Abstract
The yeast Candida albicans is a harmless commensal in most healthy people, but it causes superficial as well as life-threatening systemic infections in immunocompromised patients. C. albicans can colonize or infect virtually all body sites because of its high adaptability to different host niches, which involves the activation of appropriate sets of genes in response to complex environmental signals. We have used an in vivo expression technology that is based on genetic recombination as a reporter of gene expression to monitor the differential activation of individual members of a gene family encoding secreted aspartic proteinases (Saps), which have been implicated in C. albicans virulence, at various stages of the infection process. Our results demonstrate that SAP expression depends on the type of infection, with different SAP isogenes being activated during systemic disease as compared with mucosal infection. In addition, the activation of individual SAP genes depends on the progress of the infection, some members of the gene family being induced immediately after contact with the host, whereas others are expressed only after dissemination into deep organs. In the latter case, the number of invading organisms determines whether induction of a virulence gene is necessary for successful infection. The in vivo expression technology allows the elucidation of gene expression patterns at different stages of the fungus–host interaction, thereby revealing regulatory adaptation mechanisms that make C. albicans the most successful fungal pathogen of humans and, at the same time, identifying the stage of an infection at which certain virulence genes may play a role.
The yeast Candida albicans is a member of the microflora in most healthy people, where it predominantly colonizes the mucosal surfaces of the gastrointestinal tract. However, especially in immunocompromised patients, C. albicans develops from a harmless commensal to an opportunistic pathogen that can cause superficial as well as life-threatening disseminated infections (1). Although the immune status of the host is the major factor that determines whether C. albicans can become a pathogen and cause infection, the fact that C. albicans is by far the most frequent cause of fungal infections in such debilitated patients indicates that it must possess traits that make it a more successful colonizer and pathogen than other medically important Candida species or the usually apathogenic yeast Saccharomyces cerevisiae. It is a general view that the pathogenicity of C. albicans is not caused by single dominant virulence factors (2). Rather, it seems to be the high adaptability of C. albicans to many different host niches, as illustrated by the possession of many different adhesins that mediate binding to a variety of tissues, which allows the fungus the colonization and infection of virtually all body locations (3–6). A prerequisite for this adaptability is the capacity to respond to complex environmental signals representing the different host niches by the expression of an appropriate set of virulence-related and other genes.
C. albicans possesses a gene family encoding secreted aspartic proteinases (7, 8), and these enzymes have been linked with the virulence of the fungus since their discovery (9–11). Proposed functions of the proteinases during infection include the digestion of host proteins for nutrient supply, the evasion of host defenses by degrading immunoglobulins and complement proteins, adherence, and degradation of host barriers during invasion (12). Individual members of the gene family might have their own special role in infection, and this might be reflected by a differential expression pattern at various stages of the infection process. In concordance with this assumption is the finding that the secreted aspartic proteinase (SAP) genes, which are not expressed in standard laboratory media, are differentially expressed in vitro under special induction conditions (13–16). However, although proteinase production has been observed during experimental infection (17), the in vivo regulation and role in pathogenicity of the individual SAP genes remains unclear.
For bacterial pathogens, different in vivo expression technologies (IVETs) have been developed to detect expression of a gene during infection (18). One of these technologies, which uses site-specific recombination as a reporter of gene activation, is especially suitable to detect the in vivo induction of genes that are only transiently expressed at a certain stage of infection (19). In C. albicans, the development of similar reporter techniques has been hampered by the unusual codon usage of this organism (20), which is responsible for the failure to express most heterologous genes (21–23). We recently adapted the recombination-based IVET described by Camilli et al. (19) for use in C. albicans. The FLP gene encoding a site-specific recombinase from S. cerevisiae was genetically modified for expression in C. albicans, and FLP-mediated excision of a marker that confers resistance against mycophenolic acid (MPA) served to monitor the induction of a promoter by using FLP as a reporter gene (24). In this report, we describe the use of an optimized version of this IVET with enhanced sensitivity to analyze the expression of six different members of the C. albicans SAP gene family during superficial and disseminated infection in mice.
Materials and Methods
Strains and Growth Conditions.
C. albicans strains used in this study are listed in Table 1. Strains were maintained on minimal agar plates containing 6.7 g yeast nitrogen base without amino acids (Bio 101), 2 g glucose, and 0.77 g of complete supplement medium without uracil (CSM-URA; Bio 101) per liter. To screen for MPA-resistant and sensitive clones, 1 μg/ml of MPA was added to minimal agar plates. Other media used were YPD (20 g peptone, 10 g yeast extract, 20 g glucose) and YCB-BSA (23.4 g yeast carbon base, 4 g BSA, pH 4.0). Strains were routinely grown at 30°C. To support growth of strain CFI1, 100 μg/ml uridine was added to the media.
Table 1.
