Abstract
Background:
Recent explosions of suicide bombers introduced new and unique profiles of injury. Explosives frequently included small metal parts, increasing severity of injuries, challenging both physicians and healthcare systems. Timely detonation in crowded and confined spaces further increased explosion effect.
Methods:
Israel National Trauma Registry data on hospitalized terror casualties between October 1, 2000 and December 31, 2004 were analyzed.
Results:
A total of 1155 patients injured by explosion were studied. Nearly 30% suffered severe to critical injuries (ISS ≥ 16); severe injuries (AIS ≥ 3) were more prevalent than in other trauma. Triage has changed as metal parts contained in bombs penetrate the human body with great force and may result in tiny entry wounds easily concealed by hair, clothes etc. A total of 36.6% had a computed tomography (CT), 26.8% had ultrasound scanning, and 53.2% had an x-ray in the emergency department. From the emergency department, 28.3% went directly to the operating room, 10.1% to the intensive care unit, and 58.4% directly to the ward. Injuries were mostly internal, open wounds, and burns, with an excess of injuries to nerves and to blood vessels compared with other trauma mechanisms. A high rate of surgical procedures was recorded, including thoracotomies, laparotomies, craniotomies, and vascular surgery. In certain cases, there were simultaneous multiple injuries that required competing forms of treatment, such as burns and blast lung.
Conclusions:
Bombs containing metal fragments detonated by suicide bombers in crowded locations change patterns and severity of injury in a civil population. Specific injuries will require tailored approaches, an open mind, and close collaboration and cooperation between trauma surgeons to share experience, opinions, and ideas. Findings presented have implications for triage, diagnosis, treatment, hospital organization, and the definition of surge capacity.
Suicide bombers schedule detonation in crowded and confined spaces creating injuries from small metal fragments besides blast. Israel National Trauma Registry data (October 1, 2000 to December 31, 2004) produced 1155 such casualties. Entry wounds were easily concealed by hair and clothes, affecting triage. A total of 36.6% had a computed tomography (CT), 26.8% ultrasound scanning in the emergency department, and 532% had an x-ray. A high rate of surgical procedures was recorded, including thoracotomies, laparotomies, craniotomies, and vascular surgery. Injuries were mostly internal, open wounds, and burns, with an excess of injuries to nerves and to blood vessels. Severe injuries (AIS ≥ 3) were more prevalent in explosion victims than in patients with other trauma. In certain cases, there were simultaneous multiple injuries that required competing forms of treatment, such as burns and blast lung. Findings have implications for triage, diagnosis, treatment, and hospital organization.
A recent review on blast injuries1 outlined the mechanisms of blast injuries and provided guidelines for initial management on the basis of experience. While the article mentioned that current explosive devices used in Iraq and Israel are particularly challenging in that they are often loaded with metallic objects to inflict penetrating injuries in crowded civilian settings, the characteristics and care for such injuries are not described in the review. Such injuries have unique characteristics, scarcely mentioned in the literature and are thus not yet recognized by the wide medical community. In this paper, we use data from Israel's National Trauma Registry to provide a detailed perspective on this injury mechanism.
Injury initiated by terrorist bombings has been described in the literature spanning back for at least 20 years. These reports describe in detail the physical factors that are responsible for injury following an explosion,2 the resulting injuries and the deemed appropriate medical care.3–6 However, recent bomb explosion events in Israel vary from previous blasts: First, a new bomb composition that contains nails, bolts, small metal balls, and other components, often referred to as shrapnel, was detonated in crowded and confined spaces, and second, there was frequent use of suicide bombers to detonate these bombs. These explosions result in a combination of penetrating, blast, blunt and burn injuries.4,7
This manuscript describes in detail, suicide-bomber explosion injuries, to increase familiarity with their unique characteristics and management.
