Abstract
Background:
Pyloric stenosis, the most common surgical condition of infants, is treated by longitudinal myotomy of the pylorus. Comparative studies to date between open and laparoscopic pyloromyotomy have been retrospective and report conflicting results. To scientifically compare the 2 techniques, we conducted the first large prospective, randomized trial between the 2 approaches.
Methods:
After obtaining IRB approval, subjects with ultrasound-proven pyloric stenosis were randomized to either open or laparoscopic pyloromyotomy. Postoperative pain management, feeding schedule, and discharge criteria were identical for both groups. Operating time, postoperative emesis, analgesia requirements, time to full feeding, length of hospitalization after operation, and complications were compared.
Results:
From April 2003 through March 2006, 200 patients were enrolled in the study. There were no significant differences in operating time, time to full feeding, or length of stay. There were significantly fewer number of emesis episodes and doses of analgesia given in the laparoscopic group. One mucosal perforation and one incisional hernia occurred in the open group. Late in the study, 1 patient in the laparoscopic group was converted to the open operation. A wound infection occurred in 4 of the open patients compared with 2 of the laparoscopic patients (P = 0.68).
Conclusions:
There is no difference in operating time or length of recovery between open and laparoscopic pyloromyotomy. However, the laparoscopic approach results in less postoperative pain and reduced postoperative emesis. In addition, there was a fewer number of complications in the laparoscopic group. Finally, patients approached laparoscopically will likely display superior cosmetic outcomes with long-term follow-up.
This prospective, randomized trial comparing laparoscopic with open pyloromyotomy demonstrated that both procedures are equally safe and effective while the laparoscopic approach results in less postoperative discomfort with fewer doses of analgesics and fewer episodes of emesis.
Infantile hypertrophic pyloric stenosis is the most common surgical condition in infants. Extramucosal longitudinal myotomy of the pylorus (Fredet-Ramstedt procedure) has long been the standard management. The first description of pyloromyotomy using the laparoscopic approach appeared in the literature in 1991.1 This report was followed by several small institutional series describing the 3-port technique as feasible and safe.2–7 An early review of these reported cases concluded that, assuming the surgeon was equally facile with both approaches, the laparoscopic technique was preferred over the open approach due to superior cosmesis and otherwise equal efficacy.8 Other series have compared the approaches with mixed results, including longer operative times and increased complication rates with the laparoscopic approach.9,10 Other reports have found equal operative times with decreased recovery time following the laparoscopic approach and have concluded that laparoscopy is the preferred technique.11,12 Still others have demonstrated the operations to be equal in operating time, recovery time, and complications.13,14 A recent meta-analysis of the available reports found that fewer complications occurred when the open approach was used, but a shorter recovery time was evident with laparoscopy.15 This meta-analysis emphasized the pressing need for a prospective randomized controlled trial to fully investigate these and other outcome measures. Herein, we present the first large prospective, randomized trial to compare laparoscopic and open pyloromyotomy.
METHODS
Approval was obtained from the Children's Mercy Hospital Internal Review Board (IRB) prior to enrolling patients in this study. Patients were subsequently enrolled only after obtaining consent from the patient's legal guardian. The consent forms and consent process were carefully evaluated by the IRB on a continual basis.
Participants
The study population consisted of infants with ultrasonographic findings consistent with idiopathic hypertrophic pyloric stenosis. Standard institutional sonographic criteria for the diagnosis of pyloric stenosis were used for diagnosis.
Patients older than 3 months were excluded due to their atypical presentation. Patients who were found to possess a contraindication to the laparoscopic approach in the opinion of either the anesthesiologist or the surgeon were not considered eligible for the study. Patients with significant comorbid conditions that would influence the postoperative course or those requiring an additional procedure during the operation were excluded.
Interventions
All operations were performed by one of the 7 institutional staff surgeons as dictated by the call schedule, and the operative approach was controlled by the randomization sequence described below. The randomization of the surgical approach was not influenced by the surgeon performing the operation.
Patients randomized to the open approach underwent a standard open pyloromyotomy according to the surgeon's personal technique without protocol specification. The laparoscopic operations were performed using a 5-mm umbilical port and the stab incision technique for the operating instruments as previously described.3,16 The basic steps of this technique are outlined in Figure 1.