C. albicans strains used in this study
| Strain | Description | Reference |
|---|---|---|
| CFI1 | Δura3∷imm434/Δura3∷imm434, ACT1/act1∷FRT-MPAR-FRT | 24 |
| S2FI1 | as CFI1, but SAP2-2/sap2-1∷SAP2P-caFLP-URA3 | 24 |
| S1FI2A | as CFI1, but SAP1-1/sap1-2∷SAP1P-ecaFLP-URA3 | This study |
| S1FI2B | as CFI1, but SAP1-2/sap1-1∷SAP1P-ecaFLP-URA3 | This study |
| S2FI5B | as CFI1, but SAP2-2/sap2-1∷SAP2P-ecaFLP-URA3 | This study |
| S2FI5G | as CFI1, but SAP2-1/sap2-2∷SAP2P-ecaFLP-URA3 | This study |
| S3FI2B | as CFI1, but SAP3/sap3∷SAP3P-ecaFLP-URA3 | This study |
| S3FI2C | as CFI1, but SAP3/sap3∷SAP3P-ecaFLP-URA3 | This study |
| S4FI2A | as CFI1, but SAP4-1/sap4-2∷SAP4P-ecaFLP-URA3 | This study |
| S4FI2B | as CFI1, but SAP4-2/sap4-1∷SAP4P-ecaFLP-URA3 | This study |
| S5FI2A | as CFI1, but SAP5-2/sap5-1∷SAP5P-ecaFLP-URA3 | This study |
| S5FI2B | as CFI1, but SAP5-1/sap5-2∷SAP5P-ecaFLP-URA3 | This study |
| S6FI2A | as CFI1, but SAP6/sap6∷SAP6P-ecaFLP-URA3 | This study |
| S6FI2B | as CFI1, but SAP6/sap6∷SAP6P-ecaFLP-URA3 | This study |
Site-Specific Mutagenesis.
The four amino acid exchanges, P2S, L33S, Y108N, and S294P, (25) were introduced into the C. albicans-adapted FLP gene (caFLP) in several successive steps by using a PCR-based mutagenesis procedure. A fragment comprising positions 1–109 of the caFLP coding sequence was amplified from plasmid pFLP6123 (24) with the primers FLP12 (5′-CAGCAGCACATGATGCTATTTTC-3′) and FLP14 (5′-TCGAGGTCGACAAAATGTCACAATTTGATATATTATGTA-3′), thereby introducing the P2S and L33S exchanges (nucleotide substitutions are underlined) and a translation consensus sequence (AAA, ref. 26) between the SalI site and the FLP start codon (shown in bold). The PCR product was phosphorylated and digested with SalI. A second fragment comprising caFLP sequences from position 110 to the EcoRI site at position 750 was amplified from pFLP6123 with primer FLP13 (5′-AACTAACCTATTTATGTTGG-3′) and the universal primer. After digestion of the phosphorylated PCR product at a vector-derived SacI site, the two caFLP fragments were fused at their blunt ends and ligated between the SalI and SacI sites of pBluescript. The generated plasmid, pFLPT12, served as template for the introduction of the Y108N mutation by amplification of a caFLP fragment with the primers FLP14 and FLP15 (5′-ATCAGATTGATGTTTTTGTCCATTGTAAGGAATAATTG-3′), which subsequently was used to replace the corresponding original fragment in the SalI/EcoRV-digested pFLPT12, creating pFLPT123. The S294P mutation was first introduced into the wild-type FLP gene in pFLP1 (24) by amplification of FLP coding sequences downstream of the HindIII site (bold letters) with primer FLP16 (5′-CAATAAAGCTTTGAAGAAAAATGCTCCTTATCCAATCTTTGC-3′) and the universal primer and substituting the HindIII/XbaI-digested PCR product for the corresponding original fragment in pFLP1, thereby generating pFLPT4. Finally, the four amino acid exchanges were combined by cloning the SalI–ClaI fragment from pFLPT123 into the SalI/ClaI-digested pFLPT4. The resulting plasmid pFLPT1234 contains the previously described three CTG-TTG codon exchanges in the caFLP gene (24) as well as the four amino acid substitutions that confer enhanced activity on the FLP recombinase (25).
Construction of C. albicans Reporter Strains with SAP-ecaFLP Fusions.
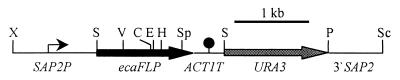
To facilitate subsequent cloning steps, part of the polylinker in plasmid pSFL26, which contains caFLP under the control of the SAP2 promoter (SAP2P) (24), was deleted by digestion with XhoI/BamHI, filling in the recessive ends and religation, yielding pSFL27. The SAP2 promoter from the SAP2P-FLP fusion in the reporter strain S2FI1 (24) was amplified with the primers SAP22 (5′-ACTTTCACTTCTAGATTTTTGCAAGC-3′) and FLP9 (5′-CGAACAAGCACCTTAGGTGG-3′). The PCR product was digested with XbaI/SalI and ligated together with a SalI–ClaI fragment from pFLPT123 into the XbaI/ClaI-digested pSFL27, generating pSFL212, which contains the P2S, L33S, and Y108N exchanges in the caFLP gene. The S294P mutation then was introduced by substitution of the ClaI–SpeI fragment from pFLPT4 for the corresponding fragment in pSFL212, generating pSFL213, which carries a SAP2P-ecaFLP fusion (Fig. 1).
Figure 1.
Structure of the insert in plasmid pSFL213 carrying the SAP2P-ecaFLP fusion. Relevant restriction sites used for cloning are shown. C, ClaI; E, EcoRI; H, HindIII; P, PstI; S, SalI; Sc, SacI; Sp, SpeI; V, EcoRV; X, XbaI. For the construction of analogous fusions with other SAP genes, the corresponding fragments were substituted for the flanking SAP2P and 3′SAP2 regions (see Materials and Methods).
