Abstract
Objective:
To assess the feasibility and safety of selective nonoperative management in penetrating abdominal solid organ injuries.
Background:
Nonoperative management of blunt abdominal solid organ injuries has become the standard of care. However, routine surgical exploration remains the standard practice for all penetrating solid organ injuries. The present study examines the role of nonoperative management in selected patients with penetrating injuries to abdominal solid organs.
Patients and Methods:
Prospective, protocol-driven study, which included all penetrating abdominal solid organ (liver, spleen, kidney) injuries admitted to a level I trauma center, over a 20-month period. Patients with hemodynamic instability, peritonitis, or an unevaluable abdomen underwent an immediate laparotomy. Patients who were hemodynamically stable and had no signs of peritonitis were selected for further CT scan evaluation. In the absence of CT scan findings suggestive of hollow viscus injury, the patients were observed with serial clinical examinations, hemoglobin levels, and white cell counts. Patients with left thoracoabdominal injuries underwent elective laparoscopy to rule out diaphragmatic injury. Outcome parameters included survival, complications, need for delayed laparotomy in observed patients, and length of hospital stay.
Results:
During the study period, there were 152 patients with 185 penetrating solid organ injuries. Gunshot wounds accounted for 70.4% and stab wounds for 29.6% of injuries. Ninety-one patients (59.9%) met the criteria for immediate operation. The remaining 61 (40.1%) patients were selected for CT scan evaluation. Forty-three patients (28.3% of all patients) with 47 solid organ injuries who had no CT scan findings suspicious of hollow viscus injury were selected for clinical observation and additional laparoscopy in 2. Four patients with a “blush” on CT scan underwent angiographic embolization of the liver. Overall, 41 patients (27.0%), including 18 cases with grade III to V injuries, were successfully managed without a laparotomy and without any abdominal complication. Overall, 28.4% of all liver, 14.9% of kidney, and 3.5% of splenic injuries were successfully managed nonoperatively. Patients with isolated solid organ injuries treated nonoperatively had a significantly shorter hospital stay than patients treated operatively, even though the former group had more severe injuries. In 3 patients with failed nonoperative management and delayed laparotomy, there were no complications.
Conclusions:
In the appropriate environment, selective nonoperative management of penetrating abdominal solid organ injuries has a high success rate and a low complication rate.
This is a prospective study of 152 patients with 185 penetrating solid organ injuries. Overall, 41 patients (27.0%), including 18 cases with grade III or V injuries, were successfully managed without a laparotomy and without any abdominal complication. Patients with isolated solid organ injuries treated nonoperatively had a significantly shorter hospital stay than patients treated operatively, even though the former group had more severe injuries. It is concluded that, in the appropriate hospital environment, selective nonoperative management of penetrating abdominal solid organ injuries is safe and has a high success rate.
Nonoperative management of blunt trauma to solid intra-abdominal organs (liver, spleen, kidney) has been the standard of care for many years. However, the concept of selective nonoperative management for penetrating solid organ injuries has remained largely unexplored and operative management is considered as the standard of care by most surgeons. The Los Angeles County and University of Southern California (LAC+USC) Trauma Center has been practicing nonoperative management of selected patients with penetrating solid organ injuries for more than 12 years. The present prospective study evaluated the safety and success rate of nonoperative management of penetrating injuries to the liver, spleen, or kidney.
PATIENTS AND METHODS
This prospective study was performed at the LAC + USC Trauma Center over a 20-month period (May 2004 to January 2006). The study included all patients with penetrating trauma to the liver, spleen, or kidney, diagnosed at laparotomy or by CT scan evaluation. The protocol for the evaluation and management of penetrating abdominal injuries is shown in Figure 1. Patients with hemodynamic instability, peritonitis (rigidity, rebound tenderness, significant tenderness away from the wound), associated head or spinal cord injury, or those who required an extra-abdominal operation under general anesthesia were selected for emergent laparotomy.
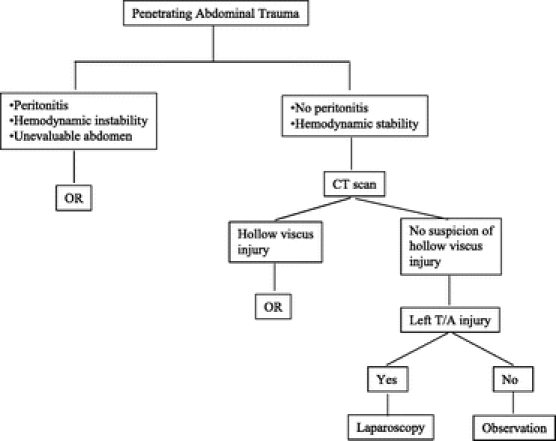
FIGURE 1. Algorithm for the management of penetrating abdominal trauma.
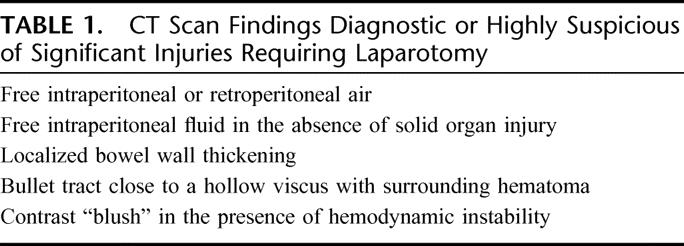
Clinically evaluable patients who were hemodynamically stable and had no signs of peritonitis were evaluated by CT scan with intravenous contrast. No routine oral or rectal contrast was administered. The entry and in the appropriate cases the exit site of the bullet were marked with external markers. The whole abdomen between the lower chest and pubic symphysis was scanned. The area between the marked entry and exit site or retained bullet was scanned with 3-mm slices. The following findings were considered as diagnostic or highly suspicious signs of hollow viscus injury: free intraperitoneal or retroperitoneal air, free intraperitoneal fluid in the absence of solid organ injury, localized bowel wall thickening, or bullet tract close to a hollow viscus with surrounding hematoma. The presence of contrast “blush” was considered as a significant finding suggestive of active bleeding or false aneurysm and, depending on the hemodynamic condition of the patient, an operation or angiographic evaluation was performed (Table 1). In the absence of CT scan findings suggestive of hollow viscus injury, all patients with penetrating solid organ injury were selected for nonoperative management. Patients with left thoracoabdominal injuries underwent delayed laparoscopic evaluation (>8 hours after admission) to rule out diaphragmatic injury and any diaphragmatic perforation was repaired laparoscopically. All observed patients were admitted to a monitored area, which is also the base station of the trauma team on call. The observation included serial clinical examinations of the abdomen and monitoring of blood pressure, pulse rate, hemoglobin, and white cell count. No prophylactic antibiotics or narcotic analgesic drugs were administered. If signs of peritonitis or a significant drop of the hemoglobin requiring acute blood transfusion occurred, an operation was performed. Otherwise, the patient was discharged 24 to 48 hours after admission, unless associated injuries required further inpatient care.