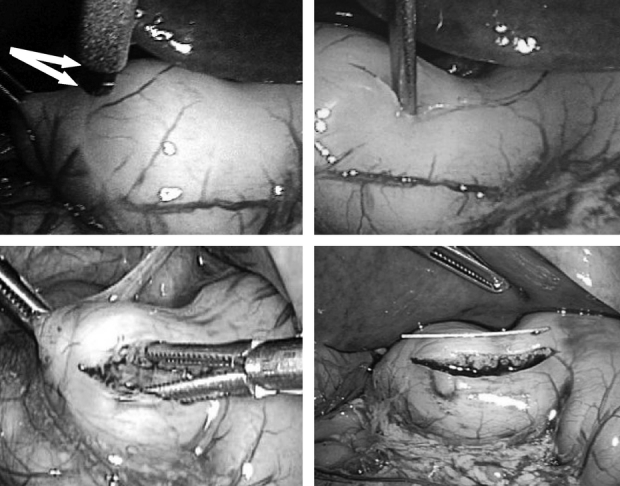
FIGURE 1. Left upper photograph demonstrates the retractable pyloromyotomy blade exposed to 2 mm (arrows). Right upper photograph shows the knife blade retracted and being used to initiate the pyloromyotomy. Left lower photograph depicts the pyloric spreader being used to complete the myotomy. The submucosa can be seen in the depths of the myotomy. Right lower photograph demonstrates the measurement of the pyloromyotomy: the white string is 2 cm in length.
Sample Size
Utilizing operative times obtained from retrospective data within our institution and assigning power at 0.80 and α of 0.05, a sample size of 60 patients in each arm was established. However, given that the potentially severe complication of this operation (mucosal perforation) occurs quite infrequently, and the desire to evaluate emesis episodes, length of stay, time to full feedings, and feeding failures, we felt increased enrollment was warranted to detect a potential difference in these important parameters. Therefore, we established a recruitment goal of 100 patients in each arm.
Assignment
An individual unit of randomization was used in a nonstratified sequence in blocks of 10. After consent for study enrollment was obtained, the randomization sequence was accessed to identify the next allotment. The operation was then discussed with the family as the allocated procedure could not be blinded to guardians or caregivers.
Protocol
Postoperative orders were controlled via a standard order set for all operations: All patients began a weight-controlled volume feeding schedule 2 hours after the completion of the operation. The schedule was advanced sequentially with 2 feedings of Pedialyte given 2 hours apart followed by 2 feedings of half-strength formula or breast milk given 2 hours apart follow by 2 feedings of full-strength formula or breast milk given 2 hours apart followed by ad libitum feeds or the previously used home feeding regimen. Patients with 2 emesis episodes at a given level on the feeding schedule were held at that level until they tolerated the feeds. More than 2 emesis episodes resulted in a “setback” and cessation of feeding for 6 hours with subsequent reinstitution of oral intake at the previous level.
Postoperative pain was assessed using the Neonatal Infant Pain Scale. Analgesia for all patients consisted of acetaminophen given at a dose of 10 mg/kg orally or per rectum up to every 4 hours as needed for pain.
Upon reaching ad libitum feeds, patients were discharged to home with a standard instruction set and a 2-week follow-up with the staff surgeon. During the postoperative period, a wound infection was defined as an incision felt to require drainage or antibiotics by a surgeon in the study.
Data Collection
Preoperative electrolytes, ultrasound measurements, operating time, operative and hospital complications, pyloromyotomy length, time to complete advancement of diet, number of episodes of emesis, number of feeding setbacks, doses of analgesia, length of postoperative hospitalization, operative charges, and hospital charges were recorded during the hospital stay. Any abnormal findings during the postoperative or follow-up visits were recorded.
Statistical Analysis
Continuous variables were compared using an independent sample, 2-tailed Student t test. Discrete variables were analyzed with Fisher exact test. Significance was defined as P value ≤0.05.
RESULTS
From April 2003 through March 2006, 200 patients were enrolled in the study.
Demographics
There was no difference in age or weight between the 2 groups. Sonographic parameters of the hypertrophied pylorus and presenting serum electrolytes were nearly identical (Table 1).
TABLE 1. Preoperative Data

Operation
There was no difference in operating time between the groups (Table 2). During the first 50 cases in the study, the laparoscopic approach took a mean time of 23 minutes 19 seconds compared with 18 minutes 19 seconds in the open group (P = 0.01). However, over the most recent 50 cases, the operative times were nearly identically between the 2 approaches with a mean time of 19 minutes 26 seconds in the laparoscopic group compared with 19 minutes 48 seconds in the open group (P = 0.89).
TABLE 2. Outcomes

Outcome
There was no difference in time to full oral intake or the length postoperative hospitalization between the 2 groups (Table 2). The laparoscopic group required significantly less doses of analgesia during their hospitalization (P = 0.0008, Table 2) and experienced fewer episodes of postoperative emesis (P = 0.05, Table 2). There was 1 mucosal perforation in the open group, which was recognized and repaired during the operation without subsequent sequelae. Late in the study, 1 laparoscopic case was converted to open because of concerns about bleeding. This patient was analyzed in the laparoscopic group on an intention-to-treat basis.
