Abstract
Objective:
To examine whether delayed surgical intervention in adult patients with acute appendicitis is safe by correlating the interval from onset of symptoms to operation (total interval) with the degree of pathology and incidence of postoperative complications.
Summary Background Data:
Prompt appendectomy has long been the standard of care for acute appendicitis because of the risk of progression to advanced pathology. This time-honored practice has been recently challenged by studies in pediatric patients, which suggested that acute appendicitis can be managed in an elective manner once antibiotic therapy is initiated. No such data are available in adult patients with acute appendicitis.
Methods:
A retrospective review of 1081 patients who underwent an appendectomy for acute appendicitis between 1998 and 2004 was conducted. The following parameters were monitored and correlated: demographics, time from onset of symptoms to arrival at the emergency room (patient interval) and from arrival to the emergency room to the operating room (hospital interval), physical, computed tomography (CT scan) and pathologic findings, complications, length of stay, and length of antibiotic treatment. Pathologic state was graded 1 (G1) for acute appendicitis, 2 (G2) for gangrenous acute appendicitis, 3 (G3) for perforation or phlegmon, and 4 (G4) for a periappendicular abscess.
Results:
The risk of advanced pathology, defined as a higher pathology grade, increased with the total interval. When this interval was <12 hours, the risk of developing G1, G2, G3, and G4, was 94%, 0%, 3%, and 3%, respectively. These values changed to 60%, 7%, 27%, and 6%, respectively, when the total interval was 48 to 71 hours and to 54%, 7%, 26%, and 13% for longer than 71 hours. The odds for progressive pathology was 13 times higher for the total interval >71 hours group compared with total interval<12 hours (95% confidence interval = 4.7–37.1). Although both prolonged patient and hospital intervals were associated with advanced pathology, prehospital delays were more profoundly related to worsening pathology compared with in-hospital delays (P < 0.001). Advanced pathology was associated with tenderness to palpation beyond the right lower quadrant (P < 0.001), guarding (P < 0.001), rebound (P < 0.001), and CT scan findings of peritoneal fluid (P = 0.01), fecalith (P = 0.01), dilation of the appendix (P < 0.001), and perforation (P < 0.001). Increased length of hospital stay (P < 0.001) and antibiotic treatment (P < 0.001) as well as postoperative complications (P < 0.001) also correlated with progressive pathology.
Conclusion:
In adult patients with acute appendicitis, the risk of developing advanced pathology and postoperative complications increases with time; therefore, delayed appendectomy is unsafe. As delays in seeking medical help are difficult to control, prompt appendectomy is mandatory. Because these conclusions are derived from retrospective data, a prospective study is required to confirm their validity.
The common practice of early appendectomy for acute appendicitis was recently challenged in children. The present study found that in adult patients the degree of pathology and incidence of complications are time-dependent; therefore, delayed management is unsafe.
Acute appendicitis is the most common surgical emergency in the United States.1 Although the exact mechanisms leading to this condition are still obscure, it is likely that luminal obstruction by external (lymphoid hyperplasia) or internal (inspissated fecal material, appendicoliths) compression plays a key pathogenic role. The luminal obstruction leads to increased mucus production, bacterial overgrowth, and stasis, which increase appendiceal wall tension. Consequently, blood and lymph flow is diminished, and necrosis and perforation follow. As these events occur over time, it is conceivable that early surgical intervention prevents progression of disease. Indeed, this notion provided the basis for the historical concept of immediate operation for patients with acute appendicitis. Nevertheless, a review of the literature indicates that the common practice of early appendectomy is supported by limited data. Furthermore, recent reports in pediatric patients suggest that postponing surgery with fluid and antibiotic treatment can be safely pursued.2–4
The present study was designed to evaluate whether acute appendicitis in adult patients is indeed a surgical emergency requiring immediate intervention or a disease that can be approached in a semi-elective manner. To that end, the relationships between duration of symptoms, timing of surgery, degree of pathology, and complications were determined in all adult patients who underwent an appendectomy for acute appendicitis during a 6-year period in a tertiary care urban hospital.
