Coeliac disease (CD) is a common condition with many atypical manifestations and an estimated worldwide prevalence of 1 in 266.1 It often goes unrecognised because characteristic histopathological abnormalities must be found to confirm the diagnosis. Endoscopic signs of CD are described in the literature but cannot be relied upon for detection of the disease because their sensitivity and specificity are not high. To investigate CD in every patient undergoing oesophagogastroduodenoscopy (OGD) for dyspeptic symptoms is not realistic, especially if we consider the significant costs of histological handling. Therefore, a way of detecting CD is selection of patients in which biopsies of the duodenal mucosa must be performed.
A useful new medical technique, optical coherence tomography (OCT), that combines the principles of ultrasound and infrared backscattering light, enables detailed study of the microstructure of the first layers of the gastrointestinal wall, particularly the villous morphology. OCT is an imaging technique, similar to B‐mode ultrasound (US), but its resolution is far better (5–10 μm), closer to histology.2,3 The technique is similar to US imaging but uses light in place of sound waves. No data are currently available on the use of OCT in the small intestine and, in particular, in the diagnosis of CD. We tested the utility of OCT to confirm the diagnosis of CD in selected patients undergoing OGD for suspicion of disease.
The study protocol was approved by the institutional ethics committee. We prospectively enrolled 18 patients with serological suspicion of CD (group 1) and 22 who were undergoing OGD for dyspepsia, with negative antigliadin, antiendomysial, and antitransglutaminase antibodies (group 2). Mean age of group 1 was 30.9 years (range 21–69; 14 females and four males) and group 2, 39.2 years (range 23–75; 14 females and eight males). OCT scans of the descending duodenum were taken during diagnostic OGD by a far‐focus OCT probe (Pentax; Lightlab Imaging, Westford, Massachusetts, USA), with a diameter of 1.5 mm, a penetration depth of approximately 1 mm, and resolution of approximately 5–10 μm. We acquired multiple images of the second part of the duodenum, and biopsies were taken in the same area in which OCT was performed, one in each quadrant, according to the guidelines for the diagnosis of CD.
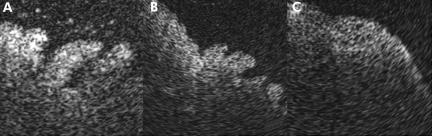
OCT images and histological specimens were evaluated blindly and independently by a gastroenterologist with experience in OCT, who was also blinded to the clinical data and endoscopic aspect of the duodenal mucosa, and by a pathologist. To compare villi morphology, we considered three patterns: 1, no atrophy (normal) (fig 1); 2, mild atrophy (type 3a Marsh); and 3, marked atrophy (type 3b Marsh).4 We found 100% agreement between OCT and histology for villi morphology in both groups (table 1).
Figure 1 Optical coherence tomography (OCT) patterns of normal (A), middle (B), and total (C) villous atrophy morphology (patterns 1, 2, and 3).
Table 1 Number (%) of control dyspeptic subjects (with negative coeliac disease (CD) serology) and patients with none, mild, or total villous atrophy, as shown by optical coherence tomography (OCT) and histology.
| Villous atrophy grade | Patients | Control group | ||
|---|---|---|---|---|
| OCT | Histology | OCT | Histology | |
| No villous atrophy | 6/18 (33.3%) | 6/18 (33.3%) | 22/22 (100%) | 22/22 (100%) |
| Mild atrophy | 11/18 (61.1%) | 11/18 (61.1%) | 0/22 (0%) | 0/22 (0%) |
| Total atrophy | 1/18 (5.6%) | 1/18 (5.6%) | 0/22 (0%) | 0/22 (0%) |
In conclusion, OCT identified intestinal villous morphology, and the degree of atrophy, with excellent accuracy compared with histology. Therefore, OCT appears to be a promising technique for selecting dyspeptic patients who need biopsies to detect CD, requiring only a few minutes to obtain the profile of duodenal villi. Its use in these patients could be high if one considers that a recent study showed that in patients with dyspepsia the specificity of endoscopic markers was high (92%) but sensitivity was low (59%).5 In the future, OCT could identify not only CD subjects but others undergoing OGD for conditions possibly related to CD, such as iron deficiency anaemia, osteoporosis, diabetes mellitus, and autoimmune diseases in which a misdiagnosis of CD is estimated to range from 0.7 to 8.7%.6,7
Footnotes
Conflict of interest: None declared.
References
- 1.Fasano A, Berti I, Gerarduzzi T.et al Prevalence of celiac disease in at‐risk and not at‐risk groups in the United States: a large multicentric study. Arch Inter Med 200363286–292. [DOI] [PubMed] [Google Scholar]
- 2.Huang D, Swanson E A, Lin C P.et al Optical coherence tomography. Science 19912541178–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jabbari M, Wild G, Goresky C A.et al Scalloped valvulae conniventes: an endoscopic marker of celiac sprue. Gastroenterology 1988951518–1522. [DOI] [PubMed] [Google Scholar]
- 4.Oberhuber G, Granditsch G, Vogelsang H. The histopathology of coeliac disease: time for a standardized report scheme for pathologists. Eur J Gastroenterol Hepatol 1999111185–1194. [DOI] [PubMed] [Google Scholar]
- 5.Oxentenko A S, Grisolano S W, Murray J A.et al The insensitivity of endoscopic markers in celiac disease. Am J Gastroenterol 200297933–938. [DOI] [PubMed] [Google Scholar]
- 6.Green P H, Murray J A. Routine duodenal biopsies to exclude celiac disease? Gastrointest Endosc 20035892–95. [DOI] [PubMed] [Google Scholar]
- 7.Mandal A K, Mehdi I, Munsi S K.et al Value of routine duodenal biopsy in diagnosing coeliac disease in patients with iron deficiency anaemia. Postgrad Med J 200480475–477. [DOI] [PMC free article] [PubMed] [Google Scholar]