Abstract
Background and aims
Despite occasional positive reports on the efficacy of acupuncture (AC) on functions of the gastrointestinal tract, there is no conclusive evidence that AC is effective in the treatment of irritable bowel syndrome (IBS).
Patients and methods
Forty three patients with IBS according to the Rome II criteria were randomly assigned to receive either AC (n = 22) or sham acupuncture (SAC) (n = 21) using the so‐called “Streitberger needle”. Treatment duration was 10 sessions with an average of two AC sessions per week. The primary end point was improvement in quality of life (QOL) using the functional digestive diseases quality of life questionnaire (FDDQL) and a general quality of life questionnaire (SF‐36), compared with baseline assessments. QOL measurements were repeated three months after treatment.
Results
Both the AC and SAC groups improved significantly in global QOL, as assessed by the FDDQL, at the end of treatment (p = 0.022), with no differences between the groups. SF‐36 was insensitive to these changes (except for pain). This effect was partially reversed three months later. Post hoc comparison of responders and non‐responders in both groups combined revealed a significant prediction of the placebo response by two subscales of the FDDQL (sleep, coping) (F = 6.746, p = 0.003) in a stepwise regression model.
Conclusions
Acupuncture in IBS is primarily a placebo response. Based on the small differences found between the AC and SAC groups, a study including 566 patients would be necessary to prove the efficacy of AC over SAC. The placebo response may be predicted by high coping capacity and low sleep quality in individual patients.
Keywords: irritable bowel syndrome, acupuncture, sham acupuncture, quality of life, placebo response
Complementary medical procedures are increasingly popular in the Western world,1 and acupuncture (AC) in particular is frequently used, despite the fact that its efficacy has been demonstrated in only a few diseases.2 The strongest evidence has been found with postoperative and other forms of nausea and vomiting,2 and in the treatment of pain.3 Studies have shown that AC modulates the endorphin system4 via central pain processing pathways.5
AC has also been widely used in functional gastrointestinal disorders, such as irritable bowel syndrome (IBS).6 This frequent disorder7 still lacks an effective drug treatment for many patients in many parts of the world,8 while alternative medicine offers treatment options for all suffering patients.9
Previous studies of AC in IBS have not provided conclusive evidence of its efficacy.10 In a study by Chan and colleagues,11 immediate improvement of symptoms was seen in seven patients but this pilot study did not include a control group. A randomised controlled study in 25 patients12 did not find AC effective but employed atypical AC treatment with a single AC point. A data set published as an abstract only13 reported symptomatic improvement in both AC and placebo AC groups to a similar degree, but randomisation, choice of AC points, and long term effects remained obscure. In addition to these clinical trials, AC has been found to affect a variety of intestinal functions14,15,16,17 but also to produce high placebo responses.13,18
Placebo responses in IBS are known to be as high as 80% in single trials, with an average response rate of approximately 40%,19 depending, among other things, on the amount of patient‐doctor contact during the trial.20 Predictors of a placebo response are currently not known19 and require analysis of individual data21 rather than the meta‐analysis of published trials.22
The purpose of the present study was thus twofold: to test the efficacy of AC following the rules of traditional Chinese medicine (TCM) in comparison with sham AC (SAC = placebo acupuncture)23 in patients with IBS, and to identify individual predictors of a placebo response in patients receiving SAC.
Methods
Study design
The study was performed as a randomised placebo controlled trial. Block randomisation was done by a central telephone centre so that neither the patient nor the investigator (AS) knew whether the patient would receive AC or SAC. The randomisation result was told to the acupuncturist (SB, CW) directly after informed consent. Prior to treatment, immediately after its termination, and three months later patients were send a questionnaire requesting health related quality of life (QOL) information. The questionnaire evaluator (AS) was also blinded as to whether patients had received AC or SAC.
Based on literature findings, a medium sized effect was expected.11,12 Therefore, we intended to include 62 patients to detect a clinically relevant difference of 10 points on the functional digestive diseases quality of life questionnaire (FDDQL) scale with a power of 80%, based on a standard deviation of 14 and a type I error of 5%.