METHODS
Data recorded in the Israeli National Trauma Registry between October 1, 2000 and December 31, 2004 were analyzed. Israel National Trauma Registry records trauma hospitalizations, inpatient deaths, and transfers from other hospitals at all level I trauma centers in the country (6 in total) and at 4 regional trauma centers. Data recorded include demographic information, injury diagnosis detail, severity indicators, treatments provided, hospital services utilization, and patient disposition. Data are recorded by medical registrars at each hospital into a designated computer system and transferred periodically to the Israel National Centre for Trauma and Emergency Medicine Research at the Gertner Institute for quality assurance and statistical analysis. This system is identical at all hospitals and has been in place since 1997.
Terror casualties were identified among Israeli residents, who were hospitalized following an injury that received an ICD-9-CM external cause of injury code in the range E990–E998.
SAS statistical software was used for data summary and analysis. Statistical tests included χ2 tests for categorical data, t tests for continuous data, and Wilcoxon sum of ranks test for continuous data that did not distribute normally. A P value <0.05 was considered to be statistically significant.
RESULTS
A total of 1997 patients were hospitalized due to injuries inflicted by terrorist acts at the 10 hospitals that took part in the Israel National Trauma Registry between October 1, 2000 and December 31, 2004. The majority of terror casualties, 1155 (57.8%), were injured by suicide bomber explosion. These patients are at the focus of this paper. Other terror mechanisms (n = 842) include gunshot wounds, stabbings, injuries caused by stone throwing, deliberate running over by vehicles and more, were not included in this paper. Non–terror-related trauma hospitalizations during the same period (n = 93,498) were used for comparison of several parameters.
Triage and Management at the Emergency Department
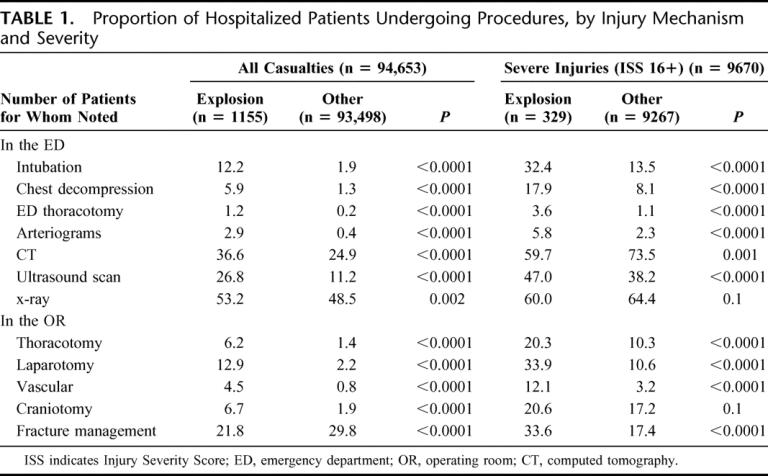
The use of diagnostic imaging in suicide bomber explosion victims was significantly more prevalent. The proportion of patients having a computed tomography (CT) in the emergency department was 36.6% in suicide bomber explosion patients versus 24.9% in other trauma. Significantly more patients (26.8% vs. 11.2%) had ultrasound scanning in the emergency department. X-rays were more common among suicide bomber explosion patients (53.2%) compared with 48.5% in nonterror injury mechanisms. Beyond diagnostic imaging, treatments in the ED provided further indication for the need for immediate life saving care. Table 1 details this information. Blood or blood products were given to 5.4% of suicide bomber explosion patients compared with 1.4% in other trauma. Chest decompression was conducted in 5.9% versus 1.3% in other trauma. Intubations at the ED were performed on 12.2% compared with 1.9% in other trauma. An ED thoracotomy was performed in 1.2% of suicide bomber explosion victims compared with 0.2% of other trauma. These results in comparison to severe or critically injured (Injury Severity Score, ISS above 16) patients are detailed in Table 1.
