Abstract
Hydrogen breath tests are widely used to explore the pathophysiology of functional gastrointestinal disorders. Small intestinal bacterial overgrowth and carbohydrate malabsorption are disorders detected by these tests that have been proposed to be of great importance for symptoms in, for instance, irritable bowel syndrome. However, conclusions drawn from these studies are highly controversial and divergent results exist. There is also an extensive use of these tests in clinical practice with difficulties regarding interpretation of the tests and sometimes erroneous conclusions. The limitations and pitfalls of these tests will be reviewed in this article, and hopefully the occasional abuse of these tests can be turned into proper clinical and scientific use instead in the future.
Keywords: hydrogen breath tests, fructose malabsorption, irritable bowel syndrome, lactose malabsorption, small intestinal bacterial overgrowth
Within the field of gastroenterology, the majority of symptoms cannot be explained by structural abnormalities detected on routine investigations.1 Many of these symptoms are clustered together forming the functional gastrointestinal disorders, as defined by the Rome II criteria.2,3 The pathophysiology behind these disorders is still incompletely known.4 In the search for possible pathophysiological factors of functional gastrointestinal disorders, several authors have used different hydrogen breath tests in recent years to detect various abnormalities, such as carbohydrate malabsorption5,6,7 and small intestinal bacterial overgrowth (SIBO).8,9 However, these tests are indirect, with several drawbacks and pitfalls. In this article, we will review the literature on the use of hydrogen breath tests to detect carbohydrate malabsorption and SIBO, and highlight the controversies and inconsistencies in the interpretation of these tests, especially regarding the relevance of fructose malabsorption and SIBO in patients with functional gastrointestinal disorders.
Hydrogen breath tests
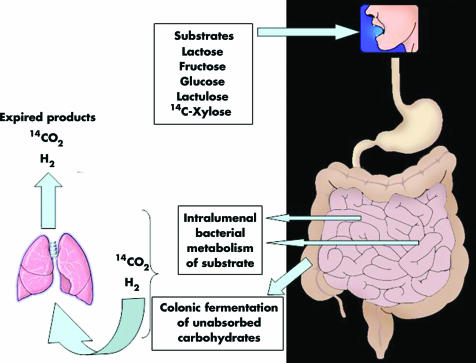
Hydrogen breath tests are based on the fact that there is no source for hydrogen gas in humans other than bacterial metabolism of carbohydrates.10 For these tests different carbohydrates are administered orally and the concentration of hydrogen is measured in expired air. When defective sugar absorption is present, unabsorbed sugars are available in the colon for bacterial fermentation, and in the case of SIBO the bacterial population migrates proximally in the small intestine gaining access to the sugars. When exposed to bacteria in the bowel, the substrate will be metabolised to hydrogen, which is quickly absorbed, expired, and possible to measure in expired air (fig 1). The different tests are performed in the fasting state after at least one day of a low fibre diet. Smoking raises and exercise lowers hydrogen concentrations and is therefore not allowed during the test.11 Glucose12,13 or lactulose14 are the most commonly used substrates for diagnosis of SIBO whereas the different sugars tested for carbohydrates malabsorption are given to detect these disorders.15
Figure 1 Schematic drawing showing the principles behind breath tests.
“Hydrogen breath tests are based on the fact that there is no source for hydrogen gas in humans other than bacterial metabolism of carbohydrates”
The hydrogen breath test depends on the presence of hydrogen producing bacteria. However, a considerable proportion of non‐hydrogen producing bacteria, which can yield false negative results, has been observed in some12,16,17 but not all studies.18,19,20 Several other potential sources of error exist, such as carbohydrate malabsorption in chronic pancreatitis and coeliac disease, with false positive tests for SIBO due to colonic fermentation and gas production,20,21,22,23 and gastrointestinal motor disorders, where delayed gastric emptying may cause false negative tests24 and rapid transit through the small bowel will produce false positive breath tests.22,25,26,27 False positive results may also be due to the oral bacterial flora and if the subject has failed to adhere to a low fibre diet the day before the test.
Carbohydrate malabsorption
Carbohydrate digestion and absorption
Almost all carbohydrates from the diet are large polysaccharides or disaccharides. In order to be adequately absorbed from the intestine into portal blood, poly‐ and disaccharides must undergo digestion in order to become absorbable monosaccharides (glucose, galactose, and fructose). For this, different enzymes are required, such as pancreatic amylase and intestinal epithelial enzymes (that is, lactase, sucrase, and maltase). Absorption is mainly an active transport, with selectivity for specific monosaccharides and competition between different sugars. Therefore, the composition of the diet influences the efficiency of carbohydrate absorption and the amount of carbohydrates that reaches the colon unabsorbed.
Carbohydrates that reach the colon unabsorbed are fermented by bacteria and have been proposed to be of importance for symptoms such as bloating, abdominal distension, and diarrhoea. In particular, lactose,7,28,29,30 fructose, and sorbitol5,31 has been extensively studied in patients with functional gastrointestinal disorders but more complex carbohydrates that escape small bowel absorption may be of even greater importance.32
Lactose malabsorption
Lactose absorption
Lactose, found in milk, is a disaccharide composed of galactose and glucose. It is digested by lactase, which is found on the brush border of small intestine epithelium, into glucose and galactose, and these monosaccharides can then be absorbed. Lactose maldigestion is the incomplete hydrolysis of lactose due to lactase deficiency, which may occur as a primary disorder33 or secondary to another disorder of the small intestinal mucosa, for instance coeliac disease.34 The vast majority of patients with the primary form have an acquired deficiency (that is, enzyme activity is normal during the first years of life but then declines with ageing). Because lactose cannot be absorbed it passes into the colon and through increased fluid secretion and gas production it can lead to gastrointestinal symptoms referred to as lactose intolerance. There are marked racial differences in the prevalence of lactase deficiency, with the prevalence being 3–8% in Scandinavia and Northwest Europe, increasing to close to 100% in Southeast Asia. In Europe, the frequency increases in southern and eastern directions, reaching 70% in southern Italy and Turkey.15
Testing for lactose malabsorption
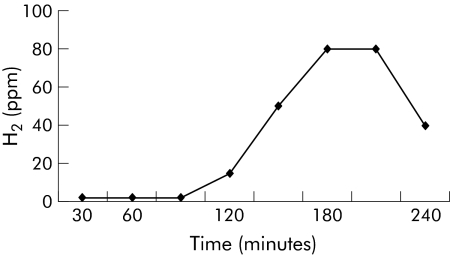
The most common test today to diagnose lactose malabsorption is the lactose hydrogen breath test. Breath hydrogen is measured following ingestion of 25–50 g lactose dissolved in 100–500 ml of water, and after intake hydrogen concentration in end expiratory air is determined at 15–30 minutes intervals for 4–5 hours. The definition of a positive test has varied but a rise of 10–20 ppm over basal values is usually considered to indicate lactose malabsorption. The rise should be detected in more than one breath sample. A positive test indicative of lactose malabsorption usually peaks at 2–4 hours (fig 2), while an early peak (within one hour of ingestion) may reflect rapid small bowel transit, SIBO, or substrate fermentation by the oral flora. The appearance of gastrointestinal symptoms during the test is also assessed to evaluate the presence of subjective lactose intolerance. However, this is usually done with the patient knowing that he/she has ingested lactose, which makes the usefulness of this information unclear. Importantly, there are great discrepancies between the presence of lactose maldigestion and symptoms of lactose intolerance,35,36 and lactose maldigesters can usually tolerate small amounts of lactose, up to 240 ml of milk (12.1 g lactose) daily according to one study, with minimal or no symptoms.35,37
Figure 2 Schematic drawing of hydrogen breath tests (fructose with or without sorbitol and lactose) indicating carbohydrate malabsorption.