At follow-up, 1 incisional hernia was discovered in the open group which required an additional operation to repair the fascial defect. A wound infection occurred in 2 patients in the laparoscopic group compared with 4 patients in the open group, which was not significantly different (P = 0.68). The typical appearance of the abdomen 2 weeks after the laparoscopic approach is shown in Figure 2A and is compared with an abdomen after the open approach, seen in Figure 2B.

FIGURE 2. A, Typical postoperative appearance 1 year after laparoscopic pyloromyotomy. B, Two examples of open pyloromyotomy scar appearance. The photograph on the left was taken 2 weeks after surgery. The photograph on the right is another patient 6 months after surgery.
DISCUSSION
Current literature regarding pyloromyotomy for hypertrophic pyloric stenosis produces more questions than answers. This prospective study provides valuable information toward answering these questions.
Several retrospective studies have found laparoscopic pyloromyotomy takes longer to perform than the open procedure.9,14 This is clearly refuted in this study as there was no difference in operating time. We did, however, witness a decrease in operative time with laparoscopy over the course of the study, with the open technique significantly shorter for the first 50 cases. This is a common phenomenon recognized by others comparing a laparoscopic and open technique. The group of surgeons performing the operations in this current study had varying levels of laparoscopic expertise (2 had advanced laparoscopic skills), and there was clearly a period of adaptation for surgeons beginning to use the laparoscopic approach. This has been seen in prior retrospective reviews.11 One retrospective review not involving a learning curve for the surgeons involved actually found operative times to be shorter with laparoscopy.17 Importantly, it should be emphasized that while some retrospective series have found statistically significant differences in operative times, those differences exist as minutes and cannot be considered clinically relevant.
Early comparative studies of laparoscopic and open pyloromyotomy reported a higher complication rate, with laparoscopic pyloromyotomy leading to the conclusion that the operation is equal to the open approach only after the surgeon has incurred substantial experience.18 This conclusion resulted in the argument that the technical ability of performing a laparoscopic pyloromyotomy requires a period of learning and that this period should be respected prior to considering the laparoscopic approach to be as safe as the traditional open technique.9,18–20 Attempts to quantify this period of learning have estimated it to be about 30 cases.20
Our institution had previous experience with the laparoscopic approach for pyloromyotomy, which adds validity to the results of this prospective trial.21 At the start of this prospective study, because of this prior experience with laparoscopic pyloromyotomy, we felt we were equipped to embark on a prospective comparative study between the laparoscopic and open approach. The laparoscopic technique used by all surgeons in this study was the simple modification of the 3-port technique using stab incisions to pass the operating instruments directly through the abdominal wall.3,16 This method decreases operative time by removing the steps of cannula insertion, and decreases operative cost as only 1 disposable cannula is used for the procedure.16 The 2 stab incisions are much smaller than cannula incisions and heal in a nearly undetectable manner. Further, we feel the operation is easier to perform without the bulky ports consuming much of the precious operating space, which is quite small in these patients.
Several retrospective series have raised concerns that laparoscopic pyloromyotomy may potentially result in higher complication rates.9,10,17 This finding was not found in our study as the laparoscopic approach produced fewer complications and no mucosal perforations or incomplete pyloromyotomies. Although the difference in complication rates in our study was not significant, another group has reported more perforations with the open approach when examining their experience retrospectively.22 Others have brought attention to the possibility that laparoscopic pyloromyotomy may increase the chances of incomplete myotomy.23 In this study, we did not have an incomplete myotomy in either group. Further, the prior retrospective review of our laparoscopic pyloromyotomy experience in more than 170 patients documented a mean pyloromyotomy length of 1.9 cm without a single patient having an incomplete myotomy.21 When the results of our previous experience are combined with patients undergoing the laparoscopic approach in this current study, we have now performed more than 270 laparoscopic pyloromyotomies without a single incomplete pyloromyotomy or mucosal perforation. We did identify twice as many wound infections in the open group. A concern could be raised about the lack of antibiotic usage in this population. We designed this study based on our existing practice prior to its initiation. Because pyloromyotomy is a clean case, it has been our practice to not use antibiotics. Therefore, no patient in the study received antibiotics. The insignificant difference in wound infection is validated through the randomization sequence of the study; and although a larger accrual cohort may have eventually shown a statistical significance, it is doubtful that the significance would be clinically relevant in this population. Therefore, we continue to recommend no prophylactic antibiotic usage for pyloromyotomy.
