Abstract
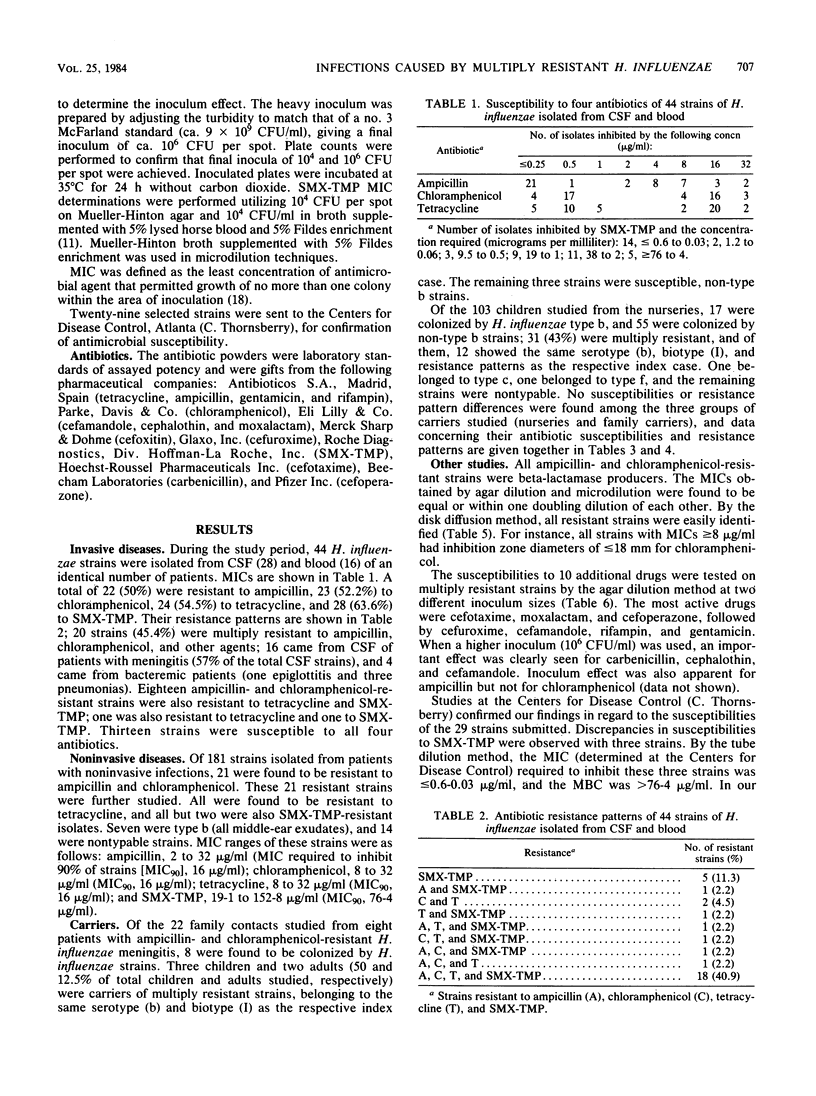
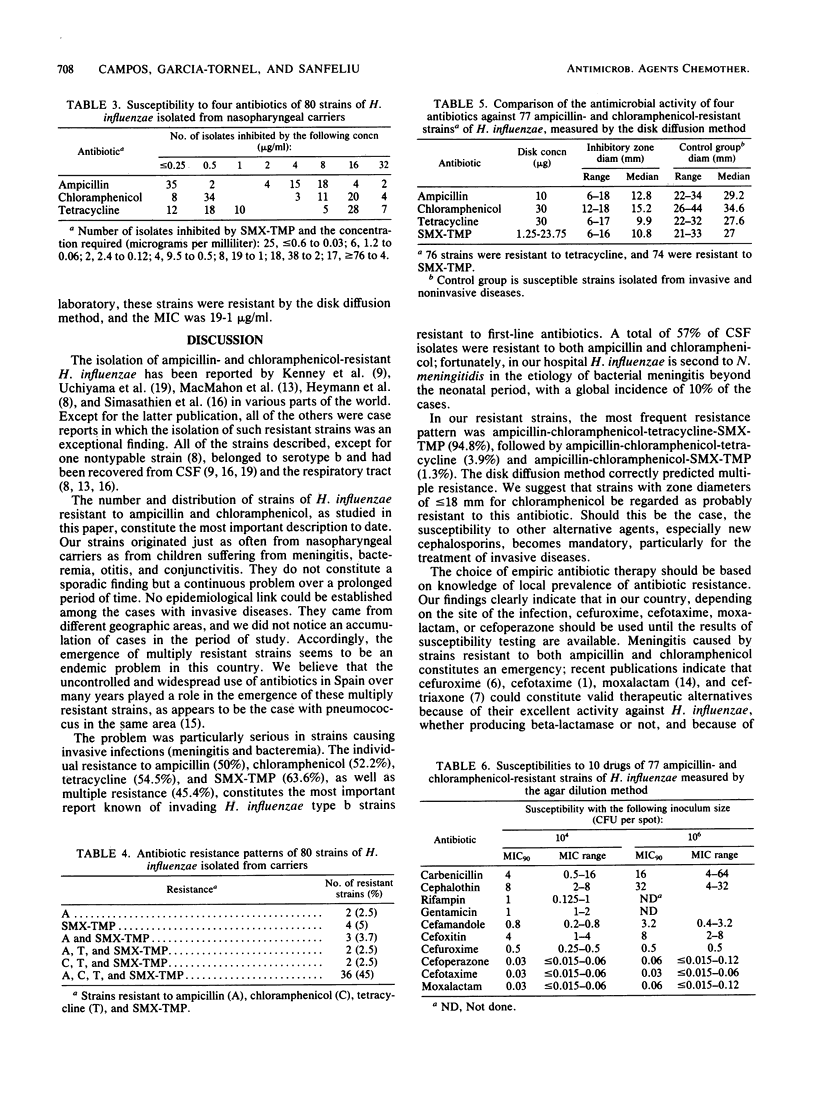
From February 1981 to December 1983, 225 strains were isolated from pediatric patients infected with Haemophilus influenzae. Forty-one strains were found to be resistant to ampicillin, chloramphenicol, and other antibiotics. They were isolated from 20 patients with invasive diseases (meningitis, 16; bacteremia, 4) and 21 with noninvasive diseases (otitis media, 19; conjunctivitis, 2). During this period, 44 patients with invasive diseases were seen (meningitis, 28; bacteremia, 16). Strains resistant to both ampicillin and chloramphenicol occurred in 45.4% of cerebrospinal fluid and blood isolates and in 51% of cerebrospinal fluid isolates only. In this group, individual resistance to ampicillin was 50%; chloramphenicol, 52.2%; tetracycline, 54.5%; and sulfamethoxazole-trimethoprim, 63.6%. No epidemiological relationship could be found among the patients. The presence of asymptomatic carriers was investigated in two nurseries and in eight family groups. From a total of 125 individuals studied, 80 were found to be colonized by H. influenzae, and 36 carried multiply resistant strains. From patients and carriers, 77 strains were found to be resistant to ampicillin, chloramphenicol, and other drugs; 39 belonged to type b (cerebrospinal fluid, 16; blood, 4; ear, 7; and nasopharynx, 12), and 38 were non-type b. The most frequent pattern of resistance was ampicillin-chloramphenicol-tetracycline-sulfamethoxazole-trimethoprim (94.8%), followed by ampicillin-chloramphenicol-tetracycline (3.9%). The disk diffusion method correctly predicted multiple resistance. The mean inhibition zone diameters were: ampicillin, 12.8 mm; chloramphenicol, 15.2 mm; tetracycline, 9.9 mm; and sulfamethoxazole-trimethoprim, 10.8 