Setting and patients
Patients were recruited at the outpatient clinic of the Department of Gastroenterology, University Medical Hospital, via gastroenterology specialists in private practice in the Heidelberg area, and via advertisements in local newspapers. The recruitment period was from April 2003 to April 2004. Patients were at least 18 years of age and fulfilled the Rome II classification for IBS with symptoms present for at least 12 weeks out of the last 12 months. Diagnosis was confirmed by the presence of abdominal pain/discomfort with at least two of the following features: symptom relieve with defecation and/or symptoms associated with a change in frequency of stools, and/or associated with a change in form (appearance) of stools, in the absence of structural or metabolic abnormalities to explain the symptoms.24
A diagnosis of IBS had to exclude other causes of symptoms, such as inflammatory bowel diseases, carbohydrate malabsorption, and colon cancer. Colonoscopy had to have been performed within the last five years. Patients were excluded if they had an insufficient diagnostic workup, received AC treatment within the last three months, were receiving concomitant medication with effects on the gut, such as 5‐HT3 antagonists or spasmolytics, or were pregnant.
Compliance with the Rome II criteria was tested using the bowel disease questionnaire (BDQ)25 and by assessing symptoms during history taking. Patients received a psychometric test (patients' health questionnaire (PHQ‐D)) to verify the diagnosis on the subscales depression, somatisation, and anxiety.26
The local ethics committee approved the study protocol and patients had to give written informed consent prior to enrolment.
Intervention
Each patient was scheduled for a total of 10 AC/SAC sessions, twice a week, over five weeks. AC treatment was performed as standardised AC according to TCM. From the point of view of TCM, the core problem of IBS is an “affection of the spleen”, which could be explained by different so‐called “patterns”. For our study, the most important patterns, according to TCM, were “weakness of the spleen caused by stagnation of liver qi”, “weakness of the spleen qi”, and “weakness of the spleen and kidney”. We tried to derive a global concept to include all of these patterns into therapy. According to Chinese textbooks, IBS could be defined as follows: “suppressed emotions and concerns would induce a liver qi stagnation, which in turn would lead to an attack of the liver on the spleen and stomach. The resulting weakness of the spleen leads to digestion problems. Furthermore, liver qi stagnation would block qi flow in the meridians. This would induce abdominal pain”.27,28
Based on this concept, a fixed selection of AC points was used in all patients, comprising the most important points to treat the “weakness of the spleen” (basic pattern) and to strengthen digestion (table 1). The rules of TCM would have been best met if individual therapeutic schemes had been used. This was avoided to allow statistical comparison between groups and to keep the placebo effect as small as possible, as individualised treatment would amplify patient‐doctor interactions.
Table 1 Selection of acupuncture (AC) points; each patient was acupunctured at the same points. Sham AC was performed at locations in close proximity, 2 cm apart.
| AC point | Anatomical location | Function according to TCM |
|---|---|---|
| Liver 3 | Proximal angle between os metatarsal I and II | “Calms down the liver” |
| Stomach 36 | 5 cm below patella, 2 cm lateral of the tibial rim | “Strengthens spleen and stomach” |
| Spleen 6 | 5 cm above the medial malleolus, dorsal tibial rim | |
| Conception 12 | Middle between navel and sternum | “Removes stomach stagnation” |
| Stomach 21 | 3 cm lateral of conception 12 | |
| Stomach 25 | 3 cm lateral of navel | |
| Heart 7 | In the angle between os pisiform and radial side of the tendon of m flexor carpi ulnaris | “Calms down the mind” |
| Du Mai 20 | On the midline of the head, approximately on the midpoint of the line connecting the apexes of the two auricles |
TCM, traditional Chinese medicine.
AC was performed by an experienced female acupuncturist (SB) and by a trained female research assistant (CW). A stainless steel needle (0.32×30 mm; Asia Med, Munich, Germany) was inserted through a plaster over the respective AC points, under which a plastic ring was positioned. Care was taken that with needle insertion at each AC point, a dull needling sensation (called: de qi) occurred, that usually vanished during the course of a session.
In the control group, patients received SAC with a blunted telescopic placebo needle (Asia Med) that simulates an AC procedure without penetrating the skin.23 The efficiency of this method has been shown in various studies.29,30 Each SAC procedure was performed 2 cm adjacent to the real AC point to avoid acupressure effects. In the SAC group, the AC point LG 20 was not needled as fixation of the plaster is not possible on the head due to hair.
