Abstract
Background and aims
Early endoscopic recurrence is frequent after intestinal resection for Crohn's disease. Bacteria are involved, and probiotics may modulate immune responses to the intestinal flora. Here we tested the probiotic strain Lactobacillus johnsonii LA1 in this setting.
Patients and methods
This was a randomised, double blind, placebo controlled study. Patients were eligible if they had undergone surgical resection of <1 m, removing all macroscopic lesions within the past 21 days. Patients were randomised to receive two packets per day of lyophilised LA1 (2×109 cfu) or placebo for six months; no other treatment was allowed. The primary endpoint was endoscopic recurrence at six months, with grade >1 in Rutgeerts' classification or an adapted classification for colonic lesions. Endoscopic score was the maximal grade of ileal and colonic lesions. Analyses were performed primarily on an intent to treat basis.
Results
Ninety eight patients were enrolled (48 in the LA1 group). At six months, endoscopic recurrence was observed in 30/47 patients (64%) in the placebo group and in 21/43 (49%) in the LA1 group (p = 0.15). Per protocol analysis confirmed this result. Endoscopic score distribution did not differ significantly between the LA1 and placebo groups. There were four clinical recurrences in the LA1 group and three in the placebo group.
Conclusion
L johnsonii LA1 (4×109 cfu/day) did not have a sufficient effect, if any, to prevent endoscopic recurrence of Crohn's disease.
Keywords: Crohn's disease, randomised controlled trial, probiotics, lactobacillus
More than 70% of patients with Crohn's disease (CD) undergo surgical treatment during their lifetime.1 New lesions usually appear shortly after ileocolonic resection, followed by clinical recurrence and, eventually, new complications and further surgery.1 There is strong clinical evidence that luminal bacteria are involved in the occurrence of new lesions.2 Nitro imidazole antibiotics can prevent postoperative recurrence but their adverse effects limit their long term use.3,4 One attractive alternative is to manipulate the bacterial flora with probiotics,5 which can compete with the commensal and pathogenic flora and may influence local immune responses.5,6 Only two small clinical trials have tested probiotic prophylaxis of postoperative CD recurrence.7,8 VSL #3 was claimed to be effective but the results have not been reported in detail.7Lactobacillus rhamnosus GG was ineffective.8
Lactobacillus johnsonii LA1 (LA1) is a probiotic strain present in commercial fermented milks (LC1; Nestlé, Switzerland). Previous studies have shown that ingested LA1 survives during intestinal transit, generating ileal and faecal concentrations of approximately 106 colony forming units (cfu)/g.9 In vitro studies with CaCo2 cells, alone or cocultured with peripheral blood mononuclear cells, have shown that LA1 has lower proinflammatory properties than many other bacteria, and that it stimulates the production of transforming growth factor β.10
Here we report the results of a randomised placebo controlled trial designed to determine if LA1, given by mouth for a period of six months, could prevent or attenuate recurrent CD lesions after curative surgery.
Patients and methods
Objective and hypotheses
The objective of the trial was to demonstrate the efficacy of the LA1 strain to decrease the endoscopic recurrence rate six months after surgery by 30% compared with a 50% rate on placebo, when given at a concentration of 2×109 cfu twice a day for six months.
Patients
Patients were recruited between November 2002 and January 2004 by 16 centres belonging to the GETAID Study Group (Groupe d'Etude Thérapeutique des Affections Inflammatoires Digestives). CD was diagnosed on the basis of standard clinical, radiographic, endoscopic, and pathological criteria. Male and female patients aged at least 18 years of age were eligible to participate if they had: (a) undergone recent surgical resection for ileal, ileocolonic, or colonic CD, removing all macroscopic lesions, with an anastomosis which could be reached by ileocolonoscopy; (b) cumulative small bowel resection(s) of <1 m; and (c) no other intestinal resection during the previous five years.