PATIENTS AND METHODS
Patients
A retrospective analysis was performed on 1287 adult patients (≥16 years of age) who underwent an appendectomy for acute appendicitis at Yale New Haven Hospital between February 1998 and December 2004. Patients found to have a normal appendix (96, 7.5%), whose pathologic analysis differed from the intraoperative assessment (14, 1.9%), or without a documented time of onset of symptoms (96, 7.5%) were excluded. Preoperative data extracted from the patients’ charts included: gender, age, physical and computed tomography (CT scan) findings, time from onset of symptoms to the emergency room (patient interval), and time from emergency department admission to the operating suite (hospital interval). Interval from onset of symptoms to surgery (total interval) was calculated by adding the patient and hospital intervals. Operative and pathologic findings were graded G1 for acute appendicitis, G2 for gangrenous appendicitis, G3 for perforated appendicitis or a phlegmon, and G4 for a periappendicular abscess. Postoperative data retrieved included length of hospital stay and of antibiotic treatment, complications, and mortality.
Statistical Analysis
Data were maintained on an Excel (Microsoft) spreadsheet and analyzed using the Mantel-Haenszel χ2 test for trend, ordinal logistic regression, and linear regression where appropriate, as specified below.
The ordinal logistic regression is a proportional odds model that determines the cumulative odds of a less favorable response compared with a more favorable response.5 In this model, 3 log odds ratios (G4 vs. others; G4 or G3 vs. others; and grade G4, 3, 2 vs. 1) were defined and assumed to be parallel (ie, the effects of the risk factors were the same for the different log odds, but the intercepts are different). The resulting odds ratios may be interpreted as the relative likelihood for worsening pathology in the presence compared with the absence of a given risk factor. Separate multivariable models were evaluated for physical examination (PE) and CT findings using an automated backward selection procedure with a 0.05 significance level to stay in the model.
RESULTS
Demographics
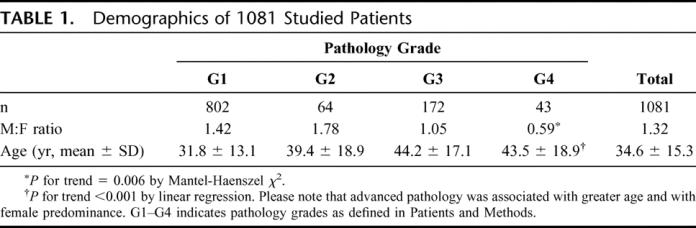
Most patients were males in their 30s (Table 1). Advanced pathology was associated with the female gender (P = 0.006) and increase in age (P < 0.001).
TABLE 1. Demographics of 1081 Studied Patients
Relationship Between Timing of Surgery and Degree of Pathology
The prevalence of advanced pathology, defined as a higher pathology grade, positively correlated with prolonged total interval (P for trend, <0.001, Fig. 1A). Odds ratios comparing the likelihood of advancing pathology between increasing total intervals were estimated using an ordinal logistic regression (Fig. 1B). The reference category for these odds ratios is a total interval <12 hours. The odds of advancing pathology were greater in prolonged total intervals compared with the reference category (P for trend, <0.001). For example, the risk for progressive pathology increased 13-fold when the total interval was greater than 71 hours. Patient (Fig. 2A) and hospital (Fig. 2B) intervals, the components of total interval, also increased with advanced pathology (P for trend, <0.01). However, there was a positive relationship of increasing patient to hospital interval ratio with pathology grade (P for trend, >0.001, Fig. 2C).