Parts of the coding regions of the SAP1, SAP3, SAP4, SAP5, and SAP6 genes were obtained by PCR with the following primer pairs derived from the published sequences (X56867, L22358, L25388, Z30191, Z30192): SAP1C (5′-GTTATGCTGCAGACATCACTATTGG-3′) and SAP1D (5′-GACCGTTAGCGGAGCTCAACGGAGC-3′), SAP3C (5′-TGATTCTGCAGTTTCATGTCAAGCTGG-3′) and SAP3D (5′-TATAGGCTGAGCTCAAGAAATTATCACC-3′), SAP4C (5′-CGGTTCCTATTCTGCAGCTGCTTCTAGC-3′) and SAP4D (5′-GAGCCATGGAGCTCTTTCTATCATCC-3′), SAP5C (5′-ACCTGCTGCAGTTACTTTGCACAATGAAGC-3′) and SAP5D (5′-GGAACGGAGCTCTTGAGGTTATTACCA-3′), SAP6C (5′-CCCGTCGATGATACTGCAGAAATGTAGG-3′) and SAP6D (5′-AAGCAGGAACGGAGCTCTTGAGGTTTT-3′). The PCR products were digested at the introduced PstI and SacI sites (bold letters; nucleotide substitutions are underlined) and used to replace the 3′SAP2 fragment in pSFL27, yielding pSFL11, pSFL31, pSFL41, pSFL51, and pSFL61.
The SAP promoter regions immediately upstream of the start codons were obtained by PCR amplification from strain CFI1. For SAP1P, the primers SAP1P1 (5′-GGTTACGGAAAATCTAGAAGATGGCCC-3′) and SAP1P2 (5′-TGTGTGTCGACTTAGAAATGGAAGAGTGA-3′), derived from the published sequence (L12451) were used. The sequences of the SAP4, SAP5, and SAP6 promoter regions were kindly provided by Klaus Schröppel (Institut für Klinische Mikrobiologie und Immunologie, Erlangen, Germany) and amplified with the primer pairs SAP4P1 (5′-CGGGAAGGCTCTAGAATGTATACCC-3′) and SAP4P2 (5′-AACATGTCGACTTGAGTTGAACTTTGGATTAG-3′), SAP5P3 (5′-GTATAAATGCTCTAGAATTCTGTTTGGCG-3′) and SAP5P2 (5′-ACATTGTCGACTTGAGCTTAACTTTGGATTAG-3′), and SAP6P1 (5′-TCTCGGGAGGCTCTAGAATGTATCA-3′) and SAP6P2 (5′-ACATTGTCGACTTGAGCTTAACTTTAGATTAG-3′). To obtain the SAP3 promoter, a clone carrying the SAP3 gene was first identified by screening a C. albicans fosmid library (kindly provided by Stewart Scherer, Acacia Biosciences, Richmond, CA) with a probe from the SAP3 coding region. A suitable subfragment of a positive clone (1H10) was cloned, and partial sequence analysis revealed that SAP3 was located 1.1 kb downstream of the CDR1 gene. The primers SAP3P1 (5′-CATTGTTATCTAGACGTGGTGG-3′), derived from the CDR1 downstream sequence (X77589), and SAP3P2 (5′-AACATGTCGACTATATATGTGTATGTGTGTGTGG-3′) were used to amplify the SAP3 promoter region. All SAP promoter fragments were cut at the introduced XbaI and SalI sites (bold letters; nucleotide substitutions are underlined) and used to replace the SAP2 promoter in pSFL11, pSFL31, pSFL41, pSFL51, and pSFL61, generating pSFL12, pSFL32, pSFL42, pSFL52, and pSFL62, respectively. The SalI–SpeI fragment with caFLP sequences then was replaced in these plasmids by the corresponding ecaFLP fragment from pFLPT1234, resulting in pSFL13, pSFL33, pSFL43, pSFL53, and pSFL63. The inserts from these plasmids and pSFL213 were obtained by XbaI/SacI digestion, gel-purified, and used to replace one of the SAP alleles in the ura-negative strain CFI1 by the corresponding SAP-ecaFLP fusion after electroporation (27) and selection of transformants on minimal agar plates without uridine.
Isolation of Chromosomal DNA and Southern Hybridization.
Chromosomal DNA from C. albicans strains was isolated as described (28). Southern hybridization with enhanced chemiluminescence-labeled probes was performed with the ECL labeling and detection kit provided by Amersham Pharmacia, according to the instructions of the manufacturer.
In Vivo Experiments.
Eight- to twelve-week-old female BALB/c mice, which were used for i.v. and i.p. infection, or DBA/2 mice, which were used for oral infection, were purchased from Harlan (Borchen, Germany). To prepare the inoculum, C. albicans cells grown overnight in YPD broth at 37°C were washed twice in PBS (GIBCO) and resuspended in the same buffer. In all experiments, the inocula also were spread on MPA indicator plates to verify that no FLP induction had occurred before infection.