Lactose malabsorption in functional gastrointestinal disorders
The importance of lactose malabsorption for gastrointestinal symptoms in irritable bowel syndrome (IBS) and other functional gastrointestinal disorders is controversial. The majority of studies, including a recent large survey of more than 1000 IBS patients, found the prevalence of lactose malabsorption in IBS subjects to be virtually the same as in the normal population.28,30,36,38,39 As stated previously, the prevalence of lactose maldigestion differs widely between different countries but the prevalence of IBS has not been found to differ substantially between countries with low versus high prevalence of lactose maldigestion.28,30,38 The importance of lactose malabsorption in IBS is therefore questionable, and the association between these two conditions is probably a coincidence because both are common and would be expected to occur together.40 However, in some studies, lactose malabsorption has been reported to be of great relevance for patients with IBS, and a positive effect on symptoms after lactose restriction has been demonstrated.7,29 Moreover, subjective lactose intolerance might be more prevalent in IBS patients due to increased sensitivity to lactose maldigestion in some, and to yet unresolved issues in others.7,36,29,41
“The importance of lactose malabsorption for gastrointestinal symptoms in IBS and other functional gastrointestinal disorders is controversial”
The importance of factors other than maldigestion of lactose behind subjective lactose intolerance is supported by the fact that self reported milk intolerance in IBS patients does not help in identifying lactose malabsorbers.42,43 Moreover, the majority of patients with lactose malabsorption can consume a considerable amount of lactose before having symptoms,35 and the use of lactase treatment seems to be of limited value.44 Therefore, subjective lactose intolerance is probably relevant only for a subgroup of IBS patients, especially in those consuming large amounts of dairy products. In these patients a lactose reduced diet might have a positive effect on some of the symptoms, especially diarrhoea and gas/bloating, but the general impression is that the importance of lactose malabsorption in IBS has been overestimated during the past, and that dietary lactose exclusion rarely ameliorates the symptoms to any large extent in these patients.40
Fructose malabsorption
Fructose absorption
Fructose is a ketohexose occurring naturally in its free form or as sucrose (glucose+fructose). It is widely used as a sweetener in different foods, beverages, and candy, and it is also present in fruits such as apples, peaches, cherries, and pears.45 It is absorbed by carrier mediated facilitated diffusion and results indicate that the capacity for fructose absorption is small compared with that for sucrose and glucose.46 The absorptive capacity for fructose varies greatly, but as high as 30–80% of healthy individuals tested with a hydrogen breath test demonstrated incomplete absorption of a 10% solution of 50 g of fructose.47,48,49 These studies also demonstrated that the absorptive capacity was unrelated to age or sex but that it was dose and concentration dependent. To put this dose into perspective, mean daily intake of free fructose (sucrose excluded) in the US population has been found to be 16 g/day but “heavy” consumers may reach 60–100 g/day.50
Testing for fructose malabsorption
When testing for fructose malabsorption, 25–50 g of fructose dissolved in 150–250 ml of water have been used. Methodology and interpretation of results is otherwise similar to lactose, as described above (fig 2). It is unclear what the optimal dosage of fructose is to detect clinically meaningful malabsorption. Another unresolved issue is how symptoms should be assessed during the test and to what extent these are reliable, as very few blinded studies have been performed and the majority of studies are also uncontrolled. Of great importance is also the fact that simultaneous ingestion of glucose increases fructose absorption,48,49 and the majority of dietary sources of fructose also contain glucose. On the other hand, simultaneous ingestion of sorbitol, a naturally found sugar alcohol often used as a “sugar free” sweetener by the food industry, increases malabsorption of fructose.51 Therefore, breath testing of fructose alone probably does not reflect fructose ingestion in everyday life, making interpretation of the test extremely unreliable from a clinical point of view.
Fructose malabsorption in functional gastrointestinal disorders
A controversial issue is the importance of symptomatic malabsorption of fructose and/or sorbitol in IBS and other functional gastrointestinal disorders. Based on the few direct comparisons existing in the literature, malabsorption of fructose and/or sorbitol is not more frequent in IBS patients than in healthy subjects.6,31,52,53 However, one study demonstrated that IBS patients with incomplete absorption of fructose had significantly more severe symptoms after ingestion of fructose than IBS subjects without malabsorption, and the symptoms were enhanced by adding sorbitol, supporting the role of symptomatic fructose‐sorbitol malabsorption in IBS.5 A subsequent large study reported a similar proportion of fructose‐sorbitol malabsorption in IBS patients with and without symptoms after intake of fructose and sorbitol, opposing the view of an important role for fructose‐sorbitol malabsorption in IBS.31 A Spanish study found more severe symptoms after intake of a fructose‐sorbitol mixture in patients with functional gastrointestinal disorders than after intake of sucrose as a control solution6 whereas we found similar symptoms in IBS patients with subjective fruit intolerance after intake of a fructose‐sorbitol mixture versus glucose (control), irrespective of the presence of fructose malabsorption.54
“Malabsorption of fructose and/or sorbitol is not more frequent in IBS patients than in healthy subjects”
As stated in a recent review, there is need for controlled studies clarifying the relation between incomplete fructose absorption and symptoms, and also assessing the effects of co‐ingestion of other sugars on fructose absorption.55 Until we have this information the role of fructose malabsorption tests in clinical practice remains uncertain. For IBS patients ingesting large amounts of fruits and/or products where artificial sweeteners are used, diets where fructose is empirically restricted might be tested.