Measurements
The BDQ25 has been developed to validate symptom clusters in IBS in different nations. It was used here to confirm the diagnosis of IBS according to the Rome criteria in each patient prior to entry into the study. Psychological comorbidity was assessed at baseline by the subscales depression, anxiety, and somatisation of the PHQ‐D, which diagnoses psychological disorders using the diagnostic criteria from the DSM‐IV.26
Patients completed two QOL questionnaires that were used to assess any effects of symptomatic improvement by AC on their overall QOL: (a) FDDQL31 assesses disease related impact of bowel symptoms on quality of life, measured with 43 items on eight subscales: daily activity disease related anxiety, diet, sleep, discomfort, health perception, coping with disease, and impact of stress. Scores for subscales are added to a global QOL scale ranging from 0 to 100. FDDQL has an internal consistency of 0.94 (Crohnbach's alpha); (b) the health related quality of life questionnaire (SF‐36)32 is a validated global measure of health related quality of life unrelated to specific diseases that has been widely used in a variety of diseases.33 It uses 36 items to assess eight scales (bodily function, bodily role, bodily pain, general health, vitality, social function, emotional role, and physical well being).
Both questionnaires were given prior to treatment (t1), immediately after 10 AC treatments (t2 = five weeks after the first treatment), and three months after the last treatment (t3). Improvement in the global score of FDDQL immediately after the 10 treatments (t2) was the primary end point of the study. The other subscales of the FDDQL and the SF‐36 were defined as secondary end points. Outcome measures at t3 were also defined as secondary end points. Baseline differences between the two cohorts were tested using the t test and the χ2 test when appropriate. An ANOVA model adjusted for baseline scores was used to test group differences related to the primary end point (FDDQL) at week 5 and the secondary end point at week 12. In addition, a repeated measures ANOVA model with an unstructured covariance matrix was used to investigate the difference in the time pattern of the FDDQL and its subscales.
As trials with IBS patients usually report high placebo response rates,19 it was intended to perform a post hoc analysis on potential predictors of a placebo response using stepwise (forward selection) multiple regression analysis of baseline psychometric and sociometric data to identify responders and non‐responders of treatment. Responders were defined as patients in whom the change in the global FDDQL from baseline to week 5 was higher than the median change of the entire group.
All statistical testing was performed using the programs SPSS version 11.0 and SAS version 8.2 under Windows. The level of significance was set at 0.05 for all tests.
Results
Patients
A total of 43 patients were entered into the study. Eleven (26%) patients were recruited from the outpatient clinic, one patient via a private practice, and 31 (72%) by advertisements. Patients were randomly assigned to either the AC or SAC group. Only one patient in the entire study population had received AC in the past. She was able to identify SAC and declined to participate in the study after the third treatment. Another female patient declined to participate after five treatments due to time constraints. Thus two patients dropped out during the course of the study. There were no differences in age or sex between the groups at entry (table 2). The intended number of 60 patients could not be obtained despite multiple advertisements in local newspapers. Therefore, we decided to stop the trial after one year and to conduct the final analysis. Discontinuation of the trial was not data driven.
Table 2 Characteristics of the patients (bowel disease questionnaire).
| Characteristic | AC | SAC |
|---|---|---|
| No of subjects | 22 | 21 |
| Dropouts (n (%)) | 1 (4.5%) | 1 (4.5%) |
| Age (y) (mean (SD)) | 47.63 (14.71) | 47.14 (16.01) |
| Females (n (%)) | 17 (77.3%) | 17 (81.0%) |
| Did you suffer from intestinal pain/discomfort during the last year? (n (%)) | 22 (100%) | 20 (95.2%) |
| Did you consult a doctor for these complaints? (n (%)) | 14 (63.6%) | 13 (61.9%) |
| Does it happen frequently that you have to run for the bathroom? (n (%)) | 13 (59.1%) | 12 (57.1%) |
| Do you suffer from a bloated abdomen? (n (%)) | 20 (90.9%) | 20 (95.2%) |
| How would you describe your regular stool habits (n (%))? | ||
| Normal | 2 (9.1%) | 2 (9.5%) |
| Constipated | 3 (13.6%) | 2 (9.5%) |
| Diarrhoea | 8 (36.4%) | 9 (42.9%) |
| Constipation and diarrhoea alternating | 9 (40.9%) | 8 (38.1%) |
| How strong is your abdominal discomfort or pain? (n (%)) | ||
| Mild | 0 (0%) | 1 (4.5%) |
| Moderate | 7 (31.8%) | 5 (23.8%) |
| Strong | 12 (54.5%) | 11 (52.4%) |
| Very strong | 2 (9.1%) | 5 (23.8%) |
| On how many days during the last 12 months could you not perform your regular duties? (n (%)) | ||
| <3 days | 9 (40.9%) | 5 (23.8%) |
| 3–5 days | 5 (22.7%) | 4 (19.0%) |
| 6–10 days | 2 (9.1%) | 4 (19.0%) |
| >10 days | 5 (22.7%) | 8 (38.1%) |
| How long have you suffered from your intestinal complaints? (n (%)) | ||
| <2 y | 1 (4.5%) | 2 (9.5%) |
| 2–10 y | 8 (36.4%) | 6 (28.6%) |
| >10 y | 12 (54.5%) | 13 (61.9%) |
AC, acupuncture; SAC, sham acupuncture ( = placebo acupuncture).