Enrolment and treatment initiation had to occur within 21 days following resection. When a diverting stomy had been necessary at the time of intestinal resection, the patient could be included under the same conditions after its closure. A subgroup of patients participated in an ancillary substudy designed to assess the pharmacokinetics of LA1 and its effect on the local flora and cytokine production. Inclusion criteria were slightly more restrictive for this subgroup: patients had to have undergone ileal or ileocolonic resection (and not pure colonic resection) and to have received no antibiotic treatment during the week before enrolment. Finally, enrolment and treatment initiation had to occur three days before surgery in this subgroup.
Patients receiving antibiotics for more than two weeks and those treated with aminosalicylates or immunosuppressants for more than three weeks after surgery were not eligible, and neither were patients with any other disease or condition that might interfere with the study assessments (as judged by the investigator): patients who had participated in another clinical study in the previous 30 days; women of child bearing potential who were not using effective contraception; and pregnant or lactating women. Patients who underwent total or subtotal colectomy, intestinal bypass or stricturoplasty, stomy, carcinoma resection, or abscess drainage were also not eligible.
Study design
This was a double blind, randomised, placebo controlled, six month clinical study with two parallel groups of outpatients. In order to guarantee the comparability of the LA1 and placebo treated patients in the pharmacokinetic substudy, the study population was stratified for substudy participation. At the patient's selection visit, a specific form allowing verification of the inclusion and exclusion criteria was used by the investigator to request randomisation at the GETAID biostatistic centre. When all of these criteria were satisfied, randomisation was performed by this centre within each stratum per centre, using permutation tables of size 2 or 4, according to expected enrolment within each centre, each centre being blinded to the size of its blocks. Patient's treatment assignment, LA1 or placebo, was the first free treatment (not yet allocated) on the randomisation sheet corresponding to the patient's stratum and centre. Treatment number was the first free number with the corresponding treatment in a randomised list with treatment numbers and their corresponding treatment prepared by the biostatistic centre before trial initiation. Treatment number and patient identification (centre, stratum, patient number within the centre and stratum, initials) were sent to the investigator. The same information and allocated treatment were sent to the service in charge of drug delivery, allowing the service to check that treatment was in agreement with the predefined list. Treatment was sent by this service to the pharmacy of the centre with protocol identification and the patient's identification. Unblinding, if necessary, was made by a request to the biostatistic centre with a specific form. Randomisation sheets and list were regularly updated by the biostatistic centre with treatment number, treatment, patient identification, randomisation request date, and unblinding date, if any.
The study was approved by the HEGP‐Broussais ethics committee, and all the patients gave written informed consent prior to enrolment.
Treatments
Patients were randomised to receive two packets per day of lyophilised LA1 (2×109 cfu per packet) or placebo (maltodextrin) for six months. The packets had to be dissolved in half a glass of water just before consumption. Compliance with treatment was evaluated, either by pill counts when patients brought back unused medications at each visit or by patient interview. Adequate compliance was considered if it was estimated that at least 75% of the study drug had been taken. Corticosteroids were allowed if used before surgery but had to be withdrawn gradually within six weeks after surgery. Concomitant medication with the following drugs was not allowed: antibiotics for more than 15 days; aminosalicylates; glucocorticoids (after gradual withdrawal); non steroidal anti‐inflammatory drugs; immunosuppressive drugs; anti‐tumour necrosis factor agents; thalidomide; and other probiotics. Loperamide and cholestyramine were allowed.
Data collection and follow‐up
The following data were obtained at the time of inclusion (or just after surgery for patients enrolled three days before surgery): age, sex, smoking status, disease location, disease duration, previous surgery, type of resection and anastomosis, length of ileal resection, and disease behaviour. Disease behaviour was defined as penetrative or not according to the primary reason for surgery, based on clinical manifestations, preoperative explorations, and intraoperative findings. Penetrating disease included internal or external fistula formation, abscess, or acute free perforation. Study visits were planned at inclusion and three and six months after surgery, and if clinical signs of recurrence occurred. At each visit the CD activity index (CDAI) score11 was calculated from the patient's symptom diary card written during the previous week, and blood cell counts, C reactive protein (CRP), erythrocyte sedimentation rate, alanine aminotransferase, γ‐glutamyl transferase, and serum creatinine were determined. Ileocolonoscopy was performed at six months and in case of clinical recurrence.