Small intestinal bacterial overgrowth
SIBO is a condition caused by an abnormal number of bacteria in the small intestine. Symptoms related to bacterial overgrowth in the small intestine are diarrhoea, weight loss, anaemia, and malabsorption.56,57,58,59 SIBO is a common cause of malabsorption and malnutrition,56,60 especially among the elderly61,62 and in patients with blind loops,59 stenosis,63 diverticula,64,65 and motor disorders.66,67 Recently, SIBO has been suggested to be associated with a large number of different conditions, such as coeliac disease,34 chronic pancreatitis,68,69 hypothyroidism,70 Parkinson's disease,71 and fibromyalgia.72 However, the proposed contribution of SIBO to IBS has received the greatest attention, with studies demonstrating prevalence values of 38–84% of SIBO in IBS,8,9,72,73,74 but these studies have been heavily criticised,75,76,77,78,79 and contradictory results exist.80,81 In most cases the diagnosis of SIBO has been established by the use of hydrogen breath tests, usually with glucose or lactulose. However, the use of breath tests and interpretation of the result require knowledge about these tests. In some studies discussion around possible sources of errors with the test has been very sparse, as well as alternative interpretations of the results.68,82,83,84,85
“SIBO is a condition caused by an abnormal number of bacteria in the small intestine”
Normal bowel flora
The concentration of bacteria in the gastrointestinal tract increases in a caudal direction (table 1). The stomach is almost sterile and the upper part of the small bowel contains only small numbers of bacteria. The flora consists mainly of Gram positive bacteria. Strictly anaerobes are rare. In the distal part of the small bowel, the flora more resembles that of the large bowel but the ileocaecal valve acts as a barrier, with an increase in bacteria concentration distally to the valve. Gram negative aerobes predominate and strictly anaerobes are common. In the colon, anaerobes outnumber aerobes.86,87 There is large interindividual variability but within individuals the intestinal flora remains fairly constant over time.86
Table 1 Concentration of bacteria in different parts of the gastrointestinal tract (bacteria/ml).
| Stomach | Jejunum | Ileum | Caecum | |
|---|---|---|---|---|
| Aerobes | 102–103 | 102–104 | 105–108 | 102–109 |
| Anaerobes | 0 | 0 | 103–107 | 109–1012 |
| Total count | 102–103 | 102–104 | 105–108 | 1010–1012 |
Definition of SIBO
For several reasons the stability of the bowel flora can become disturbed so that bacterial overgrowth may occur. In the context of SIBO, this usually means abnormal numbers of normal inhabitants of the gastrointestinal tract. As the normal upper small bowel harbours less than 104 colony forming units/ml and the vast majority of these bacteria are Gram positive aerobes, it is possible to define SIBO as conditions differing from this (for example, a total growth of >104 bacteria and/or growth of Gram negatives or anaerobes). This definition can be acceptable in a strictly microbiological context but for clinical use it is of limited value as symptoms of SIBO correlate poorly with this definition. SIBO is usually defined as a total growth of >105 colony forming units/ml intestinal fluid.13,16,25,88,89,90 However, this definition is also insufficient as a substantial part of overgrowth with this definition consists of Gram positive flora. Gram positive overgrowth is mainly due to upper respiratory flora and is a frequent finding in the upper part of the small bowel of healthy elderly people91 and has not been correlated with symptoms of SIBO.92,93,94,95 Growth of colonic‐type bacteria (mainly Gram negatives, strictly anaerobes and enterococci) correlates with symptoms of SIBO.56,57,60 Furthermore, these bacteria possess certain properties such as the ability to deconjugate bile salts, affect the binding capacity of intrinsic factor, and reduce the absorptive function of enterocytes,87,96 mechanisms closely related to the symptoms of SIBO. A definition of SIBO as >105 colonic‐type bacteria therefore seems to be more clinically relevant.
Tests for SIBO
Small intestinal culturing
Culture of small bowel content is the most direct method for diagnosing SIBO and culture of jejunal aspirate is by many considered to be the gold standard. However, there are several difficulties associated with culturing. Obtaining aspirate for cultures is cumbersome and results of culturing are not always representative. It is a common belief that cultures are often false negative, especially concerning obligate anaerobes.60,97 Furthermore, only the upper part of the small bowel is accessible for culturing and bacteria have been proven to grow only at the actual location of the predisposing abnormality.98 On the other hand, false positive cultures due to contamination, mainly from the oral flora, are also believed to be common.99
Breath tests
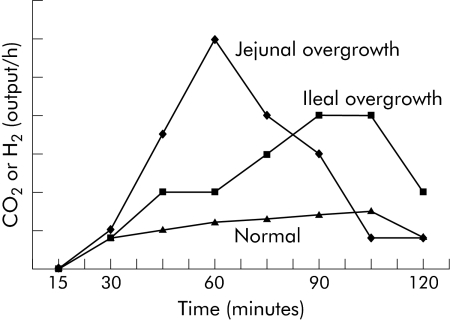
Because of the disadvantages with cultures, different breath tests have been developed. All of these are indirect tests based on certain metabolic characteristics unique for bacteria. There are three main types of breath tests used for diagnosing SIBO. The original breath test for diagnosing SIBO was the bile acid breath test,100,101 depending on the ability of many types of bacteria to deconjugate bile acids,56 but this test is rarely used today. In the 1 g 14C‐D‐xylose breath test,102,103 patients are given 1 g of 14C labelled xylose which after absorption is normally secreted through the kidneys with only minor endogenous metabolism. In the case of bacteria in the small bowel, xylose is metabolised to 14CO2 which is absorbed and expired and thus possible to detect with a breath test (fig 1), with an earlier peak implying jejunal overgrowth and a somewhat later peak more distal overgrowth (fig 3).
Figure 3 Examples of test results from glucose and xylose breath tests, indicating jejunal and ileal bacterial overgrowth, respectively, as well as a normal test.