Several retrospective series have found significantly shorter hospital stays after laparoscopic pyloromyotomy.11,12,15 While there was significantly less postoperative pain and fewer episodes of emesis in the laparoscopic group in this study, there was no difference in postoperative hospitalization. This can be attributed to the fact that, when the feeding regimen is prospectively controlled in both groups, the rate of advancement to discharge is not affected by the operative approach. There was a trend toward shorter hospitalization in the laparoscopic group; and with more patients enrolled, this difference would likely reach significance. However, this difference was only 4 hours and not clinically relevant. A comment should be made regarding the cost analysis between the 2 groups. Costs were collected for the groups; however at approximately patient 65, our institution changed the method for billing. Instead of billing for individual instrument packs, disposable instruments, reusable instruments, etc., we began billing the operating room charges by individual minutes, regardless of the instrumentation used during the operation. With the advent of the new billing method, we were unable to collect individual charges. When we calculated the charges based upon operating room time, as one can see from the data for operative times that there was no difference between the groups. Similarly, length of stay only varied by 4 hours between the 2 groups, and room charges are based on 24-hour increments. Therefore, no difference could be identified. In summary, we could not identify a difference in the cost of the 2 approaches because they all shared almost exactly the same operative times and length of stay.
There has been a move by some to obviate the cosmetic benefit for laparoscopy by performing the pyloromyotomy through a circumumbilical approach.17,24–26 While several reports have demonstrated this technique to be as safe as the open technique, most have found that the umbilical approach takes longer than either laparoscopy or an epigastric incision.17,24,25 The proposed advantage of the circumumbilical technique over laparoscopy is the absence of the 2 stab incisions.26 However, we have noticed that the portless stab technique results in incisions that are usually imperceptible at follow-up. Moreover, several of the surgeons participating in this current study have attempted the circumumbilical approach and have found an alarming number of serosal tears when trying to manipulate the hypertrophic pylorus down and through the umbilicus.
CONCLUSION
This is the only large prospective randomized trial comparing laparoscopic and open pyloromyotomy for pyloric stenosis. The data obtained in this controlled trial reveal that, in the hands of trained pediatric surgeons, the operative approach does not affect the length of recovery or complication rates associated with pyloromyotomy. However, the data support 2 benefits of the laparoscopic approach. First, there is reduced postoperative discomfort requiring significantly fewer doses of analgesics following the laparoscopic operation. Moreover, there were significantly fewer episodes of emesis with this technique compared with the open operation. Second, there is an obvious cosmetic benefit that will become more evident as these babies grow into adulthood. Although anecdotal, at the conclusion of this study, when asked which technique they would use in the future in their patients with pyloric stenosis, the 7 surgeons involved in this study unanimously agreed that they would use the laparoscopic approach unless an anesthetic contraindication existed.
ACKNOWLEDGMENTS
The authors thank Drs. Susan Sharp, Danny Little, KuoJen Tsao, Troy Spilde, Trish Valusek, Beverly Chaignaud, Stephen Shew, Suzanne Yoder, and George Gittes whose efforts made the completion of this study possible.
Discussions
Dr. Jay L. Grosfeld (Indianapolis, Indiana): I would like to note that I appreciated receiving this manuscript to review a week prior to the meeting. I want to applaud the group from Kansas City for establishing a center for prospective clinical trials in the Children's Hospital and for studying a common surgical problem that might provide data and be of value to many infants.
I think the study is of interest in that there are a fair number of patients in the study, 200, and there was absolutely no difference in the length of procedure, the length of hospital stay, or the complication rate. The open patients had a few more wound infections, 4 versus 2, but that was not significant. But perhaps if the cohort was larger, there might be some significance in infection observed.
The only differences noted in the study were more subjective in nature than objective. The number of vomiting episodes and more pain medication was required in open cases. It is well known that most infants following pyloromyotomy may have an episode of vomiting. The authors state in their manuscript that pain medication was given “as needed.” Babies cannot tell us when they hurt, so how is the need for pain assessed? What were the criteria to actually give pain medication if it wasn't routinely scheduled postoperatively?
The authors suggest that cost was compared in the study, but they failed to actually indicate what was the cost of the procedure. Since the length of the procedure and hospital stay was similar, and the complication rate wasn't different, what was the excess cost of using all the laparoscopic equipment? Was this a cost-effective procedure? In this era of evidence-based practice, does that indicate that one has to consider perhaps not doing it laparoscopically if it was much more expensive?