Infection of the oesophageal mucosa was produced after pretreating the animals 7 days and 24 h before infection with cyclophosphamide injected i.p. in a dosage of 150 mg/kg and 100 mg/kg, respectively. In addition, 24 h before infection, mice were treated orally with amoxycillin (10 mg per animal), gentamicin (8 mg per animal), and clindamycin (10 mg per animal). For oral infection, 1 × 108 blastoconidia were given by gavage. Three days after infection, mice were killed by cervical dislocation, and the oesophagus was removed aseptically and homogenized with Tenbroeck tissue grinders (Wheaton Scientific) in 5 ml of sterile distilled water supplemented with 5 μg/ml gentamicin. Aliquots of the homogenates were plated on indicator plates containing 1 μg/ml MPA and incubated at 30°C for 2 days to determine the percentage of MPA-sensitive cells, which gave rise to uniformly smaller colonies as compared with cells that contained the MPAR marker and produced large colonies. Because there is sometimes a low background of cells that accidentally grow as smaller colonies of varying size (<2%; ref. 24), the MPA-sensitive phenotype was confirmed by restreaking on plates containing 10 μg/ml MPA in cases where the percentage of small colonies was only slightly higher than the unspecific background.
For induction of peritonitis, mice were infected i.p. with 5 × 107 blastoconidia in 0.5 ml of PBS. Thirty minutes postinfection, C. albicans cells were recovered by peritoneal lavage with 10 ml of PBS. Cells that adhered to the liver surface at 4 h but had not yet invaded (as confirmed by microscopic examination) were recovered by first washing the peritoneal cavity to remove nonadherent cells. The organ then was cut out, homogenized in 10 ml of sterile distilled water, and plated. At 48 h postinfection, mesenteric lymph nodes and the infiltrated organs liver, pancreas, and spleen were cut out as a whole, homogenized, and plated as described above. The kidneys were removed separately and treated in the same way.
For i.v. infection, mice received either 2 × 105 or 4 × 105 blastoconidia in 0.2 ml of PBS by means of the lateral tail vein. Four days after infection, the mice were killed by cervical dislocation. The kidneys were removed aseptically and homogenized, and the percentage of MPAS C. albicans cells was determined as described above.
Results
A C. albicans IVET with Enhanced Sensitivity.
With an IVET that is based on genetic recombination as a reporter of gene expression, the activation of a gene can be detected in single cells whenever there is a sufficient concentration of the recombinase enzyme in a cell to result in excision of the marker, i.e., when the activity of the promoter is above a threshold level. Using a reporter strain that carried a C. albicans-adapted FLP gene (here referred to as caFLP) under control of the SAP2 promoter, we previously could detect activation of the SAP2 gene by monitoring FLP-mediated excision of an MPAR marker, which rendered the cells MPA sensitive (24). After growth in SAP2-inducing medium, the majority (70–80%), but not all cells had lost the marker, indicating that, in some cells, the SAP2 gene was not sufficiently activated to result in detectable FLP activity. Differences in SAP2 expression within a population had previously also been detected by using GFP as a reporter gene (23); however, in this case virtually all cells fluoresced, although with different intensities. These observations suggested that the FLP-based IVET was not sensitive enough to detect low-level activation of a gene.
Recently, a mutated FLP recombinase, eFLP, has been described that carries four amino acid exchanges, P2S, L33S, Y108N, and S294P, which confer enhanced activity on the enzyme (25). To increase the sensitivity of our IVET for C. albicans, we introduced these four amino acid substitutions into caFLP. A reporter strain then was constructed that carried the ecaFLP gene under control of the SAP2 promoter. The resulting strain S2FI5B differed from the previously described strain S2FI1 (24) only by the presence of ecaFLP instead of caFLP and carried the reporter fusion in the same SAP2 allele (see also below).
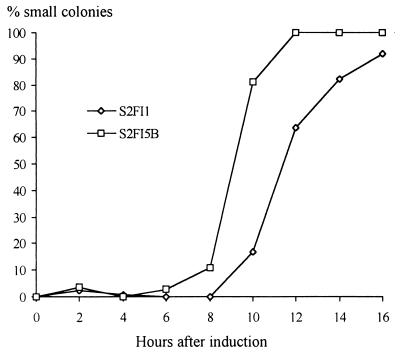
FLP activity in strains S2FI1 and S2FI5B was monitored after a shift from SAP2-repressing medium into SAP2-inducing medium in which SAP2 mRNA appears after 6–8 h of growth (24). As can be seen in Fig. 2, ecaFLP proved to be a more sensitive reporter of gene activation than caFLP, because FLP activity in strain S2FI5B was detected earlier than in strain S2FI1. In addition, SAP2 activation was detected in all cells of strain S2FI5B because, after 12 h, the whole population had become MPA sensitive. In contrast, only 90% of the cells of strain S2FI1 had become MPA sensitive after 16 h, and this percentage was not further elevated even after 28 h (data not shown). Therefore, SAP2 activation in C. albicans cells in which the gene was induced only at low levels could be detected with ecaFLP but not with caFLP as a reporter gene.
Figure 2.
FLP activity in C. albicans strains S2FI1 and S2FI5B carrying chromosomally integrated caFLP and ecaFLP genes, respectively, under control of the SAP2 promoter. Cells were grown overnight in SAP2-repressing minimal medium and inoculated into SAP2-inducing medium YCB-BSA. FLP-mediated excision of the MPAR marker was analyzed by determining the percentage of MPAS cells at the indicated times.
Construction of a Set of C. albicans Reporter Strains.