“Hydrogen breath tests, using glucose or lactulose, are the most commonly used tests for SIBO today”
Hydrogen breath tests, using glucose12,13 or lactulose,14 are the most commonly used tests for SIBO today, and therefore the rest of the article will focus on these tests. Glucose is normally given in a dose of 50–75 g dissolved in water and lactulose in a dose of 10 g. H2 in end expiratory breath samples are thereafter measured every 15 minutes for up to three hours.
Abnormal versus normal results
Definitions of normal and abnormal results of breath tests are even more variable than for cultures. The lack of generally accepted definitions raises a situation where you can almost choose the test and definition that best suits your purpose. It is not uncommon to see the same authors change their definitions of a positive test in different papers.8,9,72 Only a few papers have described adequately their reasons for choosing a certain cut off point.23,24,25,104
Glucose is readily absorbed in the proximal small bowel, and in the absence of severe transit abnormalities it rarely reaches the colon,26,105 making it an attractive substrate to detect at least proximal SIBO. The glucose hydrogen breath test is considered positive if there is a clearly recognisable hydrogen peak, exceeding 10–20 ppm (fig 3).12,13,89 High fasting concentrations may be due to SIBO but this is a very unspecific finding which may also be due to slow intestinal transit leaving a residue of poorly absorbable carbohydrates remaining in the colon.16 Mostly, however, high fasting concentrations occur when the instruction to follow a low fibre diet before the test not has been followed.
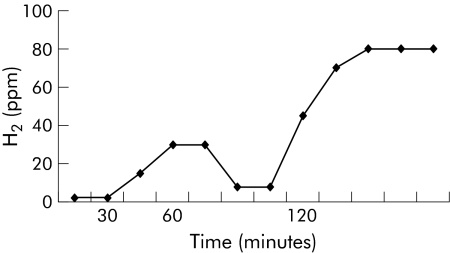
Lactulose passes unabsorbed through the small bowel and into the colon. Therefore, apart from detecting SIBO, it can also be used as a measure of orocaecal transit.106 The original definition of a positive lactulose test (that is, indicating SIBO) was an easily detected early hydrogen peak (>20 ppm), due to small intestinal bacteria, occurring at least 15 minutes before the later prolonged peak, corresponding to the passage of the remaining lactulose into the colon (fig 4).14 However, in some of the more recent studies, other less restrictive definitions, such as a rise in H2 within 90 minutes, have been used,9,72,74 which should be compared with the fact that the mean orocaecal transit time assessed with lactulose breath testing in healthy controls is slightly above 90 minutes.106,107 Therefore, using this definition, 50% of healthy controls would be expected to suffer from SIBO!79
Figure 4 A positive lactulose hydrogen breath test indicating small intestinal bacterial overgrowth with an easily detected early peak due to small bowel bacteria, clearly distinguishable from the later prolonged peak corresponding to the passage of the remaining lactulose into the colon.
“The sensitivity and specificity of the lactulose hydrogen breath test in detecting SIBO has been reported to be only 68% and 44%, and for the glucose breath test 62% and 83%”
Moreover, without a clear second peak in the lactulose breath test, it is impossible to distinguish SIBO from colonic fermentation, often caused by rapid transit,81,108 and importantly lactulose itself accelerates small bowel transit.107 However, not even detection of two easily distinguishable hydrogen peaks is a safe criterion as it has been shown in transit studies that a bolus can reach the caecum, imitating the first peak followed by the body of lumen contents, producing a second peak, yielding false positive lactulose tests.108,109 Therefore, it is not surprising that the sensitivity and specificity of the lactulose hydrogen breath test in detecting SIBO has been reported to be only 68% and 44%, and for the glucose breath test 62% and 83%.16
Which test should be used?
There is no general agreement as to which breath test is preferable.25,88,89,104 In some investigations the 1 g 14C‐D‐xylose breath test has shown excellent results but this has not been confirmed in more recent studies.23,25,104 However, as stated above, the hydrogen breath test with lactulose was found to have both lower specificity and sensitivity than other breath tests.16,89 Although sensitivity in general is acceptable, because of the low specificity for diagnosing SIBO compared with jejunal cultures, it has even been questioned if breath tests are useful at all for diagnosing SIBO.16,20,23,24,81,90,104,108
Is there a link between SIBO and IBS?
Recent studies suggest a strong link between SIBO and IBS, using the lactulose breath test,8,9,72,74,110 but others, using lactulose, glucose, and xylose breath tests, as well as jejunal cultures, have failed to confirm these findings.80,81 It has been proposed that the reason for the poor concordance between the lactulose breath test and jejunal cultures and the other breath tests is that lactulose is not absorbed in the small bowel. Because of this, the lactulose breath test is thought to be superior in detecting ileal bacterial overgrowth.8,9 As this part of the small bowel has other functions than the upper part, bacterial overgrowth of the distal small bowel may also cause different symptoms. Theoretically, it is possible that distal bacterial overgrowth would not cause malabsorption, but instead IBS symptoms. However, evidence of the existence of culture proven ileal bacterial overgrowth is lacking.
“Recent studies suggest a strong link between SIBO and IBS, using the lactulose breath test, but others, using lactulose, glucose, and xylose breath tests, as well as jejunal cultures, have failed to confirm these findings”
Pimentel et al have shown that the lactulose hydrogen breath test is often positive in IBS patients8,9,72 and that treatment with antibiotics or a low fibre diet in patients with IBS and a positive lactulose hydrogen breath test improves symptoms and reduces breath hydrogen concentration.9,111 Are these results really explained by the presence of SIBO? An alternative interpretation is that the positive breath test is due to hydrogen production by colonic bacteria and that treatment reduces the number of bacteria and their production of hydrogen. This is supported by preliminary findings from King and colleagues of abnormal colonic fermentation in IBS112 and a more recent study from the same group113 where they demonstrated that treatment of subjects with IBS with metronidazole or a low fibre diet improved symptoms, reduced gas excretion, and produced a corresponding decrease in the concentration of faecal bacteria.
The studies by Pimentel and others have paved the way towards studying alterations in the gut flora of IBS and other functional gastrointestinal disorders. The story of SIBO and IBS has not come to an end and hopefully future studies will be performed using appropriate methods and correct interpretation of the results.