I think this is the first attempt to study pyloromyotomy prospectively, and I was very pleased to see this accomplished by our colleagues in Kansas City.
One last question is that we know that there is a slight increase in wound infection rates in patients with pyloric stenosis, more commonly when it is done through the umbilicus. Why weren't perioperative antibiotics used in the infants in this study?
Dr. Daniel J. Ostlie (Kansas City, Missouri): We will address the first question and last question together about wound infections. Certainly, there is a possibility, with a greater number of patients in the study, we would have seen a difference in the wound infection rate between the 2 groups. We chose operative time as our primary endpoint because this data point was known from our previous retrospective report and from our institutional data. This institutional data allowed us to calculate a power that we thought was appropriate for the study.
If one looks at complication rates as the primary endpoint and the complication happens between 2 and 4 times out of 100, the number of patients necessary for a valid study would be almost unobtainable. So this that is why—I don't disagree with your comment about the wound infection, but certainly it is probably not something that is reasonable to do or would be clinically relevant in the long term.
With regard to perioperative antibiotics, we did not utilize perioperative antibiotics in the open operation in our group prior to initiating the study and in order to keep the 2 groups equal and masked with regard to postoperative care we decided not to use antibiotics. It certainly is something that other institutions would use, and we don't question that. But in this case, we didn't do it beforehand and we just persisted with our normal routine during the study.
Pain medications are always difficult to assess, especially in babies that are between 1 month and 3 months of age. We use a pain scale that the nurses are very adept at using that looks at blood pressure, heart rate, what the babies’ facial expressions are, what their body postures are, and the nurses, when the manuscript says are allowed to give pain med on an as-needed basis, if that baby meets the criteria set forth utilizing that pain scale, which is a validated pain scale, they receive Tylenol on an as-needed basis.
It is interesting in having rounded on the vast majority of these patients the last 3 years that, talking to the nurses, they really don't differentiate between an open and a laparoscopic pyloromyotomy. So I can't sit here and say that it is 100% blinded because it not a double-blinded study, but the nurses, I don't think, engaged to the extent that, “Oh, this is an open pyloric and we absolutely have to give this baby more pain medicine than we would for a lap pyloric.”
And finally, the question about the cost. We did collect cost data. Unfortunately, in today's environment, we see shifting of cost. When we started this study, costs were all separated. About a third of the way through the study our hospital—and I am sure other institutions have done this—went to a per-minute cost basis in the operating room regardless what instruments are used. So there was no way for us at that point to collect cost for, let's say, laparoscopic instruments versus open instruments that were used. So we lost that ability. Once you fall into that category of looking at operative time, then cost becomes analogous with operative time. And as you saw, the operative times were differentiated by less than 10 seconds. So if you are billing based on a minute in the operating room, you are not going to see a cost difference. Similarly, if you are looking at hospital stay, where we found 4 hours in difference in stay, rather than a difference in days, you are not going to be able to generate a cost difference when you are billing on a 24-hour period. So although costs certainly in some institutions may be reasonable to differentiate, in our institution, we just weren't able to do it after the study started.
Dr. James A. O'Neill, Jr. (Nashville, Tennessee): I appreciate the opportunity to discuss this paper and the fact that Dr. Holcomb sent me the manuscript well ahead of time as did he with Dr. Grosfeld. I suspect that I was asked because I belong to the generation that did its best to perfect open pyloromyotomy.
Now, the first reference in this paper is 1991 when laparoscopic pyloromyotomy was first described. So this is a very current report. On the other hand, shame on us that it's taken 15 years to accomplish a randomized, controlled trial to see whether this is really an effective modality. And at least this paper goes a good distance in terms of answering some of those questions.
And I was particularly struck by the fact that they didn't just rely on statistical significance in their analyses, you have to read the paper to see this, but also clinical relevance in deciding whether something was meaningful or not, even if statistically significant.
Now, I think that they have proven pretty well that the procedures are about equal. There are a few less complications, vomiting and so forth, that are probably meaningful in the laparoscopic group.
I remember very clearly one of the prior presidents of the American Surgical Association, H. William Scott, saying that pyloromyotomy is one of the few perfect operations we have. He might be surprised today if he heard that this has been changed somewhat.
Now, I thought that there were 3 things that were pointed out that went beyond the necessary aims of this paper. The first was, with the laparoscopic approach: do not change the basic principles of the operation and with laparoscopic operations; otherwise, some of those principles of those operations are a bit abridged. The second thing is that he pointed out that there is a trick in this technique of only using one trocar, and by having better mobility of instrumentation, and obviously cheaper with less disposable trocars, the technique of using two stab wounds, I thought, was pretty neat and I think should obviously be noticed. So I simply say to the chiefs of surgery here who are searching for pediatric surgeons for their units, you'd better take note of this because this is the way the field is going.