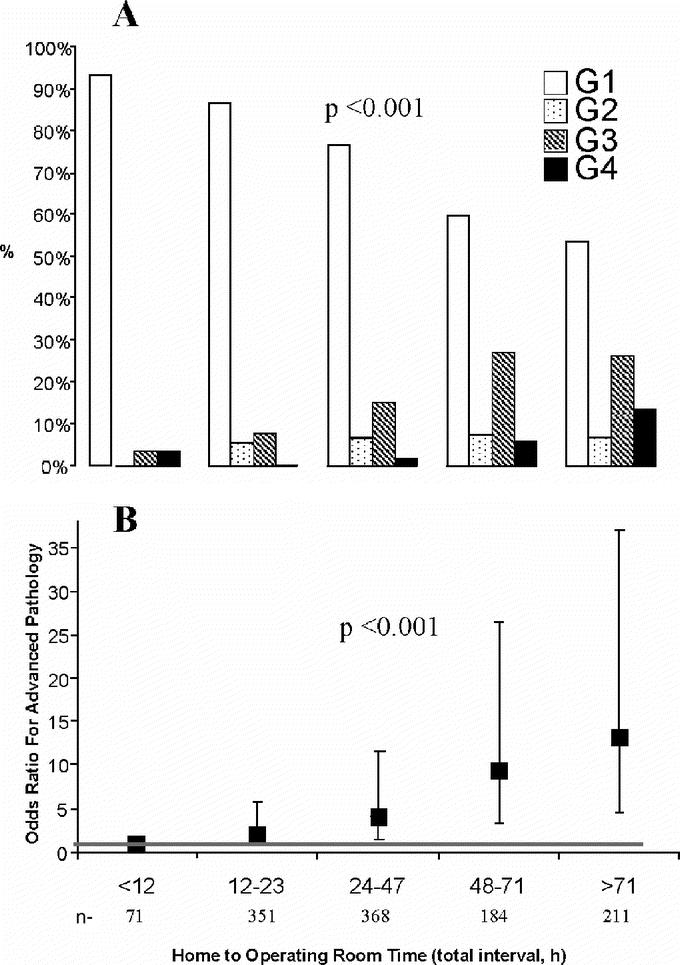
FIGURE 1. Relationship between advanced pathology and interval from onset of symptoms to surgery (total interval). A, Distribution of pathology grades per total intervals. B, Total interval and pathology grade proportions were compared using Mantel-Haenszel χ2 test for trend. Odds ratios (OR) compare the likelihood of advanced pathology for a given total interval to those with a total interval less than 12 hours. Bars represent 95% confidence intervals (CI) and the dashed line indicates OR = 1 (ie, if 1 is contained within the 95% CI, then the odds for advanced pathology for this total interval are not significantly different than the odds for the <12 hours group). G1–G4, pathology grades as defined in Patients and Methods.
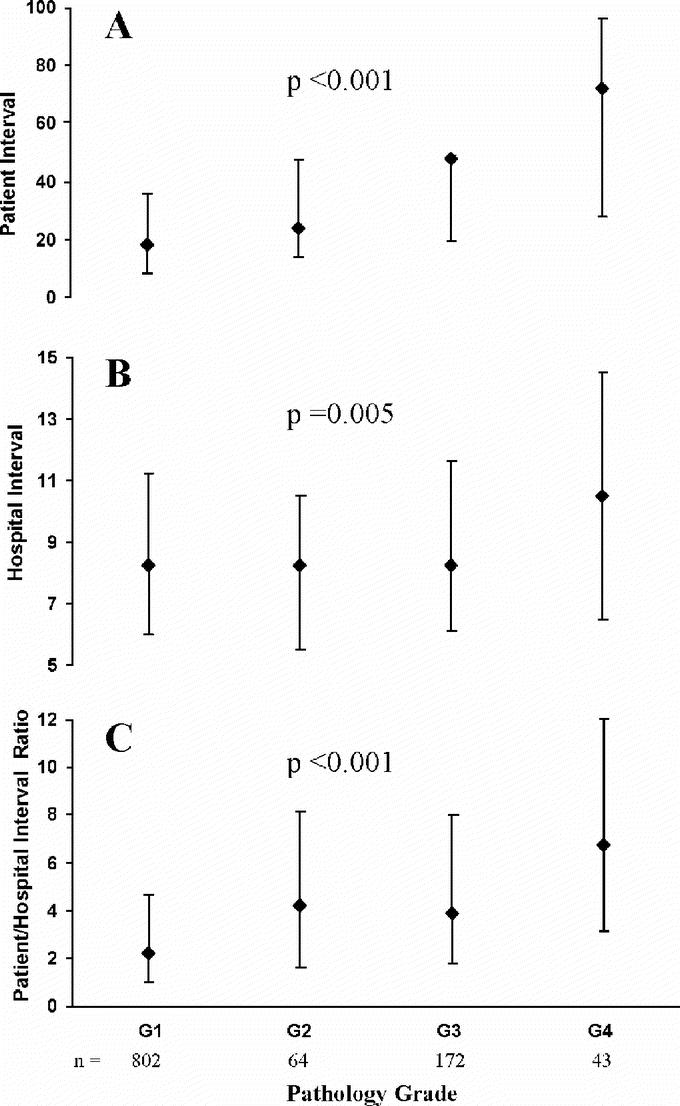
FIGURE 2. Relationship between patient to hospital interval ratio and degree of pathology. A, Relationship between patient interval and pathology grade. B, Relationship between hospital interval and pathology grade. C, Relationship between patient and hospital interval ratio and degree of pathology. Please note that increased patient and hospital intervals as well as patient and hospital interval ratio were associated with advanced pathology (P for trend from linear regression <0.01). This indicates that patient delay more significantly contributes to progressive pathology. Data are expressed as medians with bars representing 25th and 75th percentile. G1–G4, pathology grades as defined in Patients and Methods.