Conclusion
Hydrogen breath tests are simple and safe, providing us with an easy tool to unravel the pathophysiological alterations behind symptoms difficult to explain. However, these tests have a number of limitations. The importance of SIBO and bacteria in other parts of the gut for functional gastrointestinal symptoms remains to be determined, and breath tests used wisely can be important together with other techniques in future studies. Today, regular use of the lactulose breath test in clinical practice in the evaluation of symptoms in patients with suspected functional gastrointestinal disorders cannot be recommended. The relevance of maldigestion of specific carbohydrates, such as lactose and fructose, in functional gastrointestinal disorders is probably overestimated. However, in some patients with a large intake of products containing these sugars, a hydrogen breath test, followed by dietary restriction of the sugar in case of a positive test, may be advised. Hopefully, the occasional abuse of hydrogen breath tests seen today can be turned into proper clinical and scientific use in the future.
Abbreviations
SIBO - small intestinal bacterial overgrowth
IBS - irritable bowel syndrome
Footnotes
Conflict of interest: None declared.
References
- 1.Kroenke K, Mangelsdorff A D. Common symptoms in ambulatory care: incidence, evaluation, therapy, and outcome. Am J Med 198986262–266. [DOI] [PubMed] [Google Scholar]
- 2.Talley N J, Stanghellini V, Heading R C.et al Functional gastroduodenal disorders. Gut 199945(suppl 2)II37–II42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thompson W G, Longstreth G F, Drossman D A.et al Functional bowel disorders and functional abdominal pain. Gut 199945(suppl 2)II43–II47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mayer E A, Naliboff B D, Chang L. Basic pathophysiologic mechanisms in irritable bowel syndrome. Dig Dis 200119212–218. [DOI] [PubMed] [Google Scholar]
- 5.Rumessen J J, Gudmand‐Hoyer E. Functional bowel disease: malabsorption and abdominal distress after ingestion of fructose, sorbitol, and fructose‐sorbitol mixtures. Gastroenterology 198895694–700. [DOI] [PubMed] [Google Scholar]
- 6.Fernandez‐Banares F, Esteve‐Pardo M, de Leon R.et al Sugar malabsorption in functional bowel disease: clinical implications. Am J Gastroenterol 1993882044–2050. [PubMed] [Google Scholar]
- 7.Böhmer C J, Tuynman H A. The clinical relevance of lactose malabsorption in irritable bowel syndrome. Eur J Gastroenterol Hepatol 199681013–1016. [DOI] [PubMed] [Google Scholar]
- 8.Pimentel M, Chow E J, Lin H C. Eradication of small intestinal bacterial overgrowth reduces symptoms of irritable bowel syndrome. Am J Gastroenterol 2000953503–3506. [DOI] [PubMed] [Google Scholar]
- 9.Pimentel M, Chow E J, Lin H C. Normalization of lactulose breath testing correlates with symptom improvement in irritable bowel syndrome. a double‐blind, randomized, placebo‐controlled study. Am J Gastroenterol 200398412–419. [DOI] [PubMed] [Google Scholar]
- 10.Levitt M D. Production and excretion of hydrogen gas in man. N Engl J Med 1969281122–127. [DOI] [PubMed] [Google Scholar]
- 11.Thompson D G, Binfield P, De Belder A.et al Extra intestinal influences on exhaled breath hydrogen measurements during the investigation of gastrointestinal disease. Gut 1985261349–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Metz G, Gassull M A, Drasar B S.et al Breath‐hydrogen test for small‐intestinal bacterial colonisation. Lancet 19761668–669. [DOI] [PubMed] [Google Scholar]
- 13.Kerlin P, Wong L. Breath hydrogen testing in bacterial overgrowth of the small intestine. Gastroenterology 198895982–988. [DOI] [PubMed] [Google Scholar]
- 14.Rhodes J M, Middleton P, Jewell D P. The lactulose hydrogen breath test as a diagnostic test for small‐bowel bacterial overgrowth. Scand J Gastroenterol 197914333–336. [DOI] [PubMed] [Google Scholar]
- 15.Gudmand‐Hoyer E. The clinical significance of disaccharide maldigestion. Am J Clin Nutr 199459735–41S. [DOI] [PubMed] [Google Scholar]
- 16.Corazza G R, Menozzi M G, Strocchi A.et al The diagnosis of small bowel bacterial overgrowth. Reliability of jejunal culture and inadequacy of breath hydrogen testing. Gastroenterology 199098302–309. [DOI] [PubMed] [Google Scholar]
- 17.Khin Maung U, Tin A, Ku Tin M.et al In vitro hydrogen production by enteric bacteria cultured from children with small bowel bacterial overgrowth. J Pediatr Gastroenterol Nutr 199214192–197. [DOI] [PubMed] [Google Scholar]
- 18.Christl S U, Murgatroyd P R, Gibson G R.et al Production, metabolism, and excretion of hydrogen in the large intestine. Gastroenterology 19921021269–1277. [PubMed] [Google Scholar]
- 19.Strocchi A, Levitt M D. Maintaining intestinal H2 balance: credit the colonic bacteria. Gastroenterology 19921021424–1426. [DOI] [PubMed] [Google Scholar]
- 20.Riordan S M, McIver C J, Bolin T D.et al Fasting breath hydrogen concentrations in gastric and small‐intestinal bacterial overgrowth. Scand J Gastroenterol 199530252–257. [DOI] [PubMed] [Google Scholar]
- 21.Kerlin P, Wong L, Harris B.et al Rice flour, breath hydrogen, and malabsorption. Gastroenterology 198487578–585. [PubMed] [Google Scholar]
- 22.Corazza G R, Strocchi A, Gasbarrini G. Fasting breath hydrogen in celiac disease. Gastroenterology 19879353–58. [DOI] [PubMed] [Google Scholar]
- 23.Riordan S M, McIver C J, Duncombe V M.et al Factors influencing the 1‐g 14C‐D‐xylose breath test for bacterial overgrowth. Am J Gastroenterol 1995901455–1460. [PubMed] [Google Scholar]
- 24.Valdovinos M A, Camilleri M, Thomforde G M.et al Reduced accuracy of 14C‐D‐xylose breath test for detecting bacterial overgrowth in gastrointestinal motility disorders. Scand J Gastroenterol 199328963–968. [DOI] [PubMed] [Google Scholar]