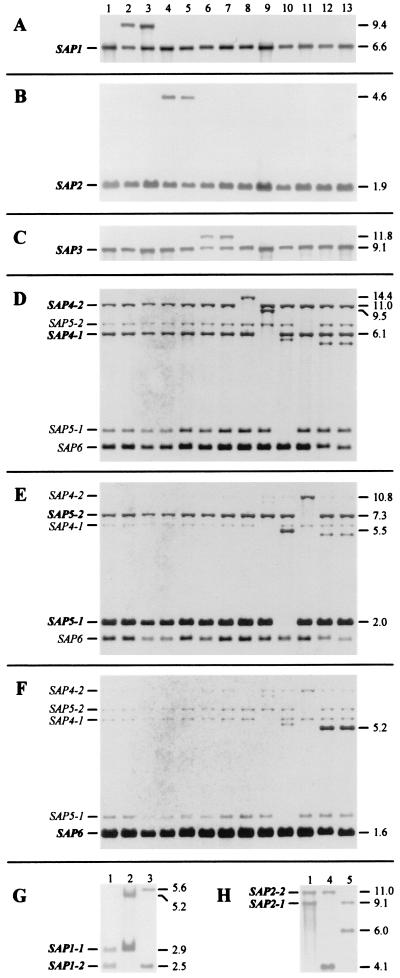
To analyze the expression of individual members of the SAP gene family during infection, ecaFLP was fused to the promoters of the SAP1-SAP6 genes and integrated into one of the corresponding SAP alleles of strain CFI1 that carries the deletable MPAR marker. Southern hybridization analysis of the transformants confirmed that the fusions had been correctly integrated and that the other SAP genes remained unchanged in each case (Fig. 3). The two SAP4 and the two SAP5 alleles could be distinguished by a BglII restriction site polymorphism, and the SAP1 and SAP2 alleles by KpnI and ClaI restriction site polymorphisms, respectively. In these cases, the two alleles were arbitrarily assigned a suffix (e.g., SAP1-1 and SAP1-2), and two transformants carrying the reporter gene fusion in either of the two possible SAP alleles were selected. For SAP3 and SAP6, no restriction site polymorphisms were found, and two randomly selected transformants were kept in each case. None of the strains had lost the MPAR marker during selection on minimal plates and subsequent growth in YPD medium, demonstrating that, despite the enhanced sensitivity of the reporter system, all strains were stable during growth in standard laboratory media in which expression of SAP genes is repressed.
Figure 3.
Construction of C. albicans reporter strains carrying chromosomally integrated fusions of the promoter regions of SAP1-SAP6 with ecaFLP. (A–F) Southern hybridizations of BglII-digested genomic DNA with the promoter fragments of the SAP1–SAP6 genes as probes. To distinguish between integration into either of the two SAP1 and the two SAP2 alleles, KpnI (G) and ClaI (H), digested DNA of the corresponding strains was used additionally. The fragments representing the wild-type SAP alleles are indicated in bold letters on the left side of the blots; the crosshybridizing SAP4, SAP5, and SAP6 alleles also are indicated. The sizes of the wild-type fragments and those containing the reporter fusions are shown on the right side of the blots. Lanes: 1, CFI1 (parent strain); 2, S1FI2A (sap1-2∷SAP1P-ecaFLP); 3, S1FI2B (sap1-1∷SAP1P-ecaFLP); 4, S2FI5B (sap2-1∷SAP2P-ecaFLP); 5, S2FI5G (sap2-2∷SAP2P-ecaFLP); 6, S3FI2B (sap3∷SAP3P-ecaFLP); 7, S3FI2C (sap3∷SAP3P-ecaFLP); 8, S4FI2A (sap4-2∷SAP4P-ecaFLP); 9, S4FI2B (sap4-1∷SAP4P-ecaFLP); 10, S5FI2A (sap5-1∷SAP5P-ecaFLP); 11, S5FI2B (sap5-2∷SAP5P-ecaFLP); 12, S6FI2A (sap6∷SAP6P-ecaFLP); 13, S6FI2B (sap6∷SAP6P-ecaFLP).
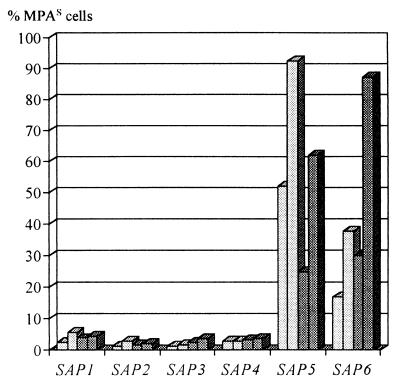
Differential Expression of SAP Genes During Infection of the Oesophageal Mucosa.
The 12 reporter strains were used in a mouse model of oesophageal infection in which C. albicans invades into the epithelium but does not disseminate through the bloodstream. After 3 days of infection, heavy mycelial growth of the strains and mucosal invasion was observed. The fungal cells were recovered from the infected tissue, and the percentage of MPA-sensitive cells was determined. Fig. 4 shows that the SAP5 and SAP6 genes were strongly activated during infection of the oesophageal mucosa, whereas only low-level induction of SAP1–SAP4 had occurred.
Figure 4.
Expression of individual SAP genes during oesophageal infection. For each of the reporter strains, two mice were orally infected, and C. albicans cells that had invaded the oesophageal epithelium were reisolated from homogenized tissue after 3 days of infection. Activation of the SAP genes in the reporter strains was analyzed by determining the percentage of MPAS cells. The light gray columns show SAP induction in strains S1FI2A, S2FI5B, S3FI2B, S4FI2A, S5FI2A, and S6FI2A, and the dark gray columns show the results obtained with S1FI2B, S2FI5G, S3FI2C, S4FI2B, S5FI2B, and S6FI2B.