Study endpoints
The endpoints were defined in the initial study protocol. The primary endpoint was endoscopic recurrence at six months, defined as grade >1 macroscopic lesions in the ileum or colon, using Rutgeerts' classification for ileal lesions1 and an adapted classification for colonic lesions as no specific classification was available for colonic lesions (table 1). Secondary endpoints included an endoscopic score (maximum of the ileum and colon grades) and clinical recurrence, defined as a CDAI score of 200 or more. Severe endoscopic recurrence, defined by an endoscopic score of more than 2, was chosen as an additional endpoint after study completion. Safety assessment was based on the reporting of adverse events and the recording of laboratory parameters.
Table 1 Grade of endoscopic recurrence.
| Ileal and ileocolonic anastomotic lesions1 | |
| i0 | No macroscopic lesions |
| i1 | Less than 5 aphthous ulcers (<5 mm) in the neoterminal ileum |
| i2 | More than 5 aphthous ulcers with normal mucosa between them, or ulceration(s) confined to the anastomosis |
| i3 | Diffuse aphthous ileitis with a diffusely inflamed ileum |
| i4 | Diffuse aphthous ileitis with larger ulcers, irregularity, and narrowing |
| Colonic lesions | |
| c0 | No macroscopic lesions |
| c1 | Less than 5 aphthous or superficial ulcerations per segment* or frank erythema or oedema without ulceration |
| c2 | More than 5 aphthous or superficial ulcerations on at least one colonic segment1 |
| c3 | Deep ulceration affecting less than 10% of the surface of the entire colon and less than 5 deep ulcerations in each colonic segment |
| c4 | Deep ulcerations affecting more than 10% of the surface of the colon, or more than 5 deep ulcerations in a colonic segment, or presence of strictures. |
*Caecum and ascending colon, transverse colon, descending and sigmoid colon, and rectum.
Statistical analysis
The hypothesis for the sample size calculation was an endoscopic recurrence rate of 50% at six months in the placebo group. In order to detect a 30% reduction in the endoscopic recurrence rate in the LA1 treatment arm, it was calculated that 48 patients per group had to be enrolled to guarantee a power of 80% in a two sided test with a type I error of 5%. Patients belonging to the two strata were pooled for the analysis of all endpoints, as stratification was not planned to detect a difference in treatment efficacy across the strata but rather to ensure comparability of the treatment groups in the substudy population.
Distributions of continuous and qualitative characteristics were described by using the median and interquartile range (IQR), and frequencies and proportions, respectively. Distributions were compared between treatment groups by using the Mann‐Whitney test, and the χ2 test or Fischer's exact test (as appropriate), respectively.
Patients were assigned to intent to treat (ITT), per protocol (PP), and safety populations prior to breaking the randomisation code. The primary efficacy analysis was based on the ITT population, which included all patients in whom the primary endpoint was assessable. Patients with major protocol deviations (use of corticosteroids; enrolment or treatment more than 27 days after resection; ileocoloscopy performed more than seven months after treatment initiation) or who consumed less than 75% of the assigned treatment were excluded from the PP population. The safety population comprised all patients who received at least one dose of the study treatment.
Differences in primary and secondary endpoints between treatment groups were analysed with the χ2 test and expressed as odds ratios (OR) and 95% confidence interval (95% CI), as estimated using a logistic regression model. For the primary endpoint, multivariate logistic regression model was used to study treatment effect adjusted on potential prognostic factors, especially those whose distributions were not well balanced between treatment groups. For smoking habits (an established factor of increased recurrence risk), the same method allowed us to test a possible different treatment effect across smoking habit categories. Data were analysed with SPSS Software for Windows Release 6.1 (SPSS Inc, Chicago, Illinois, USA).
Results
Study population
Demographic characteristics of the patients at baseline are shown in table 2. The two treatment groups were well matched, except for a higher proportion of patients who underwent ileal and colonic resection in the placebo group, and a higher median CRP level in the LA1 group.