- 25.Rumessen J J, Gudmand‐Hoyer E, Bachmann E.et al Diagnosis of bacterial overgrowth of the small intestine. Comparison of the 14C‐D‐xylose breath test and jejunal cultures in 60 patients. Scand J Gastroenterol 1985201267–1275. [DOI] [PubMed] [Google Scholar]
- 26.Sellin J H, Hart R. Glucose malabsorption associated with rapid intestinal transit. Am J Gastroenterol 199287584–589. [PubMed] [Google Scholar]
- 27.Strocchi A, Corazza G, Ellis C J.et al Detection of malabsorption of low doses of carbohydrate: accuracy of various breath H2 criteria. Gastroenterology 19931051404–1410. [DOI] [PubMed] [Google Scholar]
- 28.Bozzani A, Penagini R, Velio P.et al Lactose malabsorption and intolerance in Italians. Clinical implications. Dig Dis Sci 1986311313–1316. [DOI] [PubMed] [Google Scholar]
- 29.Böhmer C J, Tuynman H A. The effect of a lactose‐restricted diet in patients with a positive lactose tolerance test, earlier diagnosed as irritable bowel syndrome: a 5‐year follow‐up study. Eur J Gastroenterol Hepatol 200113941–944. [DOI] [PubMed] [Google Scholar]
- 30.Farup P G, Monsbakken K W, Vandvik P O. Lactose malabsorption in a population with irritable bowel syndrome: prevalence and symptoms. A case‐control study. Scand J Gastroenterol 200439645–649. [DOI] [PubMed] [Google Scholar]
- 31.Nelis G F, Vermeeren M A, Jansen W. Role of fructose‐sorbitol malabsorption in the irritable bowel syndrome. Gastroenterology 1990991016–1020. [DOI] [PubMed] [Google Scholar]
- 32.Levitt M D, Hirsh P, Fetzer C A.et al H2 excretion after ingestion of complex carbohydrates. Gastroenterology 198792383–389. [DOI] [PubMed] [Google Scholar]
- 33.Huang S S, Bayless T M. Lactose intolerance in healthy children. N Engl J Med 19672761283–1287. [DOI] [PubMed] [Google Scholar]
- 34.Ghoshal U C, Ghoshal U, Misra A.et al Partially responsive celiac disease resulting from small intestinal bacterial overgrowth and lactose intolerance. BMC Gastroenterol 2004410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Suarez F L, Savaiano D A, Levitt M D. A comparison of symptoms after the consumption of milk or lactose‐ hydrolyzed milk by people with self‐reported severe lactose intolerance. N Engl J Med 19953331–4. [DOI] [PubMed] [Google Scholar]
- 36.Vesa T H, Seppo L M, Marteau P R.et al Role of irritable bowel syndrome in subjective lactose intolerance. Am J Clin Nutr 199867710–715. [DOI] [PubMed] [Google Scholar]
- 37.Vesa T H, Korpela R A, Sahi T. Tolerance to small amounts of lactose in lactose maldigesters. Am J Clin Nutr 199664197–201. [DOI] [PubMed] [Google Scholar]
- 38.Ferguson A, MacDonald D M, Brydon W G. Prevalence of lactase deficiency in British adults. Gut 198425163–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hamm L R, Sorrells S C, Harding J P.et al Additional investigations fail to alter the diagnosis of irritable bowel syndrome in subjects fulfilling the Rome criteria. Am J Gastroenterol 1999941279–1282. [DOI] [PubMed] [Google Scholar]
- 40.Turnbull G K. Lactose intolerance and irritable bowel syndrome. Nutrition 200016665–666. [DOI] [PubMed] [Google Scholar]
- 41.Simrén M, Månsson A, Langkilde A M.et al Food‐related gastrointestinal symptoms in the irritable bowel syndrome. Digestion 200163108–115. [DOI] [PubMed] [Google Scholar]
- 42.Simrén M, Månsson A, Bengtsson U.et al Lactose maldigestion does not explain subjective intolerance for dairy products in the irritable bowel syndrome (IBS). Gastroenterology 20011204059 [Google Scholar]
- 43.Vernia P, Marinaro V, Argnani F.et al Self‐reported milk intolerance in irritable bowel syndrome: what should we believe? Clin Nutr 200423996–1000. [DOI] [PubMed] [Google Scholar]
- 44.Lisker R, Solomons N W, Perez Briceno R.et al Lactase and placebo in the management of the irritable bowel syndrome: a double‐blind, cross‐over study. Am J Gastroenterol 198984756–762. [PubMed] [Google Scholar]
- 45.Rumessen J J. Fructose and related food carbohydrates. Sources, intake, absorption, and clinical implications. Scand J Gastroenterol 199227819–828. [DOI] [PubMed] [Google Scholar]
- 46.Riby J E, Fujisawa T, Kretchmer N. Fructose absorption. Am J Clin Nutr 199358748–53S. [DOI] [PubMed] [Google Scholar]
- 47.Ravich W J, Bayless T M, Thomas M. Fructose: incomplete intestinal absorption in humans. Gastroenterology 19838426–29. [PubMed] [Google Scholar]
- 48.Rumessen J J, Gudmand‐Hoyer E. Absorption capacity of fructose in healthy adults. Comparison with sucrose and its constituent monosaccharides. Gut 1986271161–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Truswell A S, Seach J M, Thorburn A W. Incomplete absorption of pure fructose in healthy subjects and the facilitating effect of glucose. Am J Clin Nutr 1988481424–1430. [DOI] [PubMed] [Google Scholar]
- 50.Glinsmann W H, Irausquin H, Park Y K. Evaluation of health aspects of sugars contained in carbohydrate sweeteners. Report of Sugars Task Force, 1986. J Nutr 1986116S1–216. [DOI] [PubMed] [Google Scholar]
- 51.Rumessen J J, Gudmand‐Hoyer E. Malabsorption of fructose‐sorbitol mixtures. Interactions causing abdominal distress. Scand J Gastroenterol 198722431–436. [DOI] [PubMed] [Google Scholar]
- 52.Symons P, Jones M P, Kellow J E. Symptom provocation in irritable bowel syndrome. Effects of differing doses of fructose‐sorbitol. Scand J Gastroenterol 199227940–944. [DOI] [PubMed] [Google Scholar]
- 53.Evans P R, Piesse C, Bak Y T.et al Fructose‐sorbitol malabsorption and symptom provocation in irritable bowel syndrome: relationship to enteric hypersensitivity and dysmotility. Scand J Gastroenterol 1998331158–1163. [DOI] [PubMed] [Google Scholar]