I would like to ask you one single question. And that is: you did make reference to the fact that the operation is—that is laparoscopic pyloromyotomy—is contraindicated in some patients, didn't spell that out, and I think people here would be interested in those guidelines if you would share that with us.
Dr. Daniel J. Ostlie (Kansas City, Missouri): We did establish some contraindications and, interestingly, there were 2 patients that were not in the study based on those indications.
The first one was a patient that was born with gastroschisis that developed pyloric stenosis after primary closure and was not given the opportunity to be randomized because we didn't think that it would be fair to have him randomized into the laparoscopic arm as it may generate at a significant difference with regard to operating time when compared to an operation on a virgin abdomen versus a gastroschisis abdomen. So that was one of the contraindications that they couldn't be randomized into the laparoscopic arm.
There was another patient that was admitted with a dry hemoglobin of 6 g/dL and was in the ICU for a day before it was recognized that he had a pyloric stenosis. He had had a femoral line placed, and we didn't think that the patient's disease process would have been appropriate to be randomized in either arm just because it may skew that arm due to the atypical presentation and the severity of their disease at their presentation. Of the 200 patients that were actually enrolled, those were the only 2 that were not offered enrollment.
Dr. Philip L Glick (Buffalo, New York): I would like to compliment the authors on this paper. I do all of my pyloric cases laparoscopically at a pediatric surgical training program. However, I think it is important for trainees to also do open pylorics to learn haptic memory, which is something that helps laparoscopic surgeons to do safer surgery. Prior to doing laparoscopic pyloromyotomies I had done hundreds of open pylorics, and we believe our trainees should learn both techniques, also. At our center, one third of our pylorics are still done in an open fashion. Therefore, I question your final conclusion that all the surgeons at your hospital are now converting to laparoscopic technique. Who is going to teach the residents how to do these open if everyone in your center is going to do them laparoscopically?
Dr. Daniel J. Ostlie (Kansas City, Missouri): That is a great question. We have actually had this conversation in our department meetings since this study was completed, and we all agree that the laparoscopic approach is the way we are going to approach these patients. However, there are two senior surgeons who have agreed that when the fellows are on call, and if there is a family that doesn't have a significant bias toward the laparoscopic approach, they will occasionally do an open operation. Because, as we know, if you have never done an open pyloromyotomy and now you have to convert a laparoscopic pyloromyotomy, that is not the time to be learning how to the open technique. So, we as a department have to make an effort to make sure that the fellows get 6, 10, however many open pyloromyotomies it takes to be able to perform it safely, or to salvage an operation that was started laparoscopically, if necessary.
But it is a great point that you can't just abandon it, and it goes back to Dr. O'Neill's point that you have got to be able to do the laparoscopic operation as well as you do the open operation, and if you can't do the open operation, you may not be serving your patient in the best interest by doing it laparoscopically.
Dr. Keith Georgeson (Birmingham, Alabama): I want to congratulate you for doing something we rarely do in pediatric surgery, and that is to have a randomized study, and also to ask you something. We started doing pyloromyotomies laparoscopically 11 years ago and during the 1990s we more than doubled the referrals for pyloromyotomy in our institution. I wonder if you saw the same increase in referrals for pyloric stenosis.
The other thing is: we have done over 700 of these now and we do have a few inadequate pyloromyotomies and a few perforations. And I wonder how you were able to do this with no complications whatsoever in the pyloric arm, especially in a teaching institution.
Dr. Daniel J. Ostlie (Kansas City, Missouri): To the first question about the referrals, I don't know that I can honestly answer that, Dr. Georgeson. In our area, we collect 90% to 95% of all the pediatric patients that exist, so the referral basis for a pyloric stenosis isn't going elsewhere. It is not as if patients from eastern Colorado or eastern Missouri are going to come to Kansas City specifically to get their pyloric stenosis repaired. So I don't know that we can look at that and say that we have had an increase in referrals. I certainly haven't appreciated it.
The second question about not having incomplete pyloromyotomies and not having perforation, we have done about 400 now with the previously mentioned study that was included in the talk. Part of that I am sure is luck. At some point, we will have an incomplete pyloromyotomy. We utilize the 2-cm rule, which has served us very well. In our experience that we reported in the surgery reference, a 2-cm pyloromyotomy has resulted in a 100% complete pyloromyotomy rate. But as we know, especially people that take care of these patients, the pylorus is a little different in every patient, and so we may get to that point where we have the 3-cm pylorus and we don't divide it completely. We just haven't had it.