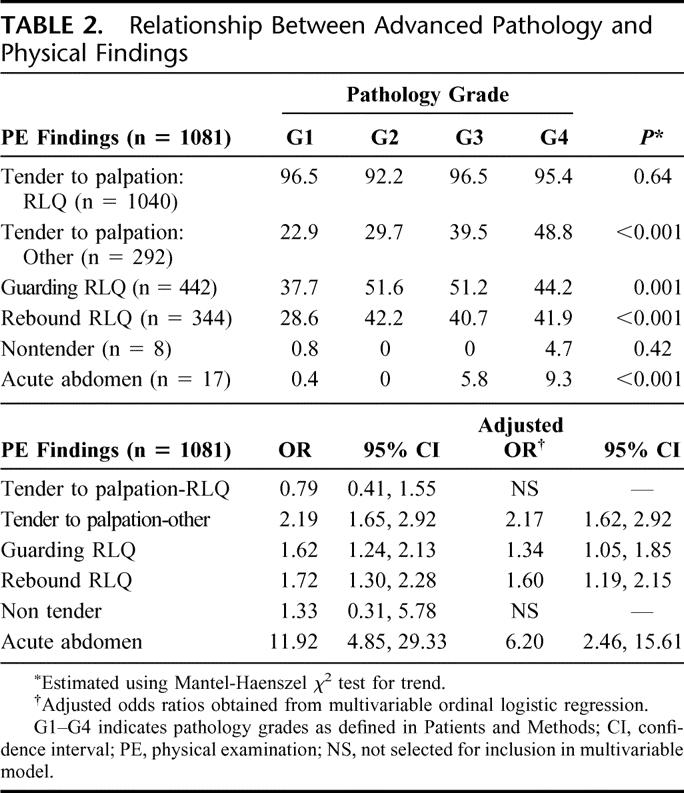
Relationship Between Severity of Pathology and Physical Findings
The incidence of tenderness to palpation outside of the right lower quadrant (RLQ), RLQ rebound and guarding, and acute abdomen were associated with advanced pathology (P ≤ 0.001) (Table 2). Similarly, as shown by the odds ratios, the risk of advanced pathology was increased for each of these findings (Table 2). For example, when tenderness outside of the RLQ was present, the likelihood of progressive pathology was increased by 2-fold. The association between these findings and advanced pathology remained significant in the multivariable model (Table 2).
