Tumour necrosis factor α (TNF‐α) plays a pivotal role in the pathogenesis of Crohn's disease. Infliximab, a chimeric monoclonal antibody against TNF‐α, has been shown to be highly effective in the treatment of Crohn's disease.1 However, treatment with infliximab may give rise to serious adverse events, including autoimmune disorders.2 We report a case of fatal aseptic meningitis associated with infliximab therapy.
A 53 year old Caucasian man was admitted to a regional hospital with progressive bloody diarrhoea. His medical history revealed a myocardial infarction in 1993. Endoscopy and histology established a diagnosis inflammatory bowel disease (IBD) but could not distinguish between ulcerative colitis and Crohn's disease. Because his symptoms did not improve following steroid and azathioprine treatment, infliximab therapy was initiated. Six days after the initial infliximab infusion, temporary numbness of the right arm and the right perioral area developed, followed four days later by dysarthria and left sided weakness and sensory loss. Cerebral computed tomography imaging revealed no abnormalities. All neurological symptoms resolved spontaneously within a few days.
Because of ongoing complaints consistent with luminal disease activity, a second dose of infliximab was administered two weeks after the initial dose. Complaints related to IBD gradually diminished with this regimen. After three days, however, neurological symptoms recurred. Over the course of three weeks he developed a dysarthria, left sided hemianopia, and motor aphasia. His level of consciousness decreased gradually and generalised seizures occurred. At that time, cerebrospinal fluid analysis showed a mild pleiocytosis and meningoencephalitis was suspected. He was treated with acyclovir, but analysis of blood and cerebrospinal fluid cultures as well as polymerase chain reaction (PCR) did not reveal any infectious agent.
Seven months after the onset of gastrointestinal symptoms and 3.5 months after the first dose of infliximab, the patient was referred to our hospital. He had a normal blood pressure and was afebrile. On neurological examination he had reduced consciousness (Glasgow coma scale E2M4V2), no meningism, intact light and corneal reflexes, and a right hemiparalysis. Magnetic resonance imaging of the brain revealed bilateral hyperintense cortical and subcortical lesions on T2 weighted imaging that showed enhancement with gadolinium. There were no signs of cerebral sinus thrombosis. Cerebral angiography showed focal narrowing of branches of the middle cerebral arteries, suggestive of vasculitis. Because repeated cultures and PCR of cerebral tissue (obtained on biopsy), blood, and cerebrospinal fluid remained negative (including for JC and BK virus) it was decided to start treatment with cyclophosphamide and prednisone for a suspected cerebral vasculitis. Despite this treatment, the patient's condition deteriorated gradually and he died approximately one month later. An autopsy was performed.
Histopathological examination revealed necrosis of the cerebral cortex (fig 1) and mononuclear infiltration with macrophages and giant cells. As no causative infectious agent or evidence for cerebral vasculitis was found, the diagnosis aseptic meningoencephalitis was made.
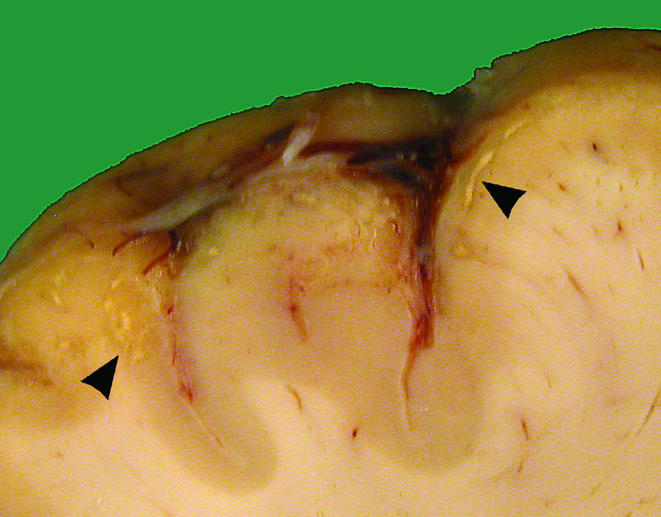
Figure 1 Cross section of the cerebral frontal cortex with multiple yellowish lesions (arrowheads) in the grey matter compatible with inflammatory infiltrate and tissue necrosis.
Neurological complications related to infliximab are uncommon.2 It has been suggested that treatment with infliximab may give rise to inflammatory demyelinating disease of the central nervous system.3,4 Aseptic meningitis related to infliximab, as in our patient, has been reported twice,5,6 but this is the first case of meningoencephalitis with a fatal outcome. In our patient, involvement of a broad range of infectious agents, including tuberculosis, was excluded.
The pathogenesis of infliximab related aseptic meningitis is unknown, and in the first case reported5 generation of antibodies to neurones or to infliximab was excluded. Presumably, the inability of infliximab to pass the blood‐brain barrier results in a failure to downregulate proinflammatory pathways in the brain while effectively blocking peripheral TNF‐α. Based on the present case and the currently available literature, we conclude that infliximab therapy should be withdrawn permanently when (even transient) neurological symptoms occur.
Acknowledgements
We thank RHWM Derksen, MD PhD, Department of Rheumatology and Immunology, UMC Utrecht, for critically reviewing our manuscript.
Footnotes
Conflict of interest: None declared.
References
- 1.Hanauer S B, Feagan B G, Lichtenstein G R.et al Maintenance infliximab for Crohn's disease: the ACCENT I randomized trial. Lancet 20023591541–1549. [DOI] [PubMed] [Google Scholar]
- 2.Colombel J F, Loftus E V, Jr, Tremaine W J.et al The safety profile of infliximab in patients with Crohn's disease: The Mayo Clinic experience in 500 patients. Gastroenterology 200412619–31. [DOI] [PubMed] [Google Scholar]
- 3.Thomas C W, Jr, Weinshenker B G, Sandborn W J. Demyelinisation during anti TNF‐α therapy with infliximab for Crohn's disease. Inflamm Bowel Dis 20041028–31. [DOI] [PubMed] [Google Scholar]
- 4.Mohan N, Edwards E T, Cupps T R.et al Demyelination occurring during anti‐tumor necrosis factor alpha therapy for inflammatory arthritides. Arthritis Rheum 2001442862–2869. [DOI] [PubMed] [Google Scholar]
- 5.Marotte H, Charrin J E, Miossec P. Infliximab‐induced aseptic meningitis. Lancet 20013581784. [DOI] [PubMed] [Google Scholar]
- 6.Hegde N, Gayomali C, Rich M W. Infliximab‐induced headache and infliximab induced meningitis: two ends of the same spectrum? South Med J 200598564–566. [DOI] [PubMed] [Google Scholar]