Stage-Specific Activation of SAP Genes During Intraperitoneal Infection.
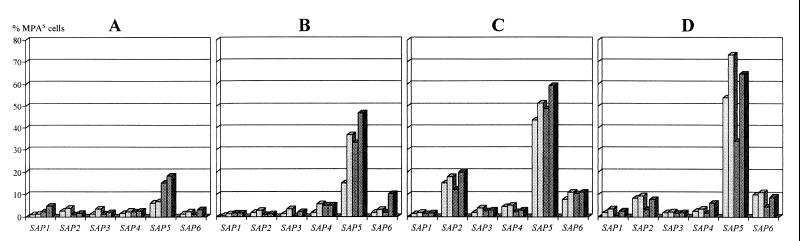
To monitor expression of the various SAP genes during systemic disease, a mouse model of Candida peritonitis was used, and the reporter strains were reisolated at various stages and from different sites of the infection. The SAP5 gene was significantly activated already 30 min after inoculation in the peritoneal cavity, whereas the other SAP genes were induced in only a few cells (Fig. 5A). Remarkably, only yeast cells but no germ tubes or hyphae were detected at this early stage of the infection. After 4 h, C. albicans cells that adhered to the liver surface exhibited mycelial growth, and a large portion of the population had activated SAP5 but not, or only at low levels, the other SAP genes (Fig. 5B). After 48 h, when the cells had invaded into the liver, a significant activation of SAP6 and, as previously reported, SAP2 had occurred in addition to SAP5 (Fig. 5C). At this time point, the C. albicans cells also had disseminated by the bloodstream into the kidneys, and a SAP expression pattern similar to that seen after liver invasion was observed (Fig. 5D).
Figure 5.
Stage-specific induction of individual SAP genes during the course of i.p. infection. For each of the reporter strains, two mice were infected i.p., and SAP activation was determined in cells recovered by peritoneal lavage 30 min after inoculation (A), in cells adhering to the tissue after 4 h of infection (B), and in cells that had invaded the liver (C) or disseminated to the kidneys (D) after 48 h of infection. Strains are as described in the legend to Fig. 4.
SAP Expression after Hematogenous Dissemination.
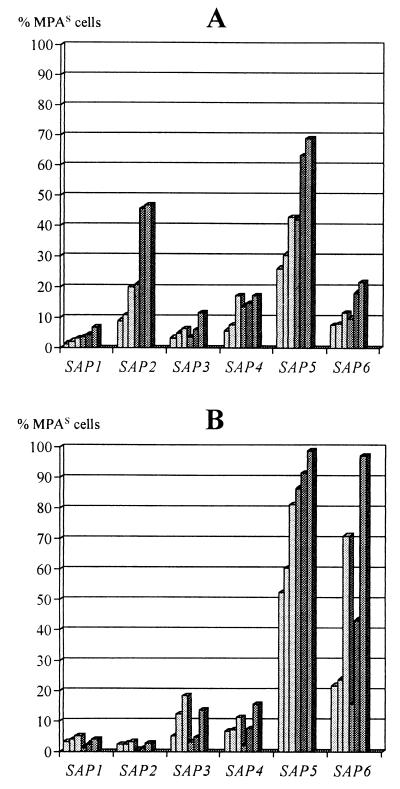
Because loss of the MPAR marker is an irreversible event, down-regulation of a gene after a previous induction cannot be detected with the IVET used. To determine whether some SAP genes are induced only during the early stages of a systemic infection but are not expressed after C. albicans has gained access to the bloodstream, an additional model of disseminated candidiasis in which the mice are infected by the i.v. route was used. In this model, a different outcome of the infection is seen within a narrow range of the infectious dose (24). With an inoculum of 4 × 105 cells, a strong multiplication of C. albicans occurred after hematogenous dissemination, resulting in 106 to 107 colony-forming units that could be recovered from the kidneys. The expression of SAP5, the first SAP gene induced after i.p. infection, was maintained after C. albicans had reached the bloodstream, because the gene also was activated after i.v. infection (Fig. 6A). In addition, SAP4 and SAP6 were significantly induced after dissemination to the kidneys, although at lower levels. The induction of SAP2 at this late stage of the infection, which had been reported previously (24), could be confirmed in these experiments. Expression of SAP1 and SAP3 was more variable, because it was clearly detected in some animals but occurred only at very low levels in others. Most strikingly, the activation of some SAP genes was extremely dependent on the outcome of the infection. With a slightly lower inoculum dose (2 × 105 cells), the organ load in the kidneys was decreased by about 2 orders of magnitude as compared with the higher inoculum. In this case, SAP2 expression was barely detectable, but other SAP genes were activated more strongly than with the higher infection dose that resulted in an overwhelming infection. Especially SAP5 and SAP6 had been induced in almost the whole population of infecting cells in some animals (Fig. 6B).
Figure 6.
Differential activation of SAP genes after hematogeneous dissemination. For each of the reporter strains, three mice were i.v.-infected with 4 × 105 cells (A) and three mice with 2 × 105 cells (B). SAP activation was determined in cells recovered from the kidneys after 4 days of infection. Strains are as described in the legend to Fig. 4.