Table 2 Characteristics of the patients at baseline according to treatment group (Lactobacillus johnsonii LA1 or placebo).
| LA1 (n = 48) | Placebo (n = 50) | |
|---|---|---|
| Age (y)† | 32 (27–42) | 29 (27–34) |
| Female sex‡ | 22 (46) | 29 (58) |
| Smoking status‡ | ||
| Current smoker | 14 (29) | 13 (26) |
| Ex‐smoker | 19 (40) | 17 (34) |
| Non smoker | 15 (31) | 20 (40) |
| Disease duration (months)† | 33 (4–99) | 24 (7–88) |
| Disease location‡ | ||
| Small bowel only | 29 (60) | 25 (50) |
| Ileocolon | 16 (33) | 24 (48) |
| Colon only | 3 (6) | 1 (2) |
| Previous surgery‡ | 7 (15) | 9 (18) |
| Type of resection‡* | ||
| Ileal | 6 (13) | 1 (2) |
| Ileocolonic | 40 (83) | 49 (98) |
| Colonic (segmental) | 2 (4) | 0 (0) |
| Steroid treatment | 19 (40) | 21 (42) |
| Length of resection (cm)† | 30 (21–47) | 30 (20–50) |
| Penetrating disease behaviour‡ | 20 (42) | 25 (50) |
| Temporary diverting stoma‡ | 10 (21) | 11 (22) |
| Time between surgery and enrolment (days)† | 13 (7–20) | 15 (8–19) |
| C reactive protein (mg/l)†* | 16 (4–41) | 8 (2–16) |
†Median (interquartile range).
‡n (%).
*p = 0.04.
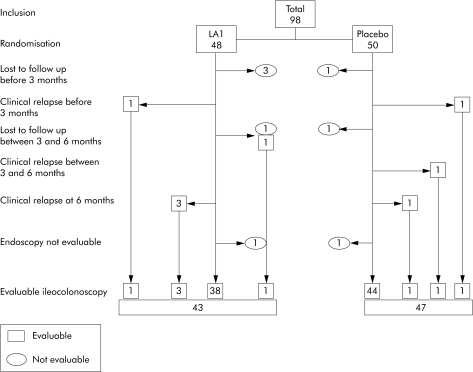
The trial profile is shown in fig 1. A total of 98 patients were enrolled (48 in the LA1 group and 50 in the placebo group). Forty three patients in the LA1 group and 47 patients in the placebo group were evaluated at six months or earlier for clinical recurrences. Four and two patients in the LA1 and placebo groups, respectively, were lost to follow up or withdrew their consent, and one patient in each group could not be evaluated as ileocoloscopy could not reach the anastomosis. One patient in the LA1 group was lost to follow up after the three month visit but was evaluated more than seven months after resection.
Figure 1 Study flow chart.
The PP population consisted of 78 patients (35 in the LA1 group and 43 in the placebo group). The remaining patients were excluded from the PP analysis for the following reasons: consumption of less than 75% of the study treatment (four patients in the LA1 group and three patients in the placebo group), unauthorised corticosteroid use (two patients in the LA1 group), inclusion more than 27 days after surgery (one patient in the LA1 group), and ileocoloscopy performed more than seven months after surgery (one patient in each group). The safety population comprised 47 and 49 patients in the LA1 and placebo groups, respectively. No unblinding was requested during the trial.