TABLE 1. CT Scan Findings Diagnostic or Highly Suspicious of Significant Injuries Requiring Laparotomy
The following data were collected for the purpose of the study: age, gender, mechanism of penetrating trauma (gunshot wound or stab wound), blood pressure and heart rate on admission, signs of peritonitis on initial evaluation, first hemoglobin, FAST results, chest x-ray, CT scan and laparoscopic findings, injured solid organ (liver, spleen or kidney), AAST grade of solid organ injury, time from admission to laparotomy, operative findings, type of surgical management, blood transfusion requirements, ICU and hospital stay, survival, and abdominal and extra-abdominal complications. The study was approved by the hospital's IRB.
RESULTS
During the study period, there were 152 patients with 185 penetrating abdominal solid organ injuries diagnosed at laparotomy or by CT scan. Gunshot injuries accounted for 70.4% (107 patients) and stab wounds for the remaining 29.6% (45 patients). The liver was the most commonly injured solid organ (73.0%) followed by the kidney (30.3%) and the spleen (30.3%). Thirty-three patients (21.7%) had more than one solid organ injury.
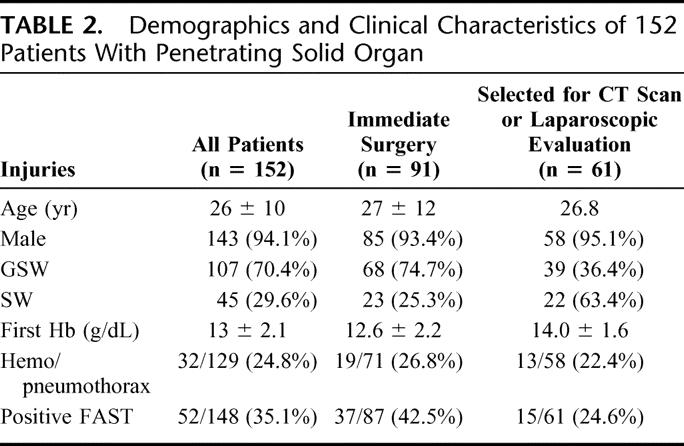
Overall, 91 patients (59.9%) had signs of peritonitis, hemodynamic instability, other major extraperitoneal injuries requiring an operation or spinal cord or head trauma and underwent an emergency laparotomy. The remaining 61 patients (40.1%) were selected for CT scan evaluation and 2 patients with left thoracoabdominal injuries were planned for elective laparoscopy. The epidemiologic characteristics and initial clinical presentation of the 2 groups of patients are shown in Table 2. Overall, 10 patients (6.6%) were hypotensive (systolic blood pressure <90 mm Hg) on admission, 7 (4.6%) had a first hemoglobin level <9 g/dL and 52 (34.2%) had a positive FAST (Table 2).
TABLE 2. Demographics and Clinical Characteristics of 152 Patients With Penetrating Solid Organ
Immediate Operation Group
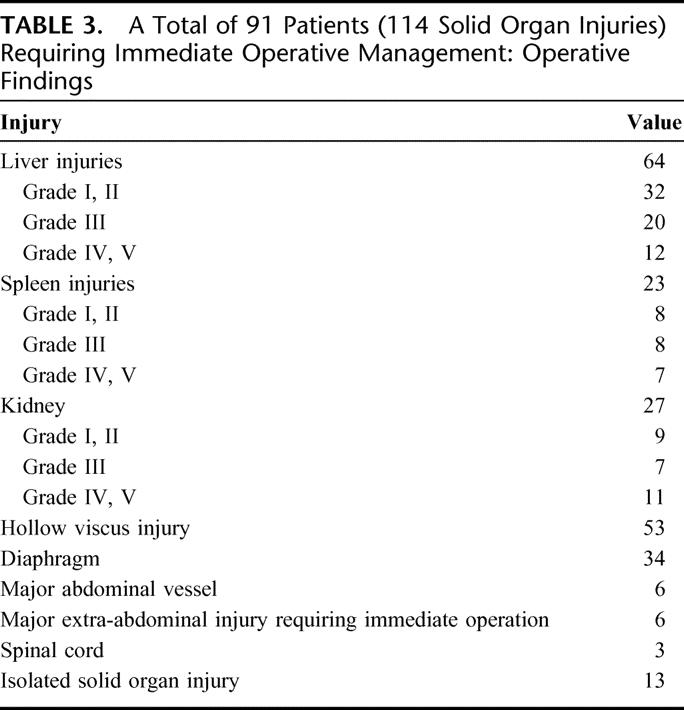
Ninety-one patients (59.9%) underwent an emergency laparotomy because of signs of peritonitis, hemodynamic instability, or clinically unevaluable abdomen. The mean time from admission to operation was 30 minutes (range, 5–118 minutes). There were 114 solid organ injuries. The liver was injured in 64 (70.3%) cases, the spleen in 23 (25.3%), and the kidney in 27 (29.7%). In 23 cases (25.3%), there was more than one solid organ injury. Forty-nine (43.0%) of the solid organ injuries were minor (grades I, II), 35 (30.7%) moderate (grade III), and 30 (26.3%) severe (grades IV, V). An associated hollow viscus injury was found in 53 patients (58.2%), a diaphragmatic injury in 34 (37.4%), pancreas in 3 (3.3%), a major vessel in 6 (6.6%), spinal cord injury in 3 (3.3%), severe head trauma in 1 (1.1%), and major extra-abdominal injuries requiring thoracotomy or neck exploration in 6 (6.6%). Thirteen patients (14.3%) had isolated solid organ injuries (Table 3).