Symptoms at study entry
The BDQ illustrates the degree and severity of bowel symptoms among the patients (table 2): two thirds had consulted a doctor for their symptoms during the past year, one third had had more than 10 days in the past year during which they could not perform their regular work, and more than half of the patients had a history of illness for 10 years or more. No differences were seen between those who received AC or SAC after assessment.
Quality of life with treatment
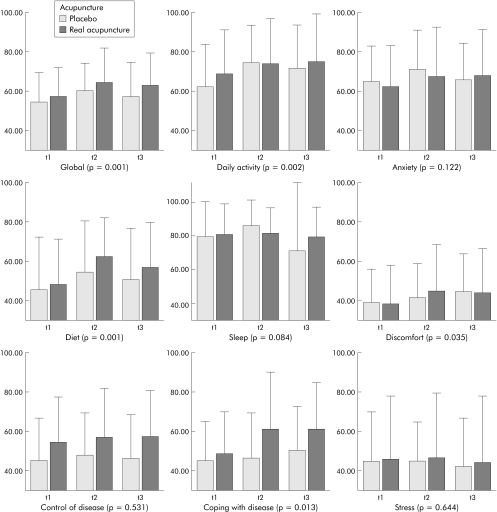
QOL, as measured by the FDDQL, improved with treatment and was significantly higher in comparison with baseline. Concerning the main outcome measurement immediately after 10 treatments (t2), the global FDDQL score increased significantly by 11% in the AC group and by 10% in the SAC group, and was moderately lower in both groups after three months of follow up (fig 1).
Figure 1 Scales of the functional digestive disease quality of life questionnaire in the placebo and real acupuncture groups (p value for change over time, using ANOVA with repeated measures). t1 = Before treatment, t2 = immediately after treatment (five weeks after t1), and t3 = 12 weeks after t2. Values are mean (SEM).
The global score revealed no difference between the groups immediately after 10 treatments (mean difference 1.98 (−3.59 to 7.38); p = 0.489, ANOVA with baseline adjustment) and three months later (mean difference 3.41 (−3.02 to 9.83); p = 0.283, ANOVA with baseline adjustment) (table 3). In both groups a significant time effect was seen (p = 0.001, ANOVA with repeated measures) (fig 1) but no interaction between time and treatment group (p = 0.565; not in fig 1). Therefore, the change over time did not seem to be affected by verum or placebo AC.
Table 3 Group differences in the functional digestive disease quality of life (FDDQL) subscales.
| FDDQL | Immediately after treatment (t2) | 3 months after treatment (t3) | ||
|---|---|---|---|---|
| Group difference | 95% CI | Group difference | 95% CI | |
| Daily activity | −3.87 | −13.63 to 5.89 | −1.18 | −10.51 to 8.16 |
| Anxiety | −2.02 | −12.25 to 8.21 | 3.96 | −4.92 to 12.83 |
| Diet | 6.06 | −2.44 to 14.56 | 4.12 | −6.24 to 14.48 |
| Sleep | −3.78 | −9.72 to 2.16 | 8.36 | −10.39 to 27.12 |
| Discomfort | 4.68 | −2.27 to 11.63 | 0.71 | −7.37 to 8.79 |
| Control of disease | −0.70 | −7.33 to 5.94 | 2.22 | −5.76 to 10.19 |
| Coping with disease | 11.6 | −0.72 to 23.99 | 7.98 | −3.19 to 19.14 |
| Stress | −0.19 | −9.75 to 9.37 | 0.13 | −11.73 to 11.99 |
| Global | 1.98 | −3.59 to 7.38 | 3.41 | −3.01 to 9.83 |
Calculation based on ANOVA with baseline adjustment.
Positive values: AC better than SAC; negative values: SAC better than AC.
95% CI, 95% confidence interval.