Efficacy
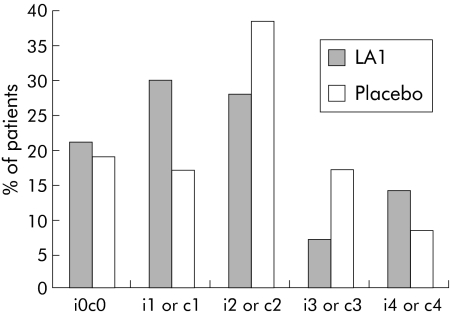
Recurrence (endoscopic score >1) was observed in 30 of 47 patients (64%) in the placebo group compared with 21 of 43 (49%) in the LA1 group (OR 1.85 (95% CI 0.80–4.30); p = 0.15). Endoscopic score distribution did not differ significantly between the LA1 and placebo groups (fig 2). Severe endoscopic recurrence was observed in 12 of 47 patients (26%) in the placebo group versus 9 of 43 (21%) in the LA1 group (OR 1.30 (95% CI 0.48–3.47); p = 0.61). Clinical recurrence was observed in four patients in the LA1 group (two of whom also had endoscopic recurrence) and in three patients receiving the placebo (all three of whom also had endoscopic recurrence). These results were confirmed in the PP population. Endoscopic recurrence was observed in 27 of 43 patients (63%) in the placebo group versus 17 of 35 (49%) in the LA1 group (OR 1.79 (95% CI 0.72–4.42); p = 0.21) whereas severe endoscopic recurrence was observed in 10 of 43 patients (23%) in the placebo group versus 7 of 35 (20%) in the LA1 group (OR 1.21 (95% CI 0.41–3.60); p = 0.73). In the subgroup of patients who began LA1 before surgery, endoscopic recurrence was observed in 6/10 patients in the placebo group compared with 6/9 in the LA1 group (p = 0.76).
Figure 2 Grade of endoscopic lesions (G0–4) at follow up (six months or earlier in case of clinical relapse) in patients receiving Lactobacillus johnsonii LA1 or placebo after surgery for Crohn's disease.
Treatment effect was not modified when adjusted for smoking habit (p = 0.12), CRP level relatively to 10 mg/l (p = 0.15), type of resection (p = 0.24), or stratum (p = 0.15). None of these factors were predictive of endoscopic recurrence. Treatment effect did not appear to be different across smoking status categories (p = 0.84).
Tolerability
Fifteen adverse events (AE) occurred in 12 patients (nine AE in six patients in the LA1 group and six AE in six patients in the placebo group). All AE consisted of digestive disorders except for one case of oedema in the LA1 group and one cutaneous nevus in the placebo group. All AE and biological abnormalities were considered unrelated to the study drug by the investigators. No treatment cessation was necessary because of AE.
Discussion
The probiotic strain L johnsonii LA1 was well tolerated in this study but failed to significantly reduce the six month risk of endoscopic recurrence after surgery for CD, at least to a clinically interesting level, as defined a priori in our protocol (the observed recurrence rate being 64% and 49% in the placebo and LA1 groups, respectively).
The rationale for probiotic use in CD is based on convincing evidence of a pathogenic role of intestinal bacteria.2,5L johnsonii LA1 was selected on the basis of its anti‐inflammatory effects in vitro10 and its ability to survive in the gastrointestinal tract.9 LA1 has also been shown to increase antibody responses to oral vaccination with Salmonella typhi Ty 21a12 and to stimulate the phagocytic activity of circulating granulocytes.9 LA1 does not increase intestinal permeability in healthy subjects.13
We chose the endoscopic recurrence rate as the primary endpoint for this study as use of the clinical recurrence rate requires larger numbers of patients and longer observation periods. The six month duration was also chosen in order to have sufficient statistical power. The endoscopic recurrence rate in the placebo group (64%) of our study was similar to that reported elsewhere1,3,4: endoscopic recurrence was observed in approximately 50% of patients three months after surgery and in 70% of patients after one year.1,3,4 New lesions usually appear on the anastomosis and proximally, and the presence of severe lesions is predictive of more rapid clinical relapse.1,4 The statistical power of our trial may not have been sufficient to rule out a slight benefit of LA1. Indeed, with 45 patients per group and a 60–70% six month endoscopic recurrence rate in the control group, the power to detect an actual 25% and 20% decrease in recurrence rate due to LA1 was approximately 67% and 48%, respectively, when using the χ2 test and a type I error of 5%. But the clinical value of drugs with only slight efficacy on postoperative CD recurrence is questionable.14 We started treatment as early as possible after surgery. As the inflammatory process leading to macroscopic recurrence begins early after surgery, one may question whether starting probiotics earlier, even before surgery, would be more effective (as a real preventive treatment). However, this was not observed in the small subset of patients who began LA1 before surgery in our trial (in this subgroup recurrence was observed in 6/10 patients in the placebo group compared with 6/9 in the LA1 group). It is noteworthy that similar results were obtained in the ITT and PP populations, showing that our negative results were not due to poor compliance or deviation from the protocol. Finally, we found no significant interaction between treatment efficacy and smoking status.