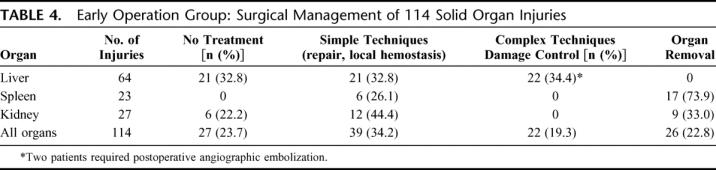
TABLE 3. A Total of 91 Patients (114 Solid Organ Injuries) Requiring Immediate Operative Management: Operative Findings
In 27 (23.7%) of the 114 solid organ injuries, there was no active bleeding at the time of operation and no specific treatment was considered necessary. In 39 (34.2%) cases, the injured solid organs were managed by simple surgical techniques such as suturing and/or local hemostatic agents and in 22 (19.3%) with complex techniques and packing for damage control. Postoperative angiographic embolization was required in 2 cases (1.8%). Of the 64 liver injuries, 21 (32.8%) did not need any treatment, 21 (32.8%) required simple surgical techniques, and 22 (34.4%) needed damage control procedures. Two patients (3.1%) required angiographic embolization immediately after the operation. Of the 23 splenic injuries, 17 (73.9%) underwent splenectomy and 6 (26.1%) repair. Of the 27 kidney injuries, a nephrectomy was performed in 9 (33.0%), repair in 12 (44.4%), and no exploration in 6 (22.2%) (Table 4).
TABLE 4. Early Operation Group: Surgical Management of 114 Solid Organ Injuries
The overall mortality was 16.5% (15 deaths). Only 2 deaths were directly related to liver injuries. The remaining 13 deaths had other major associated cardiovascular injuries. Fourteen deaths occurred within 24 hours due to massive hemorrhage and 1 death occurred on day 27 due to sepsis and multiorgan failure. There were no deaths in the 13 patients with isolated solid organ injuries.
Overall, 12 patients (13.2%) developed 20 complications. Eleven patients (12.1%) developed 14 abdominal complications. The incidence of abdominal complications was 6.3% in liver, 17.4% in spleen, and 14.8% in kidney injuries.
Patients Selected for CT Scan Evaluation
Sixty-one patients (40.1%) did not meet the protocol criteria for immediate operation and were selected for evaluation with CT scan. Two patients developed peritoneal signs after admission and were operated on before CT evaluation. The first had an isolated grade II stab wound to the liver and the second had a gunshot wound to the liver (grade IV) with associated stomach and colon injuries. Both patients had an uneventful recovery without any complications. A third patient did not undergo a CT scan in violation of the protocol. This patient required a laparotomy 19 hours after admission and a grade III liver injury was repaired with deep sutures and packing. The recovery was uneventful.
In the remaining 58 patients, the CT scan evaluation showed liver injury in 42, splenic injury in 5, and renal injury in 19 patients. Eight patients had more than one solid organ injury. In 15 patients, the CT scan findings were suspicious for hollow viscus or diaphragmatic injury and an exploratory laparotomy was performed. Forty-three patients (28.3% of all patients) with 47 diagnosed solid organ injuries were selected for either semi-elective laparoscopy to rule out diaphragmatic injury or clinical observation (Table 5; Fig. 2). Eighteen (41.9%) of this group of patients had at least one solid organ with severe injury (grades III-V). These severe injuries included 15 liver and 3 renal lesions. Two patients with left thoracoabdominal injuries underwent laparoscopic evaluation, which showed a diaphragmatic injury. Both patients had a successful laparoscopic repair of the diaphragm. The remaining 41 patients were clinically observed. Two patients with gunshot wounds failed nonoperative management and required laparotomy 41.3 and 41.5 hours after admission. The first patient had a minor splenic and colon injury and the CT scan was diagnostic but was delayed in violation of the protocol. The second patient had kidney and diaphragm injuries. Both patients had an uneventful recovery (Table 6). Four patients (3 with grade IV and 1 with grade III liver injuries) had angio-embolization of a false aneurysm or suspected active bleeding which were diagnosed on CT scan.