Discussion
The results of this study demonstrate that the recombination-based IVET for C. albicans is highly useful to analyze gene expression patterns at various stages of the fungus–host interaction. We have shown that C. albicans adapts to different host niches by the activation of appropriate subsets of SAP genes, according to the needs of the fungus in the course of an infection. It previously has been suggested that environmental parameters, like the pH of the host niche, determine which SAP gene is expressed, and that SAP4, SAP5, and SAP6 are hyphae-specific genes (13, 14). Our results suggest that this is probably too simplistic a view and that the host signals governing the activation of specific SAP genes are more complex. SAP5 and SAP6, but not the other SAP genes, were strongly activated during invasion of the oesophageal mucosa by C. albicans hyphae. SAP5, but not SAP6, also was induced immediately after inoculation in the peritoneal cavity, a host niche that is different from the oesophageal mucosa. Most strikingly, SAP5 expression at this stage of the infection did not correlate with the presence of germ tubes or hyphae because only blastoconidia were observed in the peritoneal lavage. Therefore, the expression of SAP5 may be induced by host signals that also result in hyphae formation, and both SAP5 expression and mycelial growth then could contribute to tissue invasion. In contrast, SAP6 activation was detected only when C. albicans hyphae also were observed in the infected tissue, and SAP6 may indeed be a hyphae-specific gene.
The SAP2 gene was significantly activated only in the late stages of infection, after spread to deep organs and concomitantly with tissue destruction as reported in a previous study (24). Because SAP2 is activated in vitro when proteins are the sole nitrogen source, the Sap2 proteinase may allow C. albicans to thrive within the destroyed tissue by degrading host proteins for nutrient supply. Accordingly, no significant SAP2 expression was detected after i.v. infection with a lower dose, which resulted in relatively few organisms reaching the kidneys, unable to effect the same tissue destruction as seen with a fulminant infection. It is very intriguing that the reverse effect was seen with the SAP5 and SAP6 genes that may be needed for tissue invasion. With lower numbers of cells attacking the deep organs, the majority of invading C. albicans cells apparently were forced to activate these weapons, whereas induction of the proteinases in only a part of the fungal population seems to be sufficient when an overwhelming infection takes place. After hematogenous dissemination, activation of additional SAP genes also was detected, although this varied among different animals. SAP4 expression was consistently observed, but at lower levels than those seen for SAP5 and SAP6, which are highly homologous to SAP4, the three genes forming a subgroup within the C. albicans SAP gene family (7). SAP1 and SAP3 were not activated to high levels in any of the infection models used; nevertheless, significant expression of these genes was detected in some animals. Interestingly, SAP1 and SAP3 are phase-specific genes in the C. albicans strain WO-1, where they are expressed only in the opaque phase but not in the white phase (29). Although strain SC5314, from which our reporter strains are derived, does not display the white-opaque switching, a similar phenomenon may result in a phase-variable expression of the SAP1 and SAP3 genes in this strain. However, the possibility remains that expression of these genes might not need strong promoter activity because low-level transcription could be compensated for by enhanced transcript stability or enhanced translation. In this case, a transcriptional activation of SAP1 and SAP3 that could be relevant in vivo might not be sufficiently strong to result in FLP activity.
C. albicans colonizes and infects more host niches in addition to those analyzed in our present study, for example the oral cavity or the vagina. Because the environmental conditions at these sites differ from other locations, C. albicans probably adapts to these niches by the expression of different sets of SAP and other virulence genes (16, 30, 31), which is supported by the results obtained with specific mutants (32). As a consequence of the differential expression of individual SAP genes at various stages of the infection, one would expect that the individual SAP isoenzymes differ with respect to their biochemical properties, allowing the fungus to use the proteinase that is best adapted to a certain environment and for a specific function. Purification of some of the proteinases has indeed shown differences, for example in their pH optimum (33). The recent successful expression of individual SAP genes in a heterologous host (15) should allow the dissection of the functional differences of the various isoenzymes and relate their properties to the in vivo expression pattern within the host.
Acknowledgments
We thank Klaus Schröppel for providing the sequences of the SAP4–6 promoter regions. This study was supported by the Bundesministerium für Bildung, Wissenschaft, Forschung und Technologie (Grant O1 K1 8906-0) and the Deutsche Forschungsgemeinschaft (Grant MO 846/1-1). P.S. is the recipient of a grant from the Studienstiftung des deutschen Volkes.
Abbreviations
- MPA
mycophenolic acid
- SAP
secreted aspartic proteinase
- IVET
in vivo expression technology
Footnotes
This paper was submitted directly (Track II) to the PNAS office.
Article published online before print: Proc. Natl. Acad. Sci. USA, 10.1073/pnas.110031497.