- 54.Simrén M, Månsson A, Bengtsson U.et al Is malabsorption of fructose‐sorbitol really important in the irritable bowel syndrome (IBS)? Gastroenterology 20011203232 [Google Scholar]
- 55.Skoog S M, Bharucha A E. Dietary fructose and gastrointestinal symptoms: a review. Am J Gastroenterol 2004992046–2050. [DOI] [PubMed] [Google Scholar]
- 56.Donaldson R M. Role of enteric microorganisms in malabsorption. Fed Proc 1967261426–1431. [PubMed] [Google Scholar]
- 57.King C E, Toskes P P. Small intestine bacterial overgrowth. Gastroenterology 1979761035–1055. [PubMed] [Google Scholar]
- 58.Kirsch M. Bacterial overgrowth. Am J Gastroenterol 199085231–237. [PubMed] [Google Scholar]
- 59.Toskes P P. Bacterial overgrowth of the gastrointestinal tract. Adv Intern Med 199338387–407. [PubMed] [Google Scholar]
- 60.Tabaqchali S. The pathophysiological role of small intestinal bacterial flora. Scand J Gastroenterol Suppl 19706139–163. [PubMed] [Google Scholar]
- 61.Roberts S H, James O, Jarvis E H. Bacterial overgrowth syndrome without "blind loop": A cause for malnutrition in the elderly. Lancet 197721193–1195. [DOI] [PubMed] [Google Scholar]
- 62.McEvoy A, Dutton J, James O F. Bacterial contamination of the small intestine is an important cause of occult malabsorption in the elderly. Br Med J (Clin Res Ed) 1983287789–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bishop R F, Anderson C M. The bacterial flora of the stomach and small intestine in children with intestinla obstruction. Arch Dis Child 196035487–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Farrar W E, Jr, O'Dell N M, Achord J L.et al Intestinal microflora and absorption in patients with stagnation‐inducing lesions of the small intestine. Am J Dig Dis 1972171065–1074. [DOI] [PubMed] [Google Scholar]
- 65.Eggert A. Interdigestive Motilität bei duodenaldivertikeln. Langerbecks Arch Chir 198837397–103. [DOI] [PubMed] [Google Scholar]
- 66.Vantrappen G, Janssens J, Hellemans J.et al The interdigestive motor complex of normal subjects and patients with bacterial overgrowth of the small intestine. J Clin Invest 1977591158–1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Stotzer P O, Björnsson E S, Abrahamsson H. Interdigestive and postprandial motility in small‐intestinal bacterial overgrowth. Scand J Gastroenterol 199631875–880. [DOI] [PubMed] [Google Scholar]
- 68.Casellas F, Guarner L, Vaquero E.et al Hydrogen breath test with glucose in exocrine pancreatic insufficiency. Pancreas 199816481–486. [DOI] [PubMed] [Google Scholar]
- 69.Trespi E, Ferrieri A. Intestinal bacterial overgrowth during chronic pancreatitis. Curr Med Res Opin 19991547–52. [DOI] [PubMed] [Google Scholar]
- 70.Lauritano E C, Lupascu A, Scarpellini E.et al Small intestinal bacterial overgrowth prevalence in hypothyroidism. Gastroenterology 2005128W1743 [Google Scholar]
- 71.Lupascu A, Lauritano C, Scarpellini E.et al Small intestinal bacterial overgrowth prevalence in Parkinson's disease. Gastroenterology 2005128W1742 [Google Scholar]
- 72.Pimentel M, Wallace D, Hallegua D.et al A link between irritable bowel syndrome and fibromyalgia may be related to findings on lactulose breath testing. Ann Rheum Dis 200463450–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.McCallum R, Schultz C, Sostarich S. Evaluating the role of small intestinal bacterial overgrowth (SIBO) in diarrhea predominant IBS (IBS‐D) patients utilizing the glucose breath test. Gastroenterology 2005128T1118 [Google Scholar]
- 74.Nucera G, Gabrielli M, Lupascu A.et al Abnormal breath tests to lactose, fructose and sorbitol in irritable bowel syndrome may be explained by small intestinal bacterial overgrowth. Aliment Pharmacol Ther 2005211391–1395. [DOI] [PubMed] [Google Scholar]
- 75.Cuoco L, Cammarota G, Jorizzo R.et al Small intestinal bacterial overgrowth and symptoms of irritable bowel syndrome. Am J Gastroenterol 2001962281–2282. [DOI] [PubMed] [Google Scholar]
- 76.Jones M P, Craig R, Olinger E. Small intestinal bacterial overgrowth is associated with irritable bowel syndrome: the cart lands squarely in front of the horse. Am J Gastroenterol 2001963204–3205. [DOI] [PubMed] [Google Scholar]
- 77.Mishkin D, Mishkin S. Re: Pimentel et al. Eradication of small intestinal bacterial overgrowth reduces symptoms of irritable bowel syndrome. Am J Gastroenterol 2001962505–2506. [DOI] [PubMed] [Google Scholar]
- 78.Riordan S M, McIver C J, Duncombe V M.et al Small intestinal bacterial overgrowth and the irritable bowel syndrome. Am J Gastroenterol 2001962506–2508. [DOI] [PubMed] [Google Scholar]
- 79.Hasler W L. Lactulose breath testing, bacterial overgrowth, and IBS: just a lot of hot air? Gastroenterology 20031251898–1900. [DOI] [PubMed] [Google Scholar]
- 80.Posserud I, Ringström G, Stotzer P O.et al Small intestinal bacterial overgrowth (SIBO) in irritable bowel syndrome (IBS). Neurogastroenterol Motil 200416839 [Google Scholar]
- 81.Walters B, Vanner S J. Detection of bacterial overgrowth in IBS using the lactulose H breath test: comparison with C‐D‐xylose and healthy controls. Am J Gastroenterol 20051001566–1570. [DOI] [PubMed] [Google Scholar]
- 82.Iivonen M K, Ahola T O, Matikainen M J. Bacterial overgrowth, intestinal transit, and nutrition after total gastrectomy. Comparison of a jejunal pouch with Roux‐en‐Y reconstruction in a prospective random study. Scand J Gastroenterol 19983363–70. [DOI] [PubMed] [Google Scholar]
- 83.Attar A, Flourie B, Rambaud J C.et al Antibiotic efficacy in small intestinal bacterial overgrowth‐related chronic diarrhea: a crossover, randomized trial. Gastroenterology 1999117794–797. [DOI] [PubMed] [Google Scholar]
- 84.Castiglione F, Rispo A, Di Girolamo E.et al Antibiotic treatment of small bowel bacterial overgrowth in patients with Crohn's disease. Aliment Pharmacol Ther 2003181107–1112. [DOI] [PubMed] [Google Scholar]