TABLE 5. Patients and Severity of Solid Organ Injuries Selected for Nonoperative Management (n = 43)
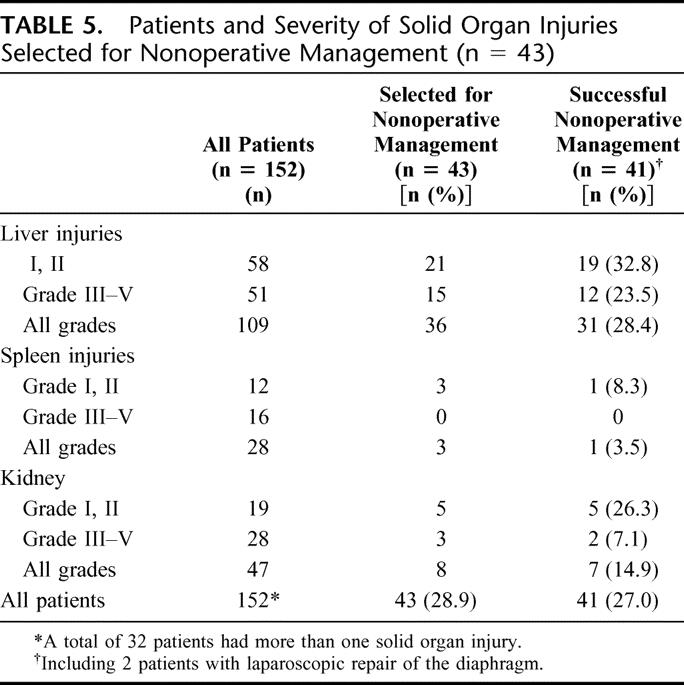
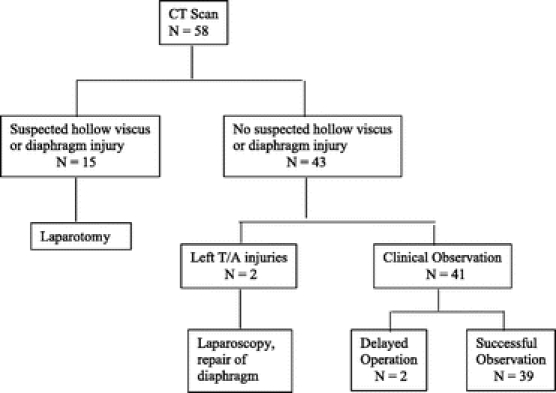
FIGURE 2. CT scan evaluation of penetrating solid organ injuries.
TABLE 6. Failure of Nonoperative Management
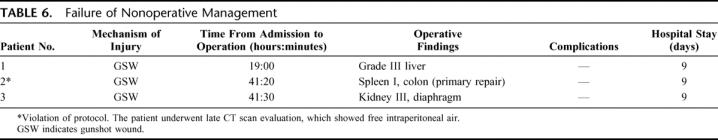
Overall, 39 patients (25.7% of all patients) with 42 solid organ injuries were successfully managed nonoperatively (Fig. 2). Including the 2 patients who underwent laparoscopic repair of the diaphragm, 41 patients (27.0%) successfully avoided a laparotomy. Overall, 28.4% of all injuries to the liver, 14.9% of kidney, and 3.5% of splenic injuries were successfully managed nonoperatively. There were no deaths or complications in the group of patients selected for nonoperative management, including the 3 patients who failed observation (Table 6).
Solid Organ Management
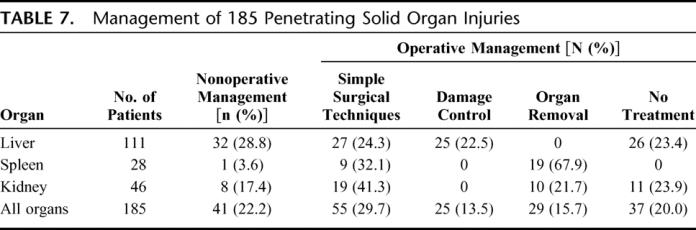
Table 7 shows the specific management of all 185 solid organ injuries, treated operatively or nonoperatively. Overall, 42.2% of the injuries did not require an operation or at laparotomy no specific treatment of the solid organ injury was needed. On the other extreme, 22.5% of liver injuries required complex procedures and damage control techniques to control bleeding.
TABLE 7. Management of 185 Penetrating Solid Organ Injuries
Isolated Solid Organ Injuries
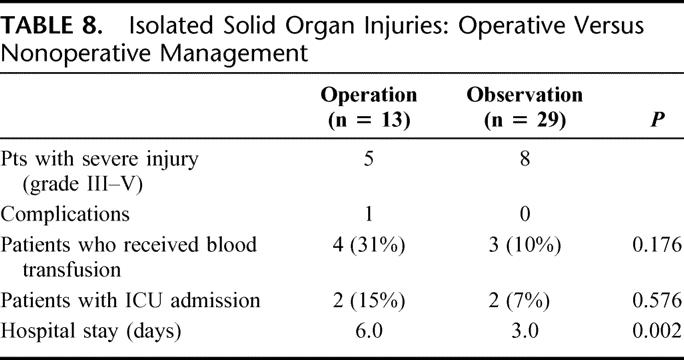
There were 42 patients with isolated solid organ injuries (29 with grades I or II and 13 with grade III-V injuries). Twenty-nine of these patients (69.0%) were successfully managed nonoperatively. Eight of the patients who were managed nonoperatively had severe (grades III-V) injuries (including 3 patients with grade IV injury), as compared with only 2 patients (both with grade III injury) in the group undergone operation. No complications occurred in the group of 29 patients who were managed nonoperatively. One patient (7.7%) in the operative management group developed an abdominal complication. This patient had a grade IV renal injury and developed urine leak, requiring hospitalization for 17 days. The mean hospital stay was 3.0 days in the observed group and 6.0 days in the group which underwent laparotomy (P = 0.002, Mann-Whitney U test), even though the observed group included more severe injuries (Table 8).
TABLE 8. Isolated Solid Organ Injuries: Operative Versus Nonoperative Management
DISCUSSION
Selective nonoperative management of stab wounds to the abdomen has become the standard of care nationwide. About 50% of stab wounds to the anterior abdomen and about 85% of stab wounds to the posterior abdomen can safely be managed nonoperatively.1,2 Even in the presence of peritoneal violation, a significant number of patients have no major intra-abdominal injury requiring operation. In a prospective study of 476 patients with stab wounds and proven peritoneal penetration, 27.6% had no significant intra-abdominal injury.1
The management of gunshot injuries to the abdomen has remained unchanged for many decades, with mandatory laparotomy being the standard practice. However, this concept has been challenged and some centers with extensive experience with penetrating injuries practice a selective nonoperative management.3–10 Approximately 30% of abdominal gunshot wounds to the anterior abdomen and about 67% of gunshot wounds to the back can safely be managed nonoperatively.4,5
Selective nonoperative management of blunt trauma to intra-abdominal solid organs has been established as the only acceptable standard of care. The success rate of nonoperative management ranges from 60% to about 90%.11–16 However, the role of nonoperative management in penetrating solid organ injuries has not been widely explored and routine laparotomy remains the usual practice. The first report of selective nonoperative management of penetrating injuries to the liver was published in 1986. In a prospective study of 63 patients with stab wounds to the liver, 33% were successfully managed nonoperatively.17 In a subsequent study by Renz and Feliciano in 1995, the authors reported 13 patients with gunshot wounds to the liver who were successfully managed nonoperatively.18 Another study from our center, in 1997, suggested that not all gunshot wounds to the liver need operation.4 Ginzburg et al10 in 1998 reported 4 cases with gunshot wounds to the liver who were successfully managed nonoperatively. In 1999, our program reported successful nonoperative management in 21% of 52 patients with isolated gunshot wounds to the liver.19 The present study has shown that 28.4% of patients with penetrating injuries to the liver, mainly gunshot wounds, can safely be managed nonoperatively. Even in severe injuries (grades III-V), 23.5% of patients were successfully managed nonoperatively. Interventional radiology with angiographic embolization may play a critical role in the successful management of these patients. Four patients in our series with CT scan “blush” were successfully managed with angiographic embolization.