With respect to secondary outcome measurements, some FDDQL subscales also showed a significant improvement in both groups immediately after 10 treatments (t2), such as daily activity index, which improved by approximately 7% and 16% (AC and SAC, respectively), diet (23% and 16%), discomfort (14% and 6% ), and disease coping (21% and 3%). These effects were stable for three months except for diet which decreased at follow up (t3) (fig 1). All of the other FDDQL subscales (anxiety, sleep, control of disease, and stress) did not respond significantly to treatment. Analysis (ANOVA with baseline adjustment) of all subscales showed no significant group differences between AC and SAC in improvement of quality of life (table 3).
Overall, no significant difference was found in treatment effects in relation to the acupuncturists who performed the AC/SAC.
SF‐36 scales showed a similar trend as the FDDQL scales. However, only the bodily pain scale was significantly improved in both groups after treatment (12% in AC, 10% in SAC) but there was no difference between the AS and SAC groups (data not shown).
If the trial had been planned with one interim analysis after 40 patients, 526 (in addition to the 40) patients for the second stage should have been recruited to reach a conditional power of 80%. This number is based on the same primary end point after 10 treatments, a simple t test approach with an adaptive Pocock design,34 and assuming the same effect size for the second stage. With an additional 20 patients a conditional power of only 5% could have been reached.
Post hoc placebo analysis
As the AC group was not different from the SAC group, the post hoc analysis for potential predictors of the placebo response was performed on both groups together to increase the statistical power.
The average change in the global FDDQL scale was 5.02 (1.28) (mean (SEM); median: 4.46) and approximately followed a normal distribution, with a range between −15 and +25. According to the definition, 19 patients were identified as responders and 24 as non‐responders.
Comparing all variables at entry between these two groups identified five potential predictors of the placebo response: the subscales sleep and coping of the FDDQL, and the PHQ‐D subscales depression, anxiety, and somatisation. They were entered into a stepwise (forward) multiple regression model, together with the grouping variable (AC/sham AC). The variables sleep and coping remained significant factors predicting responsiveness to placebo (t = −2.945, p = 0.005 and t = 2.672, p = 0.011, respectively). A model with these two variables had a combined power of F = 6.764, p = 0.003 to explain responsiveness to AC/sham AC.
Discussion
To date, this is the largest randomised controlled trial of AC treatment for IBS. We found that there was a significant improvement in global quality of life of up to 11% in both AC and SAC treated patients, which is similar to effect sizes achieved with psychotherapeutic interventions35,36 and also with antidepressants.35 In particular the scales “coping with disease” and “diet” increased by more than 20%, as well as the daily activity index and the discomfort experienced. This effect decreased moderately after three months. As no differences between the AC and SAC groups were found, these effects must be seen as placebo responses. This is in contrast with previous studies which have shown physiological effects of AC (for example, for pain treatment during colonoscopy37 and gastroscopy).38 Effects were also found for visceral reflex activity15 and acid secretion in the stomach.14
Our new method was the performance of SAC, 2 cm adjacent to the AC points, thus excluding acupressure effects in the control group. In previous studies, this has often been a concern as acupressure may also induce physiological effects.39,40 Despite being the largest AC trial in IBS, the critical issue is the small sample size. Nevertheless, calculation of conditional power showed that a very high additional sample, with 566 patients in total, would be needed to achieve significance. It may be speculated as to whether standardisation of AC instead of an individualised AC strategy in the present study may be the reason for the lack of efficacy.41,42 On the other hand, the placebo effect due to intensive patient‐doctor interaction during the diagnosis and treatment might be smaller within a standardised procedure. There is no evidence that an individual AC treatment has greater efficacy than a standardised concept. A recently published large randomised controlled trial of AC treatment of migraines does not strengthen the hypothesis that individual AC is superior.43 In this study, the effectiveness of individualised AC was equal to SAC, but both were more effective than a waiting list control. One reason for the high placebo response could be the personal intensive attribution during the AC treatment, combined with the option for the patient to relax in unusually calm surroundings. Additionally, AC is known to establish a close doctor‐patient relationship. This could be explained by the composition of an explicit “handling” as a treatment strategy and implicit signalling of an holistic understanding of the patient's problems. This might be due to the hypothesised unknown incidental effects in complex interventions such as AC treatment.44 The importance of professional attention is underscored by the influence of psychological factors on the development and course of the disease.45,46 Assuming that the increase in QOL in both groups is due to a strong placebo effect known to exist in functional bowel disorders19,20,47 for any type of treatment, and similar to other medical conditions,48,49 our post hoc data analysis provides the first clue as to what the potential determinants of these placebo responses may be: among the psychometric variables of QOL assessed prior to study entry, high disease coping capacities were linked positively to being a placebo responder, while poor sleep quality was associated with being a placebo non‐responder. Other variables that may influence placebo responses are suggestions and expectations,50 cognitions,51 suggestibility,51,52 and an external “locus of control”53 and other “personality” factors. Also, perception of bodily sensations seems to play some form of role54 but this needs to be shown in a prospective way in future trials.