- 85.Di Stefano M, Miceli E, Missanelli A.et al Absorbable vs. non‐absorbable antibiotics in the treatment of small intestine bacterial overgrowth in patients with blind‐loop syndrome. Aliment Pharmacol Ther 200521985–992. [DOI] [PubMed] [Google Scholar]
- 86.Donaldson R M. Normal bacterial populations of the intestine and their relation to intestinal function. N Engl J Med 1964270938–945. [DOI] [PubMed] [Google Scholar]
- 87.Simon G L, Gorbach S L. Intestinal flora in health and disease. Gastroenterology 198486174–193. [PubMed] [Google Scholar]
- 88.Schneider A, Novis B, Chen V.et al Value of the 14C‐D‐xylose breath test in patients with intestinal bacterial overgrowth. Digestion 19853286–91. [DOI] [PubMed] [Google Scholar]
- 89.King C E, Toskes P P. Comparison of the 1‐gram[14C]xylose, 10‐gram lactulose‐H2, and 80‐gram glucose‐H2 breath tests in patients with small intestine bacterial overgrowth. Gastroenterology 1986911447–1451. [DOI] [PubMed] [Google Scholar]
- 90.Donald I P, Kitchingmam G, Donald F.et al The diagnosis of small bowel bacterial overgrowth in elderly patients. J Am Geriatr Soc 199240692–696. [DOI] [PubMed] [Google Scholar]
- 91.Husebye E, Skar V, Hoverstad T.et al Fasting hypochlorhydria with gram positive gastric flora is highly prevalent in healthy old people. Gut 1992331331–1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Holt P R, Rosenberg I H, Russell R M. Causes and consequences of hypochlorhydria in the elderly. Dig Dis Sci 198934933–937. [DOI] [PubMed] [Google Scholar]
- 93.Lipski P S, Kelly P J, James O F. Bacterial contamination of the small bowel in elderly people: is it necessarily pathological? Age Ageing 1992215–12. [DOI] [PubMed] [Google Scholar]
- 94.MacMahon M, Lynch M, Mullins E.et al Small intestinal bacterial overgrowth—an incidental finding? J Am Geriatr Soc 199442146–149. [DOI] [PubMed] [Google Scholar]
- 95.Saltzman J R, Kowdley K V, Pedrosa M C.et al Bacterial overgrowth without clinical malabsorption in elderly hypochlorhydric subjects. Gastroenterology 1994106615–623. [DOI] [PubMed] [Google Scholar]
- 96.Lewis R, Gorbach S. Modification of bile acids by intestinal bacteria. Arch Intern Med 1972130545–549. [PubMed] [Google Scholar]
- 97.Drasar B S, Shiner M, McLeod G M. Studies on the intestinal flora. I. The bacterial flora of the gastrointestinal tract in healthy and achlorhydric persons. Gastroenterology 19695671–79. [PubMed] [Google Scholar]
- 98.Gorbach S L, Plaut A G, Nahas L.et al Studies of intestinal microflora. II. Microorganisms of the small intestine and their relations to oral and fecal flora. Gastroenterology 196753856–867. [PubMed] [Google Scholar]
- 99.Hamilton I, Worsley B W, Cobden I.et al Simultaneous culture of saliva and jejunal aspirate in the investigation of small bowel bacterial overgrowth. Gut 198223847–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fromm H, Hofmann A F. Breath test for altered bile‐acid metabolism. Lancet 19712621–625. [DOI] [PubMed] [Google Scholar]
- 101.Sherr H P, Sasaki Y, Newman A.et al Detection of bacterial deconjugation of bile salts by a convenient breath‐analysis technic. N Engl J Med 1971285656–661. [DOI] [PubMed] [Google Scholar]
- 102.Toskes P P, King C E, Spivey J C.et al Xylose catabolism in the experimental rat blind loop syndrome: studies, including use of a newly developed d‐[14C]xylose breath test. Gastroenterology 197874691–697. [PubMed] [Google Scholar]
- 103.King C E, Toskes P P, Spivey J C.et al Detection of small intestine bacterial overgrowth by means of a 14C‐D‐xylose breath test. Gastroenterology 19797775–82. [PubMed] [Google Scholar]
- 104.Stotzer P O, Kilander A F. Comparison of the 1‐gram (14)C‐D‐xylose breath test and the 50‐gram hydrogen glucose breath test for diagnosis of small intestinal bacterial overgrowth. Digestion 200061165–171. [DOI] [PubMed] [Google Scholar]
- 105.Bond J H, Jr, Levitt M D. Use of pulmonary hydrogen (H 2 ) measurements to quantitate carbohydrate absorption. Study of partially gastrectomized patients. J Clin Invest 1972511219–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hirakawa M, Iida M, Kohrogi N.et al Hydrogen breath test assessment of orocecal transit time: comparison with barium meal study. Am J Gastroenterol 1988831361–1363. [PubMed] [Google Scholar]
- 107.Bond J H, Jr, Levitt M D, Prentiss R. Investigation of small bowel transit time in man utilizing pulmonary hydrogen (H2) measurements. J Lab Clin Med 197585546–555. [PubMed] [Google Scholar]
- 108.Riordan S M, McIver C J, Walker B M.et al The lactulose breath hydrogen test and small intestinal bacterial overgrowth. Am J Gastroenterol 1996911795–1803. [PubMed] [Google Scholar]
- 109.Sadik R, Abrahamsson H, Stotzer P O. Gender differences in gut transit shown with a newly developed radiological procedure. Scand J Gastroenterol 20033836–42. [DOI] [PubMed] [Google Scholar]
- 110.Pimentel M, Soffer E E, Chow E J.et al Lower frequency of MMC is found in IBS subjects with abnormal lactulose breath test, suggesting bacterial overgrowth. Dig Dis Sci 2002472639–2643. [DOI] [PubMed] [Google Scholar]
- 111.Pimentel M, Constantino T, Kong Y.et al A 14‐day elemental diet is highly effective in normalizing the lactulose breath test. Dig Dis Sci 20044973–77. [DOI] [PubMed] [Google Scholar]
- 112.King T S, Elia M, Hunter J O. Abnormal colonic fermentation in irritable bowel syndrome. Lancet 19983521187–1189. [DOI] [PubMed] [Google Scholar]
- 113.Dear K L, Elia M, Hunter J O. Do interventions which reduce colonic bacterial fermentation improve symptoms of irritable bowel syndrome? Dig Dis Sci 200550758–766. [DOI] [PubMed] [Google Scholar]