Renal injuries are theoretically more amenable to nonoperative management than other intra-abdominal solid organ injuries. The retroperitoneal position of the kidneys may contain bleeding, and the rich blood supply may promote healing even after severe parenchymal injuries. The success rate of nonoperative management of blunt renal trauma not involving the renal vessels has been reported as high as 95%.20 Small series of successful nonoperative management of patients with stab wounds to the kidneys were published as far back as 1985.21,22 A more recent study by Wessells et al23 suggested that grade II penetrating renal injuries can successfully be managed nonoperatively. In a retrospective review of 200 renal stab wounds treated at the San Francisco General Hospital over a 20-year period, Armenakas et al24 reported successful nonoperative management in about 50% of the patients. Gunshot wounds are significantly more likely to result in severe kidney injuries than stab wounds.23 However, in our experience, even with gunshot injuries, in nearly 40% of the cases there is no need for surgical exploration of the kidney unless there is a hilar injury or continuous bleeding.25 Routine exploration of the injured kidney may result in the unnecessary loss of the kidney. The loss of a kidney, especially in the presence of other major associated injuries or septic complications, may increase the risk of renal failure. In the present study, 14.9% of all patients with penetrating kidney injuries (or 50% of patients with isolated injuries) were successfully managed nonoperatively.
There is very little published work on the safety and feasibility of the nonoperative management in penetrating splenic injuries. Pachter et al26 in 1998 reported 6 cases with stab wounds to the spleen managed nonoperatively. In the current study, the success rate was only 8.3% for minor injuries (grades I, II), and 0% in severe injuries. The high incidence of associated hollow viscus or diaphragm injury (89.3%) precludes the liberal application of nonoperative management for these injuries. Laparoscopic evaluation of the diaphragm should be liberally considered in patients selected for nonoperative management.
One of the major reasons for the reluctance of the surgical community to adopt a selective nonoperative approach in patients with penetrating solid organ injuries is the concern of missing other significant intra-abdominal injuries, especially hollow viscus perforations. The present study has shown that 39.6% of penetrating liver injuries, 30.4% of renal injuries, and 10.7% of splenic injuries do not have any other significant intra-abdominal injuries. Armenakas et al,24 in a review of 200 stab wounds to the kidneys, reported that in 39% of the cases, the injuries did not involve any other intra-abdominal organ. In another study from our center, 34% of 152 patients with gunshot wounds to the liver had no other significant intra-abdominal injuries.19 The early identification of patients with associated intra-abdominal injuries or significant bleeding is the cornerstone of selective nonoperative management. Careful initial and subsequent serial clinical examinations are very reliable and safe in the evaluation of both stab wounds and gunshot wounds to the abdomen.1–6,17–19,21–24 Patients who are clinically unevaluable (ie, severe head trauma, spinal cord injury, need for other extra-abdominal operations) should not be considered for nonoperative management. Alcohol or illicit drugs do not seem to adversely affect the reliability of physical examination.4–6 The addition of CT scan evaluation of the abdomen and lower chest has greatly enhanced the safe selection of patients for nonoperative management.10,26 CT scan findings diagnostic or suggestive of hollow viscus injury automatically preclude observation and avoid any delays in surgery. In a prospective study from our center, 100 patients with gunshot wounds to the abdomen who were hemodynamically stable and had no signs of peritonitis underwent CT scan evaluation of the abdomen. The sensitivity and specificity in identifying significant intra-abdominal injuries were 98.5% and 96.0%, respectively.27 Ginzburg et al,10 in a similar study with 83 patients, reported a sensitivity of 100%. The combination of a careful clinical examination and a contrast CT scan is highly sensitive in identifying or highly suspecting any hollow viscus injury.
