- 32.Southworth, M. W., H. Kong, R. B. Kucera, J. Ware, H. W. Jannasch, and F. B. Perler. 1996. Cloning of thermostable DNA polymerases from hyperthermophilic marine Archaea with emphasis on Thermococcus sp. 9 degrees N-7 and mutations affecting 3′-5′ exonuclease activity. Proc. Natl. Acad. Sci. USA 935281-5285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Walton, L., and L. P. Elwell. 1988. In vitro cleavable-complex assay to monitor antimicrobial potency of quinolones. Antimicrob. Agents Chemother. 321086-1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WHO. 1982. Chemotherapy of leprosy for control programmes. WHO, Geneva, Switzerland.
- 35.WHO. 2006. Global leprosy situation, 2006. Wkly. Epidemiol. Rec. 81309-316. [PubMed] [Google Scholar]
- 36.WHO. 1998. WHO Expert Committee on Leprosy, seventh report. WHO Tech. Rep. Ser. 8741-39. [PubMed] [Google Scholar]