Inflammatory bowel disease (IBD) confined to the diverticular tract—defined as segmental colitis associated with diverticula (SCAD)—occurs in 3.8% of diverticular patients.1 Recently, infliximab was reported to have a dramatic impact on severe Crohn's disease and ulcerative colitis therapy.2,3 However, tumour necrosis factor α (TNF‐α) involvement and the efficacy of anti‐TNF‐α in SCAD are unknown.
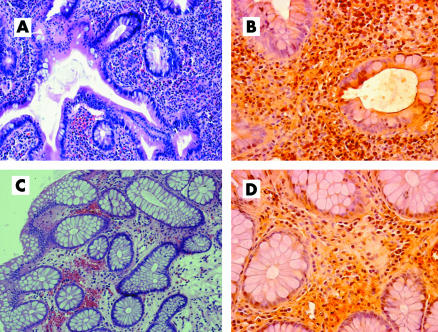
A 60 year old male smoker and non‐NSAID user was admitted for severe bloody diarrhoea. At colonoscopy, the sigmoid and descending mucosa showed granularity, friability, and erosions confined to the diverticular tract, without alterations of the remaining ileocolonic mucosa. Histology of the inflamed tract revealed an ulcerative colitis‐like picture. Therefore, a diagnosis of SCAD was made. After mesalazine and antibiotic failure, intravenous steroid therapy was successfully administered. After two years of steroid dependence, repeat endoscopy showed, in addition to the active SCAD, ulcerative colitis‐like involvement of the proximal non‐diverticular colon. Histology confirmed active SCAD, also showing severely active ulcerative colitis in the proximal colon, sparing the rectum and terminal ileum. A high dose steroid infusion achieved complete clinical remission, and azathioprine was started. After a further six months of steroid dependence, infliximab (5 mg/kg) was administered at 0, 2, and 6 weeks, and a steroid free complete clinical remission was achieved within one month. Maintenance treatment with infliximab every eight weeks has been successfully continued for up to 16 months of follow up. Ileocolonoscopy performed after one year from the beginning of infliximab revealed complete remission of SCAD, while a mild active colitis persisted in the proximal colon. Histology showed complete regression of SCAD but only a slight improvement in the proximal colon. TNF‐α label index (percentage of positive stained stromal cells to the total number of lamina propria mononuclear cells4) appeared to be markedly reduced in SCAD (40% v15%) while remaining unchanged in the proximal colon (32% v 30%) (fig 1).
Figure 1 Histological changes in colonic biopsies and tumour necrosis factor α (TNF‐α) expression before and after infliximab therapy (haematoxylin‐eosin and immunohistochemical stains; original magnification 125× and 400×). (A) Active segmental colitis associated with diverticula (SCAD) characterised by a dense inflammatory infiltrate, disturbed crypt architecture, and epithelial damage, and by high TNF‐α expression (B). (C) SCAD in remission characterised by regression of the inflammatory infiltrate, restoration of the epithelial damage, and profound downregulation of TNF‐α expression (D).
Increased TNF‐α concentrations have been reported in both Crohn's disease and ulcerative colitis.5,6 For the first time, this case report showed that TNF‐α overexpression was also present in SCAD. It is known that high TNF‐α levels detected in Crohn's disease are reduced by infliximab therapy.7 Similarly, a dramatic decrease in histological activity with profound TNF‐α downregulation in the SCAD tract occurred in our patient after infliximab. These observations suggest that SCAD pathogenesis may mirror the pathogenetic models proposed for IBD.
It has already been reported that SCAD can fade into a more classic ulcerative colitis picture.8 In our case, although the two IBD pictures presented with similar TNF‐α concentrations before therapy, complete endoscopic and histological regression was limited to the SCAD tract while only partial endoscopic improvement occurred in the non‐diverticular ulcerative colitis‐like picture. Interestingly, persistence of histological activity was associated with high TNF‐α expression. This is the first case in which two simultaneous varieties of IBD have shown a different response to infliximab in the same patient. However, due to the more aggressive clinical behaviour of the SCAD, infliximab therapy was successful in annihilating the long term steroid dependence of our patient. This implies that a much deeper knowledge of the pathogenesis of IBD needs to be pursued before preventing a patient from a potentially life saving therapy.
In conclusion, our case report showed that the pathogenesis of SCAD can be sustained by TNF‐α activity and reversed by specific therapy. Moreover, an associated ulcerative colitis may show a different degree of response to infliximab. Such different behaviours suggest that the more we struggle to unravel the inflammatory puzzle, the more puzzling the pathogenetic enigma of IBD appears to be.
Footnotes
Conflict of interest: None declared.
References
- 1.Koutroubakis I E, Antoniou P, Tzardi M.et al The spectrum of segmental colitis associated with diverticulosis. Int J Colorectal Dis 20052028–32. [DOI] [PubMed] [Google Scholar]
- 2.Sandborn W J, Faubion W A. Biologics in inflammatory bowel disease: how much progress have we made? Gut 2004531366–1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jarnerot G, Hertervig E, Friis‐Liby I.et al Infliximab as rescue therapy in severe to moderately severe ulcerative colitis: a randomized, placebo‐controlled study. Gastroenterology 20051281805–1811. [DOI] [PubMed] [Google Scholar]
- 4.Ierardi E, Monno R, Gentile A.et al Helicobacter heilmannii gastritis: a histological and immunohistochemical trait. J Clin Pathol 200154774–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murch S H, Braegger C P, Walker‐Smith J A.et al Location of tumour necrosis factor α by immunohistochemistry in chronic inflammatory bowel disease. Gut 1993341705–1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reinecker H ‐ C, Steffen M, Witthoeft T.et al Enhanced secretion of tumour necrosis factor‐alpha, IL‐6, and IL‐1b by isolated lamina propria mononuclear cells from patients with ulcerative colitis and Crohn's disease. Clin Exp Immunol 199394174–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baert F J, D'Haens G, Peeters M.et al Tumor necrosis factor α antibody (infliximab) therapy profoundly down‐regulates the inflammation in Crohn's ileocolitis. Gastroenterology 199911622–28. [DOI] [PubMed] [Google Scholar]
- 8.Imperiali G, Meucci G, Alvisi C.et al Segmental colitis associated with diverticula: a prospective study. Am J Gastroenterol 2000951014–1016. [DOI] [PubMed] [Google Scholar]