The benefits of successful nonoperative management should be weighted against the risks of missed hollow viscus injuries and delayed treatment. In the present study, the diagnosis was delayed in 2 cases with hollow viscus injuries (in both cases, there was a violation of the protocol regarding the CT scan evaluation). Both patients recovered uneventfully. In a collective review of 5 prospective studies with 728 patients with penetrating abdominal injuries, selected for nonoperative management, the incidence of delayed diagnosis was 3.4% and there was no mortality and no increased intra-abdominal septic complications.28 It is possible that patients with hollow viscus injuries and no clinical signs of peritonitis on admission have small and walled off perforations and delay of treatment by a few hours does not result in increased morbidity.28
Routine laparotomy for all diagnosed solid organ injuries in this study would have resulted in a significant number of nontherapeutic laparotomies. The complication rate in nontherapeutic laparotomies for trauma is significant. In a collective review of 1489 nontherapeutic laparotomies, the complication rate was 14.6%.28
There are few data comparing outcomes in penetrating solid organ injuries managed operatively versus nonoperatively. In a previous study from our center, grade II gunshot injuries to the liver managed nonoperatively had fewer blood transfusions and a shorter hospital stay than similar injuries managed operatively.19 In the present study, nonoperative management of isolated liver injuries was associated with a significantly shorter hospital stay than patients treated operatively (3.0 vs. 5.5 days, P = 0.015), even though the nonoperative group included more severe injuries. As discussed above, the complication rate of an exploratory laparotomy without any therapeutic interventions is 14.6%. There were no complications in the 41 patients with 44 solid organ injuries, including 18 patients with severe (grade III-V) injuries who were treated nonoperatively. The liver-related complications in severe liver injuries managed operatively are higher than 50%. In a prospective study of 49 patients with grade III to IV liver injuries managed operatively at our center, the incidence of liver-related complications was 51%.29 In a similar study of 36 grade III or IV penetrating liver injuries treated operatively, Knudson et al30 reported liver-related complications in 52% of survivors. There is evidence that in blunt liver trauma, nonoperative management is associated with fewer abdominal complications than operative management. Croce et al16 reported fewer blood transfusions and abdominal complications in blunt liver injuries managed nonoperatively than in similar injuries managed operatively. Similar results have been reported for blunt renal injuries. Robert et al31 and Moudouni et al,32 in studies of severe blunt renal injuries, concluded that operative management was more likely to result in the loss of the injured kidney than in nonoperative management.
CONCLUSION
In the appropriate trauma center environment, selective nonoperative management of penetrating abdominal solid organ injuries, especially liver injuries, has a high success rate and a low complication rate. High-grade injuries do not preclude nonoperative management.
Discussions
Dr. David B. Hoyt (San Diego, California): The earliest description of the nonoperative management of abdominal gunshot wound that I can find was written by Ambrose Pere in 1520. The patient had an epigastric gunshot wound and passed the bullet per rectum about 5 days post-injury without complication. This study is one of many over the last 20 years showing the evolving indications for laparotomy following abdominal trauma in general.
First we learned from the pediatric surgeons using primitive ultrasound that nonoperative management of splenic and liver injuries was possible. This evolved into nonoperative management of blunt cell organ injury in adults and that is now common practice.
Selective management of penetrating injuries has been advocated before but has really not been adapted due to concerns over delayed complications of bleeding and sepsis, and Dr. Demetriades alluded to this. The current study, however, demonstrates that using CT scanning you can better select patients who don't need operation. In their hands, 25% of patients can be so selected. Again, patients that are hemodynamically stable and have no peritoneal signs.
The critical question in reviewing a manuscript to me is how good CT scan is in this situation. And this leads me to 4 questions.
First, are there minimal criteria for the CT protocol in your institution that you use in this situation that should be used by the rest of us if we incorporate this into our own practice-specifically, the number of slices? Is there a density CT scan that is minimum, thickness of slices, use of oral contrast, IV contrast, water versus ionic contrast?
Secondly, what are your CT criteria that suggest enteric or diaphragmatic injury? You didn't really specifically address that in your manuscript. You alluded to it in the presentation. But can you share with us what would you call somebody that had a suspicious enteric injury on CT? Particularly, was this a useful criteria than in predicting actual enteric injury?
Third, you showed some pictures of blushes. But can you describe the blush that would force you to operate if you do delayed scanning to detect if there is persistent extravasation? How do you do that with a CT scan since you don't have that same dynamic on an angiogram?
Finally, is there a typical trajectory that really corresponds to the kind of group of patients that you are talking about? The first indications that this was possible were really with people with tangential wounds over the liver. Have you expanded those trajectories? Or can you help us understand what the typical patient is?
Again, the group at USC has led this area not only in the abdomen but also in the neck and the chest, and I appreciate the opportunity to discuss the paper.
Dr. Demetrios Demetriades (Los Angeles, California): We use an old model CT scan. We specifically request 3 millimeter cuts and we always give intravenous contrast. We practically never use oral contrast because of the risk of aspiration and delay of the procedure.
How reliable is the CT scan? I think that the combination of CT scan and a careful initial and subsequent serial clinical examinations is extremely reliable in identifying any significant injuries. It is very rarely that you miss any hollow viscous injuries.
What are the CT scan diagnostic criteria, which are suspicious for hollow viscous injury? Number one, very often tiny amounts of free air are found somewhere. This is the most diagnostic finding. In addition to that, local thickening of the bowel wall or mesenteric stranding, are suspicious signs. But again I would repeat, it is the combination of clinical examination and the CT scan findings, not the CT scan alone.
The next question is about the management of patients with a blush on CT scan. It all depends on the clinical condition of the patient. If the patient is hemodynamically unstable, he will go to the operating room immediately. If he becomes hemodynamically unstable during the CT scan, he will go from the CT scan to the operating room. If the patient is stable he will go the angio suite for evaluation and possibly angioembolization. Most likely in our experience it is a false aneurysm. Less often it is a slow, continuous bleeding. The success rate of embolization of these conditions is excellent.
The last question was about the trajectory of the bullet. Thin CT scans provide a good picture of the missile trajectory. The ideal candidate for non-operative management is a patient with a penetrating injury over the liver or kidneys with a CT trajectory away from hollow viscera or major vessels.
Dr. Anthony A. Meyer (Chapel Hill, North Carolina): I worry a little bit about the concept of pushing this continually further. Although you describe a high incidence of the finding hollow viscous injuries on CT, all the data from blunt hollow viscous injuries detected by CT show that CT is generally a poor predictor of hollow viscous injury, and free air is often not seen. You can use some of the more vague criteria that you describe in terms of thickening, but without that, looking for using CT is notably difficult.
The other one had to do with the question of what is your complication rate with regard to delayed operations in patients who have peritonitis since it is a clinical finding and oftentimes masked by things such as drugs or other things in the preoperative patient? What do you get as your complication rate when you delay until you have peritonitis? I know you said it was about a 7-hour delay, but there is obviously spectrum. What is your complication rate in those compared to what you described historically from a 14.6% complication rate in non-therapeutic operations?