TABLE 1. Proportion of Hospitalized Patients Undergoing Procedures, by Injury Mechanism and Severity
Patient and Injury Characteristics
Table 2 describes distribution of patient and injury characteristics of suicide bomber explosion victims in comparison to other (nonterror) trauma; 29.3% of hospitalized suicide bomber explosion casualties suffered severe to critical (ISS ≥ 16) injuries. These proportions are significantly higher than in nonterror explosion-related trauma types (10.1%). Systolic blood pressure lower than 90 mm Hg was present in 6.1% of suicide bomber explosion victims compared with 2.6% of other trauma and a low level of consciousness, as measured by the Glasgow Coma Scale of 3 (in ED) was noted in 8.7.8% of suicide bomber explosion patients and 2.4% of other trauma patients. The proportion of patients with injuries to multiple body regions was higher among suicide bomber explosion victims.
TABLE 2. Injury Characteristics of Terror Explosion Victims Versus Other Mechanisms
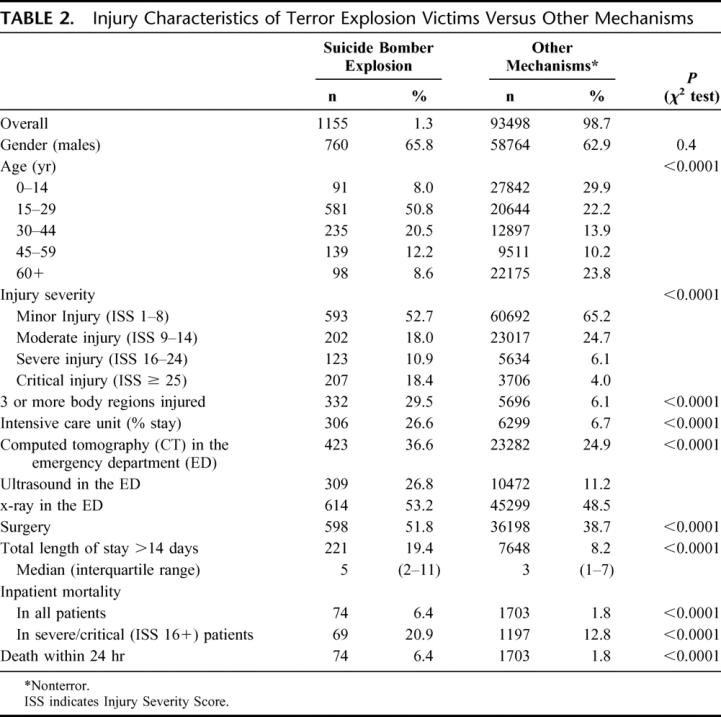
Suicide bomber explosion casualties suffered proportionately more internal injuries (32% vs. 23%), open wounds (59% vs. 17%), burns (17% vs. 5%), and most noteworthy, an excess of injuries to nerves and to blood vessels (8% vs. 1% and 4% vs. 1%, respectively) when compared with injuries from other, nonterror trauma mechanisms. The body regions injured, indicating injuries with a larger than 3 AIS severity score, are described in Figure 1. Initially, the figure showed higher percents of severe (AIS 3+) injuries in suicide bomber explosion victims among all body regions except for the extremities. Further analysis revealed that a large proportion in the “other” group were isolated hip fractures in the elderly. Once these were excluded, the pattern persisted in extremity injuries as well (Fig. 1). Nearly 18% of the patients suffered traumatic brain injuries, more than 80% of them with another injury, in another body region. In certain cases, there were simultaneous multiple injuries that required competing forms of treatment, such as burns and blast lung. Burns were present in 16.6% of suicide bomber explosion casualties, in 70.5% of them, another penetrating or blunt injury existed. The overall crude in-hospital mortality rate of suicide bomber casualties is more than 3 times higher than that of non–terror-related trauma (Table 2). The mortality rate in severely injured (ISS 16+) patients remains higher in suicide explosion casualties (21.7% vs. 13.0%).