As for perforations, we are just very careful. We take the senior residents and the fellows through the laparoscopic operation in a meticulous fashion. They all have to assist us several times before we allow them to perform the operation with us assisting them. We show them how we use the spreader, not to go too aggressively to expose the mucosa at any point during the pyloromyotomy not just at the duodenal pyloric junction, but also on the antral aspect. So, I think it is the meticulous nature, as well as luck.
Dr. Thomas M. Krummel (Stanford, California): I would like to congratulate the authors for doing something that we don't do very often, and that is a randomized, controlled trial of two different surgical techniques, that is nontrivial. I am impressed that you got it through your IRB.
Could you tell us how families reacted when you told them you didn't know what operation their child was going to get? Did all families accept the random assignment? And what were the realities of that conversation? Finally, if one of your nurses has a kid with pyloric stenosis, which way do you think they would prefer you to do it?
Dr. Daniel J. Ostlie (Kansas City, Missouri): Interestingly, if you look at the people that didn't go through the study, it was a split group. You had the group that was the Internet families that knew everything about laparoscopy. That was the way they were going to have it and it didn't make a difference what you told them. Then there was a second group, which was not insignificant, of about 30 patients, approximately 15% we lost. In that second group, they were having it the way dad had it or they were having it the way brother had it, which was open, and they aren't going to have it performed laparoscopically no matter what you thought.
Regarding consent, I hate to say it became an art, but it really does become an art on how you consent them. You need to get them to understand what your goals are. If you approach them with just a consent, and they think they are a study number or a guinea pig, it is not going to happen.
Early in the enrollment, we lost a lot of patients until we figured out that we need to present the data as unbiased as possible. You need to explain to the families that the primary goal is to collect the data that is generated from the study and not to put their child at risk or to try and tell them one arm is superior.
At the beginning, we tried to not bias our statements by not saying which arm we preferred. We just got better at the consent process. We actually saw an enrollment increase toward the end of the study where we were enrolling 95% of the patients. Families enrolled appropriately; they weren't guided or misguided. I believe that there was a true enrollment because of developing the art of consent.
This concept is supported now with 5 other prospective randomized trials ongoing with steady enrollment. We have continued to improve, and the IRB receives and approves the prospective trials because we have gone through it so many times.
The nurses in the operating room would have the laparoscopic pyloric in a minute, no doubt about it. As I said before, I don't think the floor nurses really differentiate the 2 approaches. I don't think they understand what happens because they don't see how quick the laparoscopic operation is and how little trauma it inflicts. The nurses in the clinic would all have laparoscopic pyloromyotomies, no doubt about it, because they have seen the incisional differences postoperatively.
Footnotes
Reprints: Daniel J. Ostlie, MD, Department of Pediatric Surgery, Children's Mercy Hospital, 2401 Gillham Road, Kansas City, MO 64108. E-mail: dostlie@cmh.edu.
REFERENCES
- 1.Alain JL, Grousseau D, Terrier G. Extramucosal pyloromyotomy by laparoscopy. Surg Endosc. 1991;5:174–175. [DOI] [PubMed] [Google Scholar]
- 2.Greason KL, Thompson WR, Downey EC, et al. Laparoscopic pyloromyotomy for infantile hypertrophic pyloric stenosis: report of 11 cases. J Pediatr Surg. 1995;30:1571–1574. [DOI] [PubMed] [Google Scholar]
- 3.Bufo AJ, Merry C, Shah R, et al. Laparoscopic pyloromyotomy: a safer technique. Pediatr Surg Int. 1998;13:240–242. [DOI] [PubMed] [Google Scholar]