Dr. Demetrios Demetriades (Los Angeles, California): You are right, many studies have reported fairly low sensitivity and specificity of the CT scan in diagnosing hollow viscus injuries. In our center we have better results than those reported. In a recent prospective study of 100 patients with abdominal gunshot wounds from our center, the sensitivity and specificity of CT scanning in identifying significant injuries was 90.5% and 96%, respectively. But most importantly, I want to stress what I mentioned earlier about the importance of the combination of clinical examination and CT scan. You never make a decision exclusively on the basis of the CT scan findings.
Your next question was about the complication rate for delayed operations. We read quite a lot about the magic number of 4 hours or 6 hours delay, after which the complication rate goes up. I do not agree with these figures. In this series, we had no complications in the 3 or 4 patients with delayed procedures. As you may remember, a few of years ago we did a prospective American Association for the Surgery of Trauma study, which included about 300 patients with penetrating colon injuries requiring resection. In the analysis, we compared complications in patients going to the operating room within 6 hours of injury with those operated on after 6 hours. We found no difference in the complication rate in the 2 groups. The most important factor for the development of septic complications is the degree of peritoneal contamination. If you have severe fecal contamination, the patient will develop septic complications even if you operate within 20 minutes of the injury. On the other hand, if you have a small perforation of the colon with minimal and contained fecal spillage, the patient will do well, even if you operate after more than 6 hours. So, it is mainly the degree of contamination, not the delay of a few hours.
Dr. Richard J. Mullins (Portland, Oregon): My first question is, do you feel that the non-therapeutic laparotomy rate should be included in the evaluation of trauma center registry data as an indication of quality of care? In other words, if a trauma center has too many nontherapeutic laparotomies, is that an indication of inferior care?
Second, do you feel that if there is a delay in therapeutic laparotomy in one of your patients that should be presented at your morbidity and mortality conference as a complication? Even though the patient doesn't have a problem, you have delayed intervention.
And the third question, I understand that at your hospital, your level 1 trauma center dedicated to the care of a lot of patients, this is an acceptable protocol. Suppose I am practicing in a small town, I am the only surgeon on call, and I have somebody who is shot in the abdomen. Are you advocating that I follow the same protocol that you are following at USC? Or do you think that this is maybe something that is only applicable to certain centers?
Dr. Demetrios Demetriades (Los Angeles, California): Is a nontherapeutic laparotomy a complication? Absolutely, yes. In our program every non-therapeutic operation is discussed as a complication.
Is a delay of the operation discussed as a complication. Absolutely yes! It is consider as a serious complication and will be discussed at the weekly M&M meeting.
Is this approach of selective non-operative management suitable for small peripheral hospitals? No. This is not the easy way out. The easy way out is to do a laparotomy, find nothing, close the abdomen and send the patient home a couple of days later. The nonoperative management is difficult way out. You need to have surgeons in-house, you need to have capabilities of monitoring this patient all the time. At the beginning you examine the patient every 10 to 15 minutes. Later on, you need to go back hourly and then once every 2 or 3 hours. So it is a difficult way out. I wouldn't recommend it for small non-trauma centers or not well staffed centers.
Dr. Kenneth G. Swan (South Orange, New Jersey): You had in the right arm of your algorithm unstable vital signs and signs of peritonitis. And obviously that means physical findings and you said repeatedly signs of peritonitis and physical findings.
I am distressed to find amongst medical students that their physical diagnosis courses led them to believe that peritonitis doesn't exist unless you have rebound tenderness. And I think most surgeons know that that is excessive. So if so much emphasis is placed on physical findings and you have been very appropriately cautious to not give narcotics to mask the findings, what are your definitions of peritonitis on physical exam?
Dr. Demetrios Demetriades (Los Angeles, California): Peritonitis includes rigidity, guarding, rebound tenderness, and pain away from the site of the penetrating injury. Pain away from the bullet tract is a sign of peritonitis and the patient needs an operation.
Dr. Kenneth G. Swan (South Orange, New Jersey): Tenderness for peritonitis is my question. Tenderness alone will suffice?
Dr. Demetrios Demetriades (Los Angeles, California): Any tenderness away from the bullet tract is an indication for an operation.
Dr. Kenneth G. Swan (South Orange, New Jersey): Tenderness anywhere in the abdomen? The bullet tract is up here, the tenderness is down here?
Dr. Demetrios Demetriades (Los Angeles, California): Right, anywhere in the abdomen, away from the bullet tract.
Dr. John M. Howard (Toledo, Ohio): Suppose you have to do an emergency operation for some nonabdominal problem, does that alter your management of the abdominal injury?
Dr. Demetrios Demetriades (Los Angeles, California): In these cases we will not try nonoperative management. If the patient has a head injury, a spinal cord injury, or if he is undergoing another extra-abdominal operation, we will perform a laparotomy. We will not observe this patient because the benefit of clinical examination is lost.
Footnotes
Reprints: Demetrios Demetriades, MD, PhD, Trauma/SICU, LAC+USC Medical Center, 1200 North State Street, Room 1105, Los Angeles, CA 90033. E-mail: demetria@usc.edu.