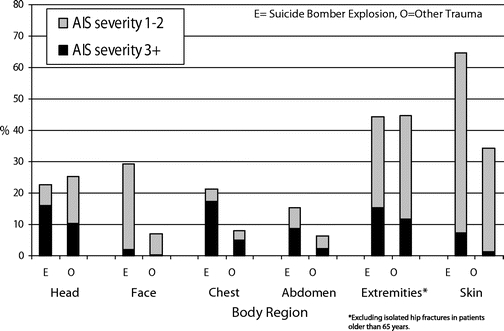
FIGURE 1. Distribution of body region injured by injury mechanism and severity.
Patient Care and Service Utilization
The frequency of surgical procedures conducted in the operating theater, such as thoracotomies, laparotomies, craniotomies, and fracture management, is detailed in Table 1, with comparisons between suicide bomber explosion victims and other trauma, in all patients and in severely/critically injured patients only. Apart from fracture management, all other surgical procedures were more frequent among suicide bomber explosion patients. Most significant is the difference in vascular surgery and laparotomies.
Intensive care was required more commonly by suicide bomber explosion victims (26.6%) compared with other trauma mechanisms (6.7%).
After the emergency department, 28.3% of suicide bomber explosion patients, compared with only 6.1% in non–terror-related trauma went directly to the operating theater, 10.1% percent in suicide bomber explosion casualties, and 4.2% in other mechanisms had gone directly to the intensive care unit and only 58.4% went directly to the ward (compared with 88.4% in non–terror-related trauma). Significantly more patients were eventually hospitalized in general surgical wards and in the intensive care unit and less in pediatric and orthopedic wards.
DISCUSSION
Recent years brought about a rise in terrorist activities worldwide. The potential use of weapons of mass destruction by terrorists poses a threat to the security of civilians everywhere. Prevention of such events, if at all possible, is beyond the role of the healthcare system; thus, our responsibility is preparedness to response. Among the variety of challenges posed by an array of potential threats, this papers’ main focus is on injuries from enhanced conventional explosives detonated by suicide bombers, creating new injury profiles.
Because of timely detonation, suicide bomber explosions usually result in mass casualty events. The proximity of recent explosions, which often occurred at city centers, near the hospital, results in short evacuation times and in patients arriving to hospitals within minutes from blast whereas they may have died if the explosion was further from the hospital and the evacuation of longer duration. This quick arrival affects the incoming case-mix and the severity of injury of the patient cohort.
Recent suicide bomber explosion casualties suffered unique injury patterns. Fragments, nails, and bolts contained in bombs fly with great force, and their penetration of the human body may result in tiny penetrating wounds (Fig. 2) that could be hidden by hair, clothes etc. The patient may walk in, apparently well, yet at the same time, the penetrating object may threaten the patient's life (Fig. 3). Thorough scanning and diagnostic imaging are necessary to identify concealed entry wounds and internal injuries due to metal pieces. In 1988, Frykberg and Tepas8 wrote that the successful management of bomb explosion trauma requires an understanding of its natural history and epidemiology. Frykberg and Tepas reviewed published experience with terrorist bombings and provided a critical analysis of these data for that cause. A more recent review5,6 studied published evidence on explosion injuries from 1966 to 2002 based on data spanning up to 1999. The latest review, published in March 2005,1 still did not present current bombs that include metal fragments in them.

FIGURE 2. Multiple minor shrapnel wounds.
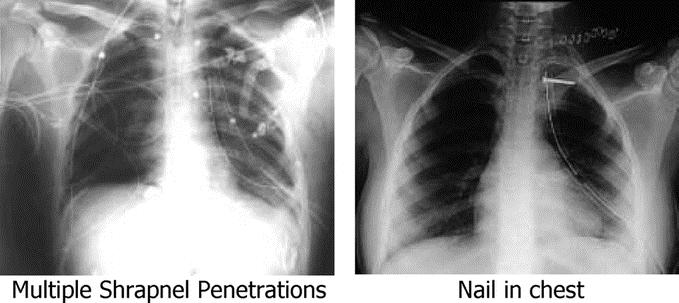
FIGURE 3. Suicide bomber explosion injuries.