Identification of any predictor of the placebo response has not been shown in IBS patients to date, and meta‐analyses of published treatment trials in IBS20 as well as other diseases do not allow for such a conclusion, as published data sets normally do not include such variables. It has been claimed that for other conditions (for example, depression), more individualised data are necessary to identify reliable predictors of the placebo response.21
In summary, the effects of AC in IBS seem to be due to placebo effects when proper control of AC by a novel sham AC needle is used. Based on the small differences found between AC and SAC, a study using individual TCM patterns with 566 patients would be necessary to prove efficacy. The question is whether such a difference would be clinically relevant. The placebo response in both AC and SAC may be linked to individual psychological variables such as coping that can be assessed prior to treatment. The placebo responsiveness of an individual may thus become predictable in future trials.
Conflict of interest: declared (the declaration can be viewed on the Gut website at http://www.gutjnl.com/supplemental).
Supplementary Material
Acknowledgements
The trial was financially supported by the German Medical Acupuncture Association (DÄGfA). The funding source had no involvement in design, performance, or analysis of the study.
Abbreviations
AC - acupuncture
BDQ - bowel disease questionnaire
FDDQL - functional digestive diseases quality of life questionnaire
IBS - irritable bowel syndrome
PHQ‐D - patients' health questionnaire (German version)
QOL - quality of life
SAC - sham acupuncture ( = placebo acupuncture)
SF‐36 - health related quality of life questionnaire
TCM - traditional Chinese medicine
Footnotes
Conflict of interest: declared (the declaration can be viewed on the Gut website at http://www.gutjnl.com/supplemental).
References
- 1.Kessler R C, Davis R B, Foster D F.et al Long‐term trends in the use of complementary and alternative medical therapies in the United States. Ann Intern Med 2001135262–268. [DOI] [PubMed] [Google Scholar]
- 2.NIH Consensus Conference Acupuncture. JAMA 19982801518–1524. [PubMed] [Google Scholar]
- 3.Kaptchuk T J. Acupuncture: theory, efficacy, and practice. Ann Intern Med 2002136374–383. [DOI] [PubMed] [Google Scholar]
- 4.Han J S. Acupuncture and endorphins. Neurosci Lett 2004361258–261. [DOI] [PubMed] [Google Scholar]
- 5.Hui K K, Liu J, Makris N.et al Acupuncture modulates the limbic system and subcortical gray structures of the human brain: evidence from fMRI studies in normal subjects. Hum Brain Mapp 2000913–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ouyang H, Chen J D. Review article: therapeutic roles of acupuncture in functional gastrointestinal disorders. Aliment Pharmacol Ther 200420831–841. [DOI] [PubMed] [Google Scholar]
- 7.Drossman D A, Whitehead W E, Camilleri M. Irritable bowel syndrome: a technical review for practice guideline development. Gastroenterology 19971122120–2137. [DOI] [PubMed] [Google Scholar]
- 8.Quartero A O, Meineche‐Schmidt V, Muris J.et al Bulking agents, antispasmodic and antidepressant medication for the treatment of irritable bowel syndrome. Cochrane Database Syst Rev 2005(2)CD003460. [DOI] [PubMed]
- 9.Spanier J A, Howden C W, Jones M P. A systematic review of alternative therapies in the irritable bowel syndrome. Arch Intern Med 2003163265–274. [DOI] [PubMed] [Google Scholar]
- 10.Sung J J. Acupuncture for gastrointestinal disorders: myth or magic. Gut 200251617–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chan J, Carr I, Mayberry J F. The role of acupuncture in the treatment of irritable bowel syndrome: a pilot study. Hepatogastroenterology 1997441328–1330. [PubMed] [Google Scholar]
- 12.Fireman Z, Segal A, Kopelman Y.et al Acupuncture treatment for irritable bowel syndrome. A double‐blind controlled study. Digestion 200164100–103. [DOI] [PubMed] [Google Scholar]