mm. These resistant strains were susceptible to cefotaxime, moxalactam, cefoperazone, cefuroxime, rifampin, and gentamicin. Our data suggest that in Spain the resistance of H. influenzae to ampicillin and chloramphenicol is endemic and that other effective therapeutic modalities are needed.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Belohradsky B. H., Bruch K., Geiss D., Kafetzis D., Marget W., Peters G. Intravenous cefotaxime in children with bacterial meningitis. Lancet. 1980 Jan 12;1(8159):61–63. doi: 10.1016/s0140-6736(80)90491-2. [DOI] [PubMed] [Google Scholar]
- Campos Marqués J., García-Tornel S., Galvi Tahull J. M. Invasive infections caused by multiply resistant Haemophilus influenzae type b. J Pediatr. 1984 Jan;104(1):162–163. doi: 10.1016/s0022-3476(84)80626-5. [DOI] [PubMed] [Google Scholar]
- Kenny J. F., Isburg C. D., Michaels R. H. Meningitis due to Haemophilus influenzae type b resistant to both ampicillin and chloramphenicol. Pediatrics. 1980 Jul;66(1):14–16. [PubMed] [Google Scholar]
- Kilian M. A taxonomic study of the genus Haemophilus, with the proposal of a new species. J Gen Microbiol. 1976 Mar;93(1):9–62. doi: 10.1099/00221287-93-1-9. [DOI] [PubMed] [Google Scholar]
- Kirven L. A., Thornsberry C. Minimum bactericidal concentration of sulfamethoxazole-trimethoprim for Haemophilus influenzae: correlation with prophylaxis. Antimicrob Agents Chemother. 1978 Nov;14(5):731–736. doi: 10.1128/aac.14.5.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liñares J., Garau J., Domínguez C., Pérez J. L. Antibiotic resistance and serotypes of Streptococcus pneumoniae from patients with community-acquired pneumococcal disease. Antimicrob Agents Chemother. 1983 Apr;23(4):545–547. doi: 10.1128/aac.23.4.