TABLE 2. Relationship Between Advanced Pathology and Physical Findings
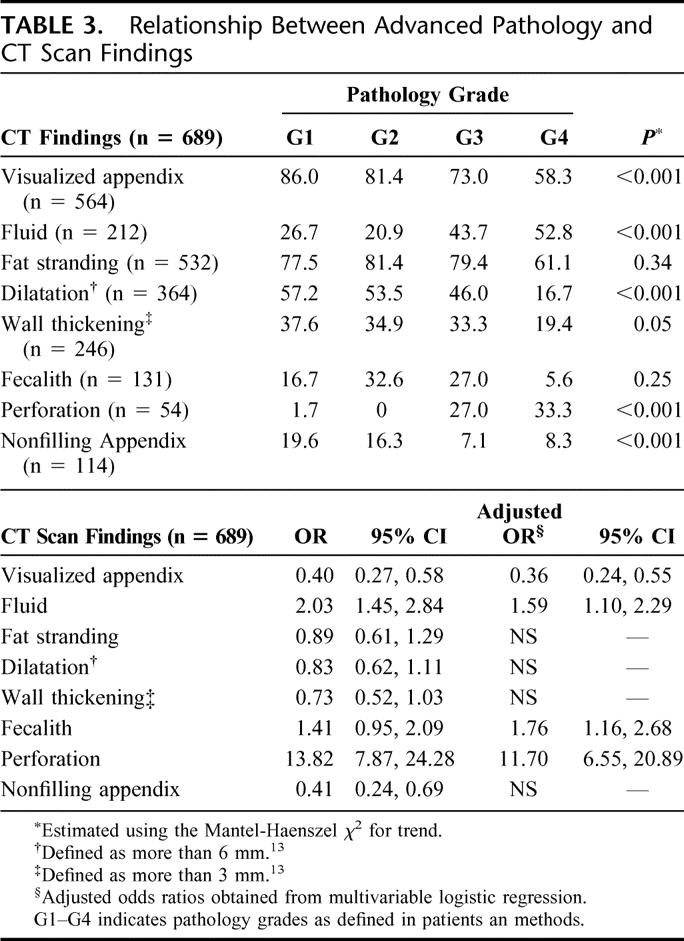
Relationship Between Severity of Pathology and CT Scan Findings
The presence of peritoneal fluid and perforation increased with advanced pathology (P < 0.001) while visualized appendix was inversely related to severity of disease (P < 0.001) (Table 3). The odd ratios for advanced pathology correlated with these CT scan findings and remained significant in the multivariable analysis. In unadjusted analysis, dilatation, wall thickening, and nonfilling of the appendix were inversely related with worsening pathology (Table 3). However, in the multivariable model, these CT scan findings were not significantly associated with pathology grade (Table 3). Furthermore, the presence of a fecalith was not related to advanced pathology (Table 3), although after adjustment for the other CT scan findings, a positive correlation emerged between the presence of fecalith and advancing pathology (Table 3).
TABLE 3. Relationship Between Advanced Pathology and CT Scan Findings
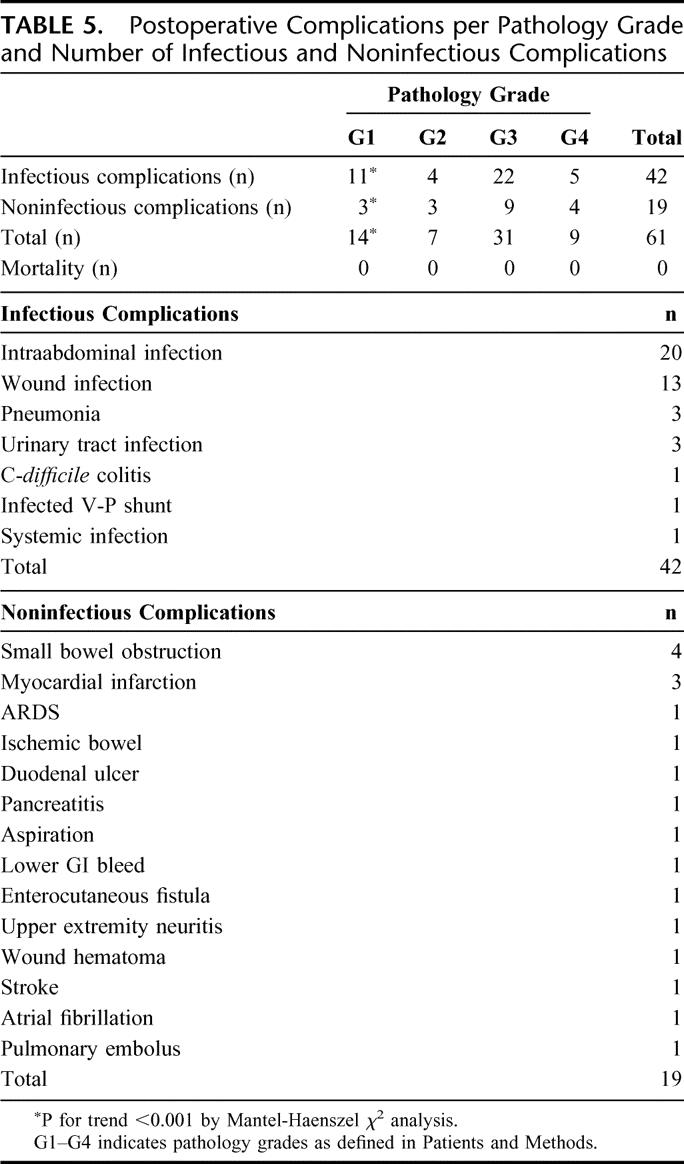
Relationship Between Severity of Pathology and Clinical Course
Length of hospital stay and antibiotic treatment (Table 4) as well as postoperative complications (Table 5) increased with advanced pathology. No mortality was recorded (Table 5).