- 13.Lowe C, Depew W T, Vanner S J. A placebo‐controlled, double‐blind trial of acupuncture in the treatment of irritable bowel syndrome. Gastroenterology 20002000A3168 [Google Scholar]
- 14.Jin H O, Zhou L, Lee K Y.et al Inhibition of acid secretion by electrical acupuncture is mediated via beta‐endorphin and somatostatin. Am J Physiol 1996271G524–G530. [DOI] [PubMed] [Google Scholar]
- 15.Li P, Rowshan K, Crisostomo M.et al Effect of electroacupuncture on pressor reflex during gastric distension. Am J Physiol Regul Integr Comp Physiol 2002283R1335–R1345. [DOI] [PubMed] [Google Scholar]
- 16.Li Y, Tougas G, Chiverton S G.et al The effect of acupuncture on gastrointestinal function and disorders. Am J Gastroenterol 1992871372–1381. [PubMed] [Google Scholar]
- 17.Lux G, Hagel J, Backer P.et al Acupuncture inhibits vagal gastric acid secretion stimulated by sham feeding in healthy subjects. Gut 1994351026–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rohrbock R B, Hammer J, Vogelsang H.et al Acupuncture has a placebo effect on rectal perception but not on distensibility and spatial summation: a study in health and IBS. Am J Gastroenterol 2004991990–1997. [DOI] [PubMed] [Google Scholar]
- 19.Enck P, Klosterhalfen S. The placebo response in functional bowel disorders: Perspectives and putative mechanisms. Neurogastroenterol Motil 200517325–331. [DOI] [PubMed] [Google Scholar]
- 20.Patel S M, Stason W B, Legedza A.et al The placebo effects in irritable bowel syndrome (IBS) trials—A meta‐analysis. Neurogastroenterol Motil 200517332–340. [DOI] [PubMed] [Google Scholar]
- 21.Welge J A, Keck P E., Jr Moderators of placebo response to antipsychotic treatment in patients with schizophrenia: a meta‐regression. Psychopharmacology (Berl) 20031661–10. [DOI] [PubMed] [Google Scholar]
- 22.Moayyedi P. Meta‐analysis: Can we mix apples and oranges? Am J Gastroenterol 2004992297–2301. [DOI] [PubMed] [Google Scholar]
- 23.Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet 1998352364–365. [DOI] [PubMed] [Google Scholar]
- 24.Thompson W G, Longstreth G F, Drossman D A.et al Functional bowel disorders and functional abdominal pain. Gut 199945(suppl 2)II43–II47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Talley N J, Holtmann G, Agreus L.et al Gastrointestinal symptoms and subjects cluster into distinct upper and lower groupings in the community: a four nations study. Am J Gastroenterol 2000951439–1447. [DOI] [PubMed] [Google Scholar]
- 26.Lowe B, Spitzer R L, Grafe K.et al Comparative validity of three screening questionnaires for DSM‐IV depressive disorders and physicians' diagnoses. J Affect Disord 200478131–140. [DOI] [PubMed] [Google Scholar]
- 27.Cheng Xinnong Chinese acupuncture and moxibustion. Beijing: Foreign Language Press, 1987
- 28.Maciocia G.The foundations of Chinese medicine. London: Churchill Livingstone, 1989
- 29.Kleinhenz J, Streitberger K, Windeler J.et al Randomised clinical trial comparing the effects of acupuncture and a newly designed placebo needle in rotator cuff tendinitis. Pain 199983235–241. [DOI] [PubMed] [Google Scholar]
- 30.Streitberger K, Diefenbacher M, Bauer A.et al Acupuncture compared to placebo‐acupuncture for postoperative nausea and vomiting prophylaxis: A randomised placebo‐controlled patient and observer blind trial. Anaesthesia 200459142–149. [DOI] [PubMed] [Google Scholar]
- 31.Chassany O, Marquis P, Scherrer B.et al Validation of a specific quality of life questionnaire for functional digestive disorders. Gut 199944527–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ware J E, Jr, Sherbourne C D. The MOS 36‐item short‐form health survey (SF‐36). I. Conceptual framework and item selection. Med Care 199230473–483. [PubMed] [Google Scholar]
- 33.Radoschewski M, Bellach B M. The SF‐36 in the Federal Health Survey—possibilities and requirements for application at the population level. Gesundheitswesen 199961S191–S199. [PubMed] [Google Scholar]
- 34.Lehmacher W, Wassmer G. Adaptive sample size calculations in group sequential trials. Biometrics 1999551286–1290. [DOI] [PubMed] [Google Scholar]