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macmahon P., Sills J., Hall E., Fitzgerald T. Haemophilus influenza type b resistant to both chloramphenicol and ampicillin in Britain. Br Med J (Clin Res Ed) 1982 Apr 24;284(6324):1229–1229. doi: 10.1136/bmj.284.6324.1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modai J., Wolff M., Lebas J., Meulemans A., Manuel C. Moxalactam penetration into cerebrospinal fluid in patients with bacterial meningitis. Antimicrob Agents Chemother. 1982 Apr;21(4):551–553. doi: 10.1128/aac.21.4.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips I., Warren C., Waterworth P. M. Determination of antibiotic sensitivities by the Sensititre system. J Clin Pathol. 1978 Jun;31(6):531–535. doi: 10.1136/jcp.31.6.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simasathien S., Duangmani C., Echeverria P. Haemophilus influenzae type B resistant to ampicillin and chloramphenicol in an orphanage in Thailand. Lancet. 1980 Dec 6;2(8206):1214–1217. doi: 10.1016/s0140-6736(80)92478-2. [DOI] [PubMed] [Google Scholar]
- Uchiyama N., Greene G. R., Kitts D. B., Thrupp L. D. Meningitis due to Haemophilus influenzae type b resistant to ampicillin and chloramphenicol. J Pediatr. 1980 Sep;97(3):421–424. doi: 10.1016/s0022-3476(80)80193-4. [DOI] [PubMed] [Google Scholar]
- del Rio M. A., Chrane D., Shelton S., McCracken G. H., Jr, Nelson J. D. Ceftriaxone versus ampicillin and chloramphenicol for treatment of bacterial meningitis in children. Lancet. 1983 Jun 4;1(8336):1241–1244. doi: 10.1016/s0140-6736(83)92696-x. [DOI] [PubMed] [Google Scholar]
- del Rio M. de los A., Chrane D. F., Shelton S., McCracken G. H., Jr, Nelson J. D. Pharmacokinetics of cefuroxime in infants and children with bacterial meningitis. Antimicrob Agents Chemother. 1982 Dec;22(6):990–994. doi: 10.1128/aac.22.6.990. [DOI] [PMC free article] [PubMed] [Google Scholar]