- 4.Alain JL, Grousseau D, Longis B, et al. Laparoscopic pyloromyotomy for infantile hypertrophic stenosis. J Pediatr Surg. 1996;31:1197–1198. [DOI] [PubMed] [Google Scholar]
- 5.Hamada Y, Tsui M, Kogata M, et al. Surgical technique of laparoscopic pyloromyotomy for infantile hypertrophic pyloric stenosis. Surg Today. 1995;25:754–756. [DOI] [PubMed] [Google Scholar]
- 6.Najmaldin A, Tan HL. Early experience with laparoscopic pyloromyotomy for infantile hypertrophic pyloric stenosis. J Pediatr Surg. 1995;30:37–38. [DOI] [PubMed] [Google Scholar]
- 7.Hendrickson RJ, Yu S, Bruny JL, et al. Early experience with laparoscopic pyloromyotomy in a teaching institution. JSLS. 2005;9:386–388. [PMC free article] [PubMed] [Google Scholar]
- 8.Downey EC Jr. Laparoscopic pyloromyotomy. Semin Pediatr Surg. 1998;7:220–224. [DOI] [PubMed] [Google Scholar]
- 9.Sitsen E, Bax NM, van der Zee DC. Is laparoscopic pyloromyotomy superior to open surgery? Surg Endosc. 1998;12:813–815. [DOI] [PubMed] [Google Scholar]
- 10.Campbell BT, McLean K, Barnhart DC, et al. A comparison of laparoscopic and open pyloromyotomy at a teaching hospital. J Pediatr Surg. 2002;37:1068–1071. [DOI] [PubMed] [Google Scholar]
- 11.Fujimoto T, Lane GJ, Segawa O, et al. Laparoscopic extramucosal pyloromyotomy versus open pyloromyotomy for infantile hypertrophic pyloric stenosis: which is better? J Pediatr Surg. 1999;34:370–372. [DOI] [PubMed] [Google Scholar]
- 12.Scorpio RJ, Tan HL, Hutson JM. Pyloromyotomy: comparison between laparoscopic and open surgical techniques. J Laparoendosc Surg. 1995;5:81–84. [DOI] [PubMed] [Google Scholar]
- 13.Caceres M, Liu D. Laparoscopic pyloromyotomy: redefining the advantages of a novel technique. JSLS. 2003;7:123–127. [PMC free article] [PubMed] [Google Scholar]
- 14.Hall NJ, Ade-Ajayi N, Al-Roubaie J, et al. Retrospective comparison of open versus laparoscopic pyloromyotomy. Br J Surg. 2004;91:1325–1329. [DOI] [PubMed] [Google Scholar]
- 15.Hall NJ, Van Der Zee J, Tan HL, et al. Meta-analysis of laparoscopic versus open pyloromyotomy. Ann Surg. 2004;240:774–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ostlie DJ, Holcomb GW 3rd. The use of stab incisions for instrument access in laparoscopic operations. J Pediatr Surg. 2003;38:1837–1840. [DOI] [PubMed] [Google Scholar]
- 17.Kim SS, Lau ST, Lee SL, et al. Pyloromyotomy: a comparison of laparoscopic, circumumbilical, and right upper quadrant operative techniques. J Am Coll Surg. 2005;201:66–70. [DOI] [PubMed] [Google Scholar]
- 18.van der Bilt JD, Kramer WL, van der Zee DC, et al. Laparoscopic pyloromyotomy for hypertrophic pyloric stenosis: impact of experience on the results in 182 cases. Surg Endosc. 2004;18:907–909. [DOI] [PubMed] [Google Scholar]
- 19.Ford WD, Crameri JA, Holland AJ. The learning curve for laparoscopic pyloromyotomy. J Pediatr Surg. 1997;32:552–554. [DOI] [PubMed] [Google Scholar]
- 20.Kim SS, Lau ST, Lee SL, et al. The learning curve associated with laparoscopic pyloromyotomy. J Laparoendosc Adv Surg Tech A. 2005;15:474–477. [DOI] [PubMed] [Google Scholar]
- 21.Ostlie DJ, Woodall CE, Wade KR, et al. An effective pyloromyotomy length in infants undergoing laparoscopic pyloromyotomy. Surgery. 2004;136:827–832. [DOI] [PubMed] [Google Scholar]
- 22.Scorpio RJ, Beasley SW. Pyloromyotomy: why make an easy operation difficult? J R Coll Surg Edinb. 1993;38:299–301. [PubMed] [Google Scholar]
- 23.Yagmurlu A, Barnhart DC, Vernon A, et al. Comparison of the incidence of complications in open and laparoscopic pyloromyotomy: a concurrent single institution series. J Pediatr Surg. 2004;39:292–296. [DOI] [PubMed] [Google Scholar]
- 24.Blumer RM, Hessel NS, van Baren R, et al. Comparison between umbilical and transverse right upper abdominal incision for pyloromyotomy. J Pediatr Surg. 2004;39:1091–1093. [DOI] [PubMed] [Google Scholar]
- 25.Podevin G, Missirlu A, Branchereau S, et al. Umbilical incision for pyloromyotomy. Eur J Pediatr Surg. 1997;7:8–10. [DOI] [PubMed] [Google Scholar]
- 26.Shankar KR, Losty PD, Jones MO, et al. Umbilical pyloromyotomy: an alternative to laparoscopy? Eur J Pediatr Surg. 2001;11:8–11. [DOI] [PubMed] [Google Scholar]