REFERENCES
- 1.Demetriades D, Rabinowitz B. Indications for operation in abdominal stab wounds: a prospective study of 651 patients. Ann Surg. 1987;205:129–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Demetriades D, Rabinowitz B, Sofianos C, et al. The management of penetrating injuries of the back: a prospective study of 230 patients. Ann Surg. 1988;207:72–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Demetriades D, Charalambides D, Lakhoo M, et al. Gunshot wounds of the abdomen: role of selective nonoperative management. Br J Surg. 1991;78:220–222. [DOI] [PubMed] [Google Scholar]
- 4.Demetriades D, Velmahos G, Cornwell E, et al. Selective non-operative management of gunshot wounds of the anterior abdomen. Arch Surg. 1997;132:178–183. [DOI] [PubMed] [Google Scholar]
- 5.Velmahos G, Demetriades D, Cornwell E, et al. A selective approach to the management of gunshot wounds to the back. Am J Surg. 1997;174:342–346. [DOI] [PubMed] [Google Scholar]
- 6.Velmahos G, Demetriades D, Toutouzas K, et al. Selective non-operative management in 1856 patients with abdominal gunshot wounds: should routine laparotomy still be the standard of care? Ann Surg. 2001;234:395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chmielewski GW, Nicholas JM, Dulchavsky SA, et al. Non-operative management of gunshot wounds of the abdomen. Am Surg. 1995;61:665–668. [PubMed] [Google Scholar]
- 8.Renz BM, Feliciano DV. Gunshot wounds to the right thoracoabdomen: a prospective study of non-operative management. J Trauma. 1994;37:737–744. [DOI] [PubMed] [Google Scholar]
- 9.Sosa JL, Arrillaga A, Puente I, et al. Laparoscopy in 121 consecutive patients with abdominal gunshot wounds. J Trauma. 1995;39:504–506. [DOI] [PubMed] [Google Scholar]
- 10.Ginzburg E, Carrillo EH, Kopelman T, et al. The role of computed tomography in selective management of gunshot wounds to the abdomen and flank. J Trauma. 1998;45:1005–1009. [DOI] [PubMed] [Google Scholar]
- 11.Velmahos G, Toutouzas KG, Radin R, et al. Non-operative treatment of blunt injury to solid abdominal organs: a prospective study. Arch Surg. 2003;138:844–851. [DOI] [PubMed] [Google Scholar]
- 12.Velmahos G, Toutouzas K, Radin R, et al. High success with non-operative management of blunt hepatic trauma: the liver is a sturdy organ. Arch Surg. 2003;138:475–480. [DOI] [PubMed] [Google Scholar]
- 13.Myers JG, Dent DL, Stewart RM, et al. Blunt splenic injuries: dedicated trauma surgeons can achieve a high rate of non-operative success in patients of all ages. J Trauma. 2000;48:801–805. [DOI] [PubMed] [Google Scholar]
- 14.Santucci RA, Fisher MB. The literature increasingly supports expectant (conservative) management of renal trauma: a systematic review. J Trauma. 2005;59:493–503. [DOI] [PubMed] [Google Scholar]
- 15.Davis KA, Reed RL, Santaniello J, et al. Predictors of the need for nephrectomy after renal trauma. J Trauma. 2000;60:164–170. [DOI] [PubMed] [Google Scholar]
- 16.Croce MO, Fabian TC, Menke PG, et al. Non-operative management of blunt hepatic trauma is the treatment of choice for hemodynamically stable patients: results of a prospective trial. Ann Surg. 1995;221:744–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Demetriades D, Rabinowitz B, Sofianos C. Non-operative management of penetrating liver injuries: a prospective study. Br J Surg. 1986;73:736–737. [DOI] [PubMed] [Google Scholar]
- 18.Renz RM, Feliciano DV. Gunshot wounds to the liver: a prospective study of selective non-operative management. J Med Assoc Ga. 1995;84:275–277. [PubMed] [Google Scholar]
- 19.Demetriades D, Gomez H, Chahwan S, et al. Gunshot injuries to the liver: the role of selective non-operative management. J Am Coll Surg. 1999;188:343–348. [DOI] [PubMed] [Google Scholar]
- 20.Nance ML, Lutz N, Carr MC, et al. Blunt renal injuries in children can be managed non-operatively: outcome in a consecutive series of patients. J Urol. 2004;57:474–478. [DOI] [PubMed] [Google Scholar]
- 21.Carroll PR, McAninch JW. Operative indications in penetrating renal trauma. J Trauma. 1985;25:587–593. [DOI] [PubMed] [Google Scholar]
- 22.Heyns CF, De Klerk DP, De Kock ML. Non-operative management of renal stab wounds. J Urol. 1985;134:239–242. [DOI] [PubMed] [Google Scholar]
- 23.Wessells H, McAninch JW, Meyer A, et al. Criteria for non-operative treatment of significant penetrating renal lacerations. J Urol. 1997;157:24–27. [PubMed] [Google Scholar]
- 24.Armenakas NA, Duckett CP, McAninch JW. Indication for non-operative management of renal stab wounds. J Urol. 1994;161:768–771. [PubMed] [Google Scholar]
- 25.Velmahos G, Demetriades D, Cornwell E, et al. Selective management of renal gunshot wounds. Br J Surg. 1998;85:1121–1124. [DOI] [PubMed] [Google Scholar]
- 26.Pachter HL, Ruth AA, Holstetier SR, et al. Changing patterns in the management of splenic trauma: the impact of non-operative management. Ann Surg. 1998;227:708–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Velmahos G, Constantinos C, Tillou A, et al. Abdominal computer tomographic scan for patients with gunshot wounds to the abdomen selected for non-operative management. J Trauma. 2005;59:1155–1160. [DOI] [PubMed] [Google Scholar]
- 28.Demetriades D, Velmahos G: Indications for and techniques of laparotomy. In: Moore, Feliciano, Mattox, eds. Trauma, 6th ed. New York: McGraw-Hill, In press.
- 29.Demetriades D, Karaiskakis M, Alo K, et al. Role of postoperative computed tomography in patients with severe liver injury, Br J Surg. 2003;90:1398–1400. [DOI] [PubMed] [Google Scholar]
- 30.Knudson MM, Lim RC, Olcot EW. Morbidity and mortality following major penetrating liver injuries. Arch Surg. 1994;129:256–261. [DOI] [PubMed] [Google Scholar]
- 31.Robert M, Drianno N, Muir G, et al. Management of major blunt renal lacerations: surgical or non-operative approach? Eur Urol. 1996;30:335–339. [DOI] [PubMed] [Google Scholar]
- 32.Moudouni SM, Hadj S, Manunta A, et al. Management of major blunt renal lacerations: is a non-operative approach indicated? Eur Urol. 2001;40:409–414. [DOI] [PubMed] [Google Scholar]