Five small randomised trials have tested probiotics for maintenance of remission in CD.7,8,15,16,17 Malchow tested Escherichia coliNissle 1917 in a double blind, placebo controlled study involving 28 patients who had initially been treated with prednisolone.15 At one year, the relapse rate was lower in the probiotic group than in the placebo group (30% v 64%) but the difference was not statistically significant.15 This pilot study has not been reproduced but three other studies showed that the same strain prevented ulcerative colitis relapse.16,18,19 Guslandi et al examined the effect of Saccharomyces boulardii in 32 patients who were randomised to receive either S boulardii 1 g/day plus mesalamine 2 g/day or mesalamine 3 g/day alone for six months.20 Clinical relapse occurred in 6% of patients in the probiotic group and in 37% of patients in the control group (p = 0.04), but this pilot study was not blinded and the results need to be confirmed. Prantera et al examined the preventive effect of L rhamnosus GG on postoperative endoscopic recurrence at one year in 45 patients.8 No other IBD medications were permitted in this double blind placebo controlled study. Endoscopic recurrence rates did not differ significantly between the two groups (60% and 35% in the L rhamnosus GG and placebo groups, respectively) and neither did the severe endoscopic recurrence rate (40% and 18%) or the clinical recurrence rate (17% v 11%). Another randomised controlled trial with the same strain confirmed that it was ineffective as an add‐on therapy to standard treatment to prevent relapse in 75 children with CD followed up for two years.17 Campieri et al carried out a single blind study to evaluate the postoperative preventive efficacy of a treatment combining rifaximin (a broad spectrum antibiotic) for three months followed by the probiotic mixture VSL#3 for nine months, in comparison with mesalazine 4 g/day for 12 months.7 Among the 40 patients enrolled in this study, the rate of severe endoscopic recurrence was lower in the antibiotic plus probiotic group (10% and 20% at three and 12 months, respectively) than in the mesalazine group (40% and 40%; p<0.01).
VSL#3 has been shown to prevent the occurrence and recurrence of pouchitis.21,22,23 The choice of a probiotic product for a clinical trial and the dose to be tested is difficult. Our choice of LA1 was based on its biological properties described above.9,10 This probiotic is present in commercial dairy product and we chose the dose usually present in these products in the hope to develop a nutritional strategy of prevention of recurrence of CD. No dose‐response study was available. Another research team has tested a higher dose of LA1 and did not observe a significant effect in preventing postoperative recurrence of CD.24 Probiotics differ strongly between each other and it is not possible to extrapolate a positive or negative result obtained with one strain to another strain. The ineffectiveness of L GG in the study of Prantera et al could not therefore predict the inefficacy of LA1 and cannot predict the inefficacy of other single strains in future trials.8 Extrapolation of doses between various strains or products is also not possible. Mixtures of various strains could theoretically have additional or synergistic effects but they may also have antagonistic properties.
LA1 was well tolerated in our study. Infections have been reported with other probiotic strains in other settings, especially in hospital patients with central catheters.25,26,27 Rare cases of infection by endogenous lactobacilli have also been reported in IBD patients,28 but no cases of probiotic related infection have been observed, despite the presence of intestinal ulcerations and poor intestinal barrier function. The effect of intercurrent immunomodulatory therapy on this risk is unknown, and should be considered when developing probiotics for IBD. Likewise, the possibility that some probiotics may stimulate the immune response in patients with IBD cannot be ruled out. In the study by Prantera et al, the postoperative recurrence rate tended to be higher in the LGG group than in the placebo group.8
We conclude that the LA1 probiotic at a daily dose of 4×109 cfu did not have a sufficiently beneficial effect, if any, on postoperative recurrence in patients with CD. As results obtained with one strain cannot be extrapolated to other strains or dosages, our negative results should not hinder the search for potential ecological treatments of CD. It remains to be determined whether combination therapy with probiotics plus antibiotics or synbiotics may be more effective than probiotic therapy alone.
Conflict of interest: declared (the declaration can be viewed on the Gut website at http://www.gutjnl.com/supplemental).