TABLE 4. Length of Hospital Stay and Antibiotic Treatment per Pathology Grade
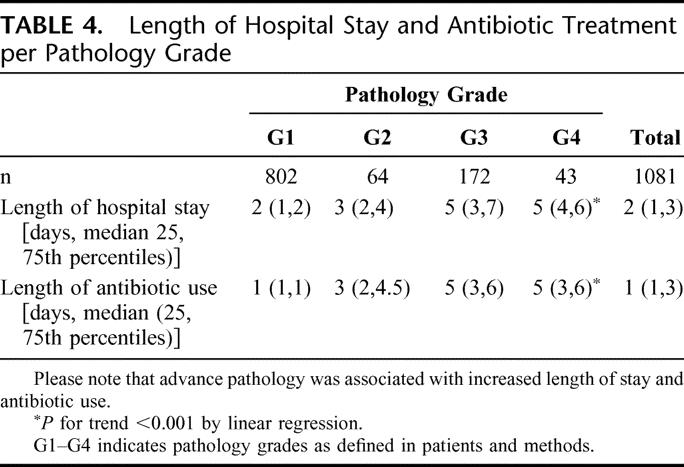
TABLE 5. Postoperative Complications per Pathology Grade and Number of Infectious and Noninfectious Complications
DISCUSSION
The present study demonstrates that the severity of pathology and complication rate in adult patients with acute appendicitis are time dependent, and therefore suggests that delaying appendectomy is unsafe. This observation contrasts with reports in pediatric patients whose appendectomy was postponed overnight without an increase in perforation rate, morbidity, and duration of hospitalization.2–4 The reasons for these diverse observations remain speculative. Potential explanations include differences in the immune status and etiologies of acute appendicitis in adult compared with pediatric patients.
The core finding in support of the observation that pathology grade and symptom duration correlate positively is the quantification of the relationship between these 2 parameters. The use of a new pathology grading system, which unlike previous studies includes the entire spectrum of acute appendicitis, and the exact time recording of events, allowed the calculation of the additional risk for advanced pathology per time interval. For example, when the total interval was less than 12 hours, the risk of developing G1, G2, G3, and G4, was 94%, 0%, 3%, and 3%, respectively. These values changed to 60%, 7%, 27%, and 6% when the total interval was 48 to 71 hours and to 54%, 7%, 26%, and 13% for longer than 71 hours. The odds for progressive pathology was 13 times higher when the total interval exceeded 71 hours compared with a total interval below 12 hours.
The data presented herein suggest that both patient and hospital factors affect the severity of acute appendicitis at the time of operation. However, the positive relationship of increasing patient to hospital interval ratio with pathology grade (Fig. 2C) indicates that patient delay in presenting to the emergency room was more profoundly related to worsening pathology compared with in-hospital delays. A similar observation was previously reported in 2 series,6,7 which included a much smaller number of patients (114 and 95, respectively). As the ability to minimize patient delay is limited, it is imperative that every effort is made by the hospital and physicians to expedite the evaluation and operation of patients with acute appendicitis. It should be noted that a previous study in 486 patients aged 5 to 85 years with acute appendicitis demonstrated that only patient but not hospital delay adversely affects the severity of disease.8 The lack of correlation between hospital factors and pathology grade in the latter study can be related to the inclusion of pediatric patients, who can be safely managed in a delayed fashion.2–4
Although the physical findings of acute appendicitis are well established,9 it is still unknown which ones predict advanced pathology. Analysis of the present data indicates that tenderness to palpation outside the right lower quadrant, right lower quadrant rebound and guarding, and acute abdomen correlate with advanced pathology as well as an increased risk for advanced pathology. Although intuitive, this observation has not been established previously in the literature.