- 35.Drossman D A, Toner B B, Whitehead W E.et al Cognitive‐behavioral therapy versus education and desipramine versus placebo for moderate to severe functional bowel disorders. Gastroenterology 200312519–31. [DOI] [PubMed] [Google Scholar]
- 36.van Dulmen A M, Fennis J F, Bleijenberg G. Cognitive‐behavioral group therapy for irritable bowel syndrome: effects and long‐term follow‐up. Psychosom Med 199658508–514. [DOI] [PubMed] [Google Scholar]
- 37.Li C K, Nauck M, Loser C.et al Acupuncture to alleviate pain during colonoscopy. Dtsch Med Wochenschr 1991116367–370. [DOI] [PubMed] [Google Scholar]
- 38.Cahn A M, Carayon P, Hill C.et al Acupuncture in gastroscopy. Lancet 19781182–183. [DOI] [PubMed] [Google Scholar]
- 39.Streitberger K, Friedrich‐Rust M, Bardenheuer H.et al Effect of acupuncture compared with placebo‐acupuncture at p6 as additional antiemetic prophylaxis in high‐dose chemotherapy and autologous peripheral blood stem cell transplantation: a randomized controlled single‐blind trial. Clin Cancer Res 200392538–2544. [PubMed] [Google Scholar]
- 40.White P, Lewith G, Hopwood V.et al The placebo needle, is it a valid and convincing placebo for use in acupuncture trials? A randomised, single‐blind, cross‐over pilot trial. Pain 2003106401–409. [DOI] [PubMed] [Google Scholar]
- 41.McCarney R W, Brinkhaus B, Lasserson T J.et al Acupuncture for chronic asthma. Cochrane Database Syst Rev 2004(1)CD000008. [DOI] [PMC free article] [PubMed]
- 42.Patel M, Gutzwiller F, Paccaud F.et al A meta‐analysis of acupuncture for chronic pain. Int J Epidemiol 198918900–906. [DOI] [PubMed] [Google Scholar]
- 43.Linde K, Streng A, Jürgens S.et al Acupuncture for patients with migraine. JAMA 20052932118–2125. [DOI] [PubMed] [Google Scholar]
- 44.Paterson C, Dieppe P. Characteristic and incidental (placebo) effects in complex interventions such as acupuncture. BMJ 20053301202–1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gwee K A, Leong Y L, Graham C.et al The role of psychological and biological factors in postinfective gut dysfunction. Gut 199944400–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Posserud I, Agerforz P, Ekman R.et al Altered visceral perceptual and neuroendocrine response in patients with irritable bowel syndrome during mental stress. Gut 2004531102–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Spiller R C. Problems and challenges in the design of irritable bowel syndrome clinical trials: experience from published trials. Am J Med 199910791–7S. [DOI] [PubMed] [Google Scholar]
- 48.de Craen A J, Moerman D E, Heisterkamp S H.et al Placebo effect in the treatment of duodenal ulcer. Br J Clin Pharmacol 199948853–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Walsh B T, Seidman S N, Sysko R.et al Placebo response in studies of major depression: variable, substantial, and growing. JAMA 20022871840–1847. [DOI] [PubMed] [Google Scholar]
- 50.Vase L, Robinson M E, Verne G N.et al The contributions of suggestion, desire, and expectation to placebo effects in irritable bowel syndrome patients. An empirical investigation. Pain 200310517–25. [DOI] [PubMed] [Google Scholar]
- 51.Kreitler S, Kreitler H, Carasso R. Cognitive orientation as predictor of pain relief following acupuncture. Pain 198728323–341. [DOI] [PubMed] [Google Scholar]
- 52.De Pascalis V, Chiaradia C, Carotenuto E. The contribution of suggestibility and expectation to placebo analgesia phenomenon in an experimental setting. Pain 200296393–402. [DOI] [PubMed] [Google Scholar]
- 53.Reynaert C, Janne P, Vause M.et al Clinical trials of antidepressants: the hidden face: where locus of control appears to play a key role in depression outcome. Psychopharmacology (Berl) 1995119449–454. [DOI] [PubMed] [Google Scholar]
- 54.Schneider A, Lowe B, Streitberger K. Perception of bodily sensation as a predictor of treatment response on acupuncture for postoperative nausea and vomiting. J Altern Complem Med 200511119–125. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.