Supplementary Material
Acknowledgement
In addition to the authors, the following investigators participated in the study:
M Allez, P Cattan, JM Gornet, Hôpital Saint‐Louis, Paris; A Berger, HEGP, Paris; O Corcos, Y Panis, X Treton, Hôpital Lariboisière, Paris; JP Galmiche, Hôtel Dieu, Nantes; D Manaouil, Jean‐Marc Regimbeau, Hôpital Nord, Amiens; F Michot, G Savoye, Rouen; S Msika, Hôpital Louis Mourier, Colombes; L Picon, Hôpital Trousseau Tours; P Renard, Hôpital R Debré, Reims; F Zerbib, Hôpital Saint‐André, Bordeaux.
The authors are indebted to Patricia Détré for her technical help.
Abbreviations
CD - Crohn's disease
CDAI - CD activity index
CRP - C reactive protein
ITT - intent to treat
PP - per protocol
OR - odds ratio
AE - adverse events
Footnotes
This study was initiated, designed, and conducted by the GETAID Study Group. It was funded by grant support from the Nestlé Research Centre, Vevey, Switzerland. Study products were provided by Nestlé. All data analysis and manuscript writing were performed independently by the GETAID Study Group, with no involvement of Nestlé representatives.
Conflict of interest: declared (the declaration can be viewed on the Gut website at http://www.gutjnl.com/supplemental).
References
- 1.Rutgeerts P, Geboes K, Vantrappen G.et al Predictability of the postoperative course of Crohn's disease. Gastroenterology 199099956–963. [DOI] [PubMed] [Google Scholar]
- 2.Marteau P, Lepage P, Mangin I.et al Gut flora and inflammatory bowel disease. Aliment Pharmacol Ther 200420(suppl 4)18–23. [DOI] [PubMed] [Google Scholar]
- 3.Rutgeerts P, Hiele M, Geboes K.et al Controlled trial of metronidazole treatment for prevention of Crohn's recurrence after ileal resection. Gastroenterology 19951081617–1621. [DOI] [PubMed] [Google Scholar]
- 4.Rutgeerts P J, Van Assche G, Vermeire S.et al Ornidazole for prophylaxis of postoperative Crohn's disease recurrence of: a randomized double blind placebo controlled trial. Gastroenterology 2005128856–861. [DOI] [PubMed] [Google Scholar]
- 5.Sartor R B. Therapeutic manipulation of the enteric microflora in inflammatory bowel diseases: antibiotics, probiotics, and prebiotics. Gastroenterology 20041261620–1633. [DOI] [PubMed] [Google Scholar]
- 6.Marteau P, Seksik P, Lepage P.et al Cellular and physiological effects of probiotics and prebiotics. Mini‐rev Med Chem 20044889–896. [DOI] [PubMed] [Google Scholar]
- 7.Campieri M, Rizzello F, Venturi A.et al Combination of antibiotic and probiotic treatment is efficacious in prophylaxis of post‐operative recurrence of Crohn's disease: a randomized controlled study vs mesalamine. Gastroenterology 2000118G4179 [Google Scholar]
- 8.Prantera C, Scribano M L, Falasco G.et al Ineffectiveness of probiotics in preventing recurrence after curative resection for Crohn's disease: a randomised controlled trial with Lactobacillus GG. Gut 200251405–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schiffrin E J, Rochat F, Link‐Amster H.et al Immune‐modulation of human blood cells following the ingestion of lactic acid bacteria. J Dairy Sci 199578491–497. [DOI] [PubMed] [Google Scholar]
- 10.Haller D, Bode C, Hammes W P.et al Non‐pathogenic bacteria elicit a differential cytokine response by intestinal epithelial cell/leucocyte co‐cultures. Gut 20004779–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Best W R, Becktel J M, Singleton J W. Rederived values of the eight coefficients of the Crohn's disease activity index (CDAI). Gastroenterology 197977843–846. [PubMed] [Google Scholar]