Abdominal CT scan has become the main diagnostic tool for patients with acute appendicitis with a high sensitivity and specificity.10 Scanning of patients with suspected acute appendicitis has been shown to shorten the admission to operating theater interval, reduce overall admission cost, and reduce the number of nontherapeutic appendectomies.10 The present study demonstrates that the presence of peritoneal fluid, perforation, and fecalith were associated with advancing pathology in the multivariate analysis. This supports an earlier report, which demonstrated correlation between the appendix diameter, dependent fluid, appendolithiasis, and extraluminal air with histologic diagnosis.11 In contrast, another previous study failed to associate CT scan finding including visualization of the appendix, free fluid, blurred pericecal fat, mesenteric fat stranding, and free air with final pathology results.12
CONCLUSION
The present study confirms the time dependency of pathology grade and complication rate on symptom duration in adult patients with acute appendicitis. Furthermore, it quantifies the relationships between these endpoints and identifies physical and CT scan findings, which can predict progressive pathology. Taken together, these findings suggest that appendectomy should be performed as expeditiously as possible once the diagnosis of acute appendicitis is established in adult patients. This information could impact hospital resource utilization and quality of life of the entire operating room team. It should be noted that the retrospective nature of the study does not allow definitive conclusions, which can be obtained in a prospective fashion only.
Footnotes
Reprints: Reuven Rabinovici, MD, FACS, Section of Trauma, Surgical Critical Care, and Surgical Emergencies, Yale University School of Medicine, 330 Cedar Street (BB-310), New Haven, CT 06520. E-mail: reuven.rabinovici@yale.edu.
REFERENCES
- 1.Owings MF, Kozak LJ. Ambulatory and in-patient procedures in the United States, 1996. In: Vital and Health Statistics, Series 13, No. 139 [DHHS publication no. (PHS) 99-1710.] Hyattsville, MD: National Center for Health Statistics, 1998:26. [PubMed] [Google Scholar]
- 2.Yardeni D, Hirschl RB. Delayed versus immediate surgery in acute appendicitis: do we need to operate in the middle of the night? J Pediatr Surg. 2004;39:464–469. [DOI] [PubMed] [Google Scholar]
- 3.Surana R, Quinn F, Puri P. Is it necessary to perform appendectomy in the middle of the night in children? Br Med J. 1993;306:1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bachoo P, Mahomed AA, Ninan GK, et al. Acute appendicitis: the continuing role for active observation. Pediatr Surg Int. 2001;17:125–138. [DOI] [PubMed] [Google Scholar]
- 5.Hosmer DW, Lemeshow S. Applied Logistic Regression, 2nd ed. New York: John Wiley and Sons, 2000:288–308. [Google Scholar]
- 6.Maroju NK, Robinson Smile S, Sistla SC, et al. Delay in surgery for acute appendicitis. Aust NZ J Surg. 2004;74:773–776. [DOI] [PubMed] [Google Scholar]
- 7.Temple CL, Huchcroft SA, Temple WJ. The natural history of appendicitis in adults. Ann Surg. 1995;221:278–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eldar S, Nash E, Sabo E, et al. Delay of surgery in acute appendicitis. Am J Surg. 1997;173:194–198. [DOI] [PubMed] [Google Scholar]
- 9.Wagner JM, McKinney P, Carpenter JL. Does this patient have appendicitis? JAMA. 1996;276:1589–1594. [PubMed] [Google Scholar]
- 10.Rao PM, Rhea JT, Novelline RA, et al. Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med. 1998;338:141–146. [DOI] [PubMed] [Google Scholar]
- 11.Hansen AJ, Scott YW, De Petris G, et al. Histologic severity of appendicitis can be predicted by computed tomography. Arch Surg. 2004;139:1304–1308. [DOI] [PubMed] [Google Scholar]
- 12.Weyant MJ, Eachempati SR, Maluccio MA, et al. Interpretation of computed tomography does not correlate with laboratory or pathologic findings in surgically confirmed acute appendicitis. Surgery. 2000;128:145–152. [DOI] [PubMed] [Google Scholar]
- 13.Choi D, Park H, Lee YR, et al. The most useful findings for diagnosing acute appendicitis on contrast-enhanced helical CT. Acta Radiol. 2003;44:574–582. [DOI] [PubMed] [Google Scholar]