Article and publication date are at www.pnas.org/cgi/doi/10.1073/pnas.110031497
References
- 1.Odds F C. Candida and Candidosis. London: Baillière Tindall; 1988. [Google Scholar]
- 2.Odds F C. Am Soc Microbiol News. 1994;60:313–318. [Google Scholar]
- 3.Klotz S A. Clin Infect Dis. 1991;14:340–347. doi: 10.1093/clinids/14.1.340. [DOI] [PubMed] [Google Scholar]
- 4.Calderone R A. Trends Microbiol. 1993;1:55–58. doi: 10.1016/0966-842x(93)90033-n. [DOI] [PubMed] [Google Scholar]
- 5.Hostetter M K. Am Soc Microbiol News. 1994;60:370–374. [Google Scholar]
- 6.Sundstrom P. Curr Opin Microbiol. 1999;2:253–257. doi: 10.1016/S1369-5274(99)80062-9. [DOI] [PubMed] [Google Scholar]
- 7.Monod M, Togni G, Hube B, Sanglard D. Mol Microbiol. 1994;13:357–368. doi: 10.1111/j.1365-2958.1994.tb00429.x. [DOI] [PubMed] [Google Scholar]
- 8.Monod M, Hube B, Hess D, Sanglard D. Microbiology. 1998;144:2731–2737. doi: 10.1099/00221287-144-10-2731. [DOI] [PubMed] [Google Scholar]
- 9.Staib F. Sabouraudia. 1965;4:187–193. doi: 10.1080/00362176685190421. [DOI] [PubMed] [Google Scholar]
- 10.Kwon-Chung K J K, Lehman D, Good C, Magee P T. Infect Immun. 1985;49:571–575. doi: 10.1128/iai.49.3.571-575.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cassone A, de Bernardis F, Mondello F, Ceddia T, Agatensi L. J Infect Dis. 1987;156:777–783. doi: 10.1093/infdis/156.5.777. [DOI] [PubMed] [Google Scholar]
- 12.Hube B. Rev Iberoam Micol. 1998;15:65–68. [PubMed] [Google Scholar]
- 13.Hube B, Monod M, Schofield D A, Brown A J P, Gow N A R. Mol Microbiol. 1994;14:87–99. doi: 10.1111/j.1365-2958.1994.tb01269.x. [DOI] [PubMed] [Google Scholar]
- 14.White T, Agabian N. J Bacteriol. 1995;177:5215–5221. doi: 10.1128/jb.177.18.5215-5221.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borg-von Zepelin M, Beggah S, Boggian K, Sanglard D, Monod M. Mol Microbiol. 1998;28:543–554. doi: 10.1046/j.1365-2958.1998.00815.x. [DOI] [PubMed] [Google Scholar]
- 16.Schaller M, Schäfer W, Korting H C, Hube B. Mol Microbiol. 1998;29:605–615. doi: 10.1046/j.1365-2958.1998.00957.x. [DOI] [PubMed] [Google Scholar]
- 17.Borg M, Rüchel R. Infect Immun. 1988;56:626–631. doi: 10.1128/iai.56.3.626-631.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valdivia R H, Falkow S. Trends Microbiol. 1997;5:360–363. doi: 10.1016/S0966-842X(97)01111-6. [DOI] [PubMed] [Google Scholar]
- 19.Camilli A, Beattie D T, Mekalanos J J. Proc Natl Acad Sci USA. 1994;91:2634–2638. doi: 10.1073/pnas.91.7.2634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santos M A, Ueda T, Watanabe K, Tuite M. Mol Microbiol. 1997;26:423–431. doi: 10.1046/j.1365-2958.1997.5891961.x. [DOI] [PubMed] [Google Scholar]
- 21.Leuker C E, Hahn A-M, Ernst J F. Mol Gen Genet. 1992;235:235–241. doi: 10.1007/BF00279365. [DOI] [PubMed] [Google Scholar]
- 22.Srikantha T, Chandrasekhar A, Soll D R. Mol Cell Biol. 1995;15:1797–1805. doi: 10.1128/mcb.15.3.1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morschhäuser J, Michel S, Hacker J. Mol Gen Genet. 1998;257:412–420. doi: 10.1007/s004380050665. [DOI] [PubMed] [Google Scholar]
- 24.Staib P, Kretschmar M, Nichterlein T, Köhler G, Michel S, Hof H, Hacker J, Morschhäuser J. Mol Microbiol. 1999;32:533–546. doi: 10.1046/j.1365-2958.1999.01367.x. [DOI] [PubMed] [Google Scholar]
- 25.Buchholz F, Angrand P-O, Stewart A F. Nat Biotechnol. 1998;16:657–662. doi: 10.1038/nbt0798-657. [DOI] [PubMed] [Google Scholar]
- 26.McCarthy J E G. Microbiol Mol Biol Rev. 1998;62:1492–1553. doi: 10.1128/mmbr.62.4.1492-1553.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Köhler G A, White T C, Agabian N. J Bacteriol. 1997;179:2331–2338. doi: 10.1128/jb.179.7.2331-2338.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Millon L, Manteaux A, Reboux G, Drobacheff C, Monod M, Barale T, Michel-Briand Y. J Clin Microbiol. 1994;32:1115–1118. doi: 10.1128/jcm.32.4.1115-1118.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.White T C, Miyasaki S H, Agabian N. J Bacteriol. 1993;175:6126–6133. doi: 10.1128/jb.175.19.6126-6133.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.de Bernardis F, Cassone A, Sturtevant J, Calderone R. Infect Immun. 1995;63:1887–1892. doi: 10.1128/iai.63.5.1887-1892.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Naglik J R, Newport G, White T C, Fernandes-Naglik L L, Greenspan J S, Greenspan D, Sweet S P, Challacombe S J, Agabian N. Infect Immun. 1999;67:2482–2490. doi: 10.1128/iai.67.5.2482-2490.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.de Bernardis F, Arancia S, Morelli L, Hube B, Sanglard D, Schäfer W, Cassone A. J Infect Dis. 1999;179:201–208. doi: 10.1086/314546. [DOI] [PubMed] [Google Scholar]
- 33.Smolenski G, Sullivan P A, Cutfield S M, Cutfield J F. Microbiology. 1997;143:349–356. doi: 10.1099/00221287-143-2-349. [DOI] [PubMed] [Google Scholar]