- 12.Link‐Amster H, Rochat F, Saudan K Y.et al Modulation of a specific humoral immune response an changes in intestinal flora mediated through fermented milk intake. FEMS Immunol Med Microbiol 19941055–64. [DOI] [PubMed] [Google Scholar]
- 13.Marteau P, Vaerman J P, Dehenin J P.et al Effect of intrajejunal perfusion and chronic ingestion of Lactobacillus acidophilus strain La1 on serum concentrations and jejunal secretions of immunoglobulins and serum proteins in healthy humans. Gastroenterol Clin Biol 199721293–298. [PubMed] [Google Scholar]
- 14.Sandborn W J, Feagan B G. The efficacy of azathioprine and 6‐mercaptopurine for the prevention of postoperative recurrence in patients with Crohns disease remains uncertain. Gastroenterology 2004127990–993. [DOI] [PubMed] [Google Scholar]
- 15.Malchow H A. Crohn's disease and Escherichia coli. A new approach in therapy to maintain remission of colonic Crohn's disease? J Clin Gastroenterol 199725653–658. [DOI] [PubMed] [Google Scholar]
- 16.Kruis W, Schutz E, Fric P.et al Double‐blind comparison of an oral Escherichia coli preparation and mesalazine in maintaining remission of ulcerative colitis. Aliment Pharmacol Ther 199711853–858. [DOI] [PubMed] [Google Scholar]
- 17.Bousvaros A, Guandalini S, Baldassano R N.et al A randomized, double‐blind trial of Lactobacillus GG versus placebo in addition to standard maintenance therapy for children with Crohn's disease. Inflamm Bowel Dis 200511833–839. [DOI] [PubMed] [Google Scholar]
- 18.Rembacken B J, Snelling A M, Hawkey P M.et al Non‐pathogenic Escherichia coli versus mesalazine for the treatment of ulcerative colitis: a randomised trial. Lancet 1999354635–639. [DOI] [PubMed] [Google Scholar]
- 19.Kruis W, Fric P, Pokrotnieks J.et al Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as with standard mesalazine. Gut 2004531617–1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guslandi M, Mezzi G, Sorghi M.et al Saccharomyces boulardii in maintenance treatment of Crohn's disease. Dig Dis Sci 2000451462–1464. [DOI] [PubMed] [Google Scholar]
- 21.Gionchetti P, Rizzello F, Venturi A.et al Oral bacteriotherapy as maintenance treatment in patients with chronic pouchitis: a double‐blind, placebo‐controlled trial. Gastroenterology 2000119305–309. [DOI] [PubMed] [Google Scholar]
- 22.Mimura T, Rizzello F, Helwig U.et al Once daily high dose probiotic therapy (VSL#3) for maintaining remission in recurrent or refractory pouchitis. Gut 200453108–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gionchetti P, Rizzello F, Helwig U.et al Prophylaxis of pouchitis onset with probiotic therapy: a double‐blind, placebo‐controlled trial. Gastroenterology 20031241202–1209. [DOI] [PubMed] [Google Scholar]
- 24.Van Gossum A, Dewit O, Geboes K.et al A randomized placebo‐controlled clinical trial of probiotics (L. johnsonii La1) on early endoscopic recurrence of Crohn's disease (CD) after ileocaecal resection. Gastroenterology 2005128A17 [Google Scholar]
- 25.Borriello S P, Hammes W P, Holzapfel W.et al Safety of probiotics that contain lactobacilli or bifidobacteria. Clin Infect Dis 200336775–780. [DOI] [PubMed] [Google Scholar]
- 26.Hennequin C, Kauffmann‐Lacroix C, Jobert A.et al Possible role of catheters in Saccharomyces boulardii fungemia. Eur J Clin Microbiol Infect Dis 20001916–20. [DOI] [PubMed] [Google Scholar]
- 27.Land M H, Rouster‐Stevens K, Wood C R.et al Lactobacillus sepsis associated with probiotic therapy. Pediatrics 2005115178–181. [DOI] [PubMed] [Google Scholar]
- 28.Farina C, Arosio M, Mangia M.et al Lactobacillus casei subsp. rhamnosus sepsis in a patient with ulcerative colitis. J Clin Gastroenterol 200133251–252. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.