This paper focused on suicide bomber explosions in Israel in the past 50 months, as such explosions created new and different injury mechanisms as a result of the contents, location, and timing of the bombs used, presenting the trauma system with new demands for preparedness and approaches to medical care.
Terror injuries have been shown to have unique epidemiology (unique distributions of age, gender, mechanism, injury types and more),4,7,9 but before all, a different pattern of arrival. Based on a study conducted by Magen David Adom (MDA, Israel's Emergency Medical Services), there was an average of 45 casualties per event.10 Although MDA evacuated the casualties from each event to several hospitals to distribute the load, thus decreasing the number of casualties per hospital, the burden usually falls on the hospitals nearest to the mass casualty incident.11 This finding is consistent with studies following the Oklahoma City bombing.12 The proportion of patients intubated in the ED in the explosion population was 6 times higher than in other trauma. This value is somewhat augmented by the fact that explosions are mass casualty incidents; thus, evacuation teams are less likely to intubate at the scene, leaving more patients to be intubated in the ED. The proportion of ED thoracotomies was also high; again, this is affected by the situation in the operating rooms as well as the fact that many of these injuries are penetrating. If we compare the number of ED thoracotomies carried out in penetrating injury patients only, the gap will decrease.
Ultrasound was used for detection of free peritoneal or pericardial fluid to identify the source of hemodynamic compromise, or as a screening test for peritoneal or pericardial penetration. The limitations of ultrasound in penetrating injuries were well appreciated, but in the setup of mass casualty event its mobility, reproducibility, and its immediate results made this modality a valuable and effective tool.
A high rate of immediate surgery and a high rate of intensive care were recorded in this study. These have important effects on the hospital. Operating rooms and intensive care units are expensive resources that function at high utilization rates. The need to clear them out from nonemergent cases and have them available to accept a sudden load of immediate cases warrants protocols to be prepared beforehand to minimize harm to patients that are already in the system and to optimize care for emergent patients when such an event occurs.
Terror casualties suffer more multiple injuries, they had a higher percent in most body region groups, as demonstrated in Figure 1. Additionally, the proportion of severe injuries within each body region is higher among terror patients. Burns were present in 16.6% of suicide bomber explosion casualties, in 70.5% of them, another penetrating or blunt injury existed. Patients with burns and blast lung present a clinical dilemma on how to treat: Burns require liberal fluid administration while blast lung requires fluid restriction. The combination of burn and blast lung will need sophisticated invasive monitoring for fluid management.
Suicide bombers are not a new phenomenon. More than 20 years ago, in 1983, a suicide bomber destroyed the building accommodating the U.S. Marines peacekeeping force in Beirut13; and ever since, this method has been used widely by many terrorist organizations. The trend of suicide bombers is on the rise, in the 1980s, they appeared mostly in Lebanon, Kuwait, and Sri Lanka, while since the year 2000, suicide bombers have attacked in India, Pakistan, Chechnya, Yemen, Algeria, Turkey, Afghanistan, Iraq, England, Spain, and more. While the ability to choose the time and place of the explosion is likely to contribute to the effectiveness of the explosion, it is not the only major factor affecting differences from previous known terror attacks. The addition of metal fragments to the explosives together with the ability to choose confined crowded locations is what makes these attacks so devastating.14,15 The explosion-related penetrating injuries are damaging multiple body regions simultaneously by fragments9,16 in addition to other effects of explosions, such as burns from the flash and hot gasses, and blast, which is described as a sudden change in environmental pressure. This pressure changes might inflict damage by passing through different body regions (especially ear drums, lungs, and bowel), displacement by mass movement of air and impact against rigid objects and causing injuries from flying objects.2,8 One major change of concept that took place following the introduction of this new injury pattern is in the frequent use of imaging in the triage process.14–17 In 1 case,14 the penetrating wound was inside the mouth, completely invisible, and the nail nested in a 14-year-old girls’ brain. As a result, seemingly stable bombing casualties are always reassessed for concealed injuries. This could be done by a CT scan or a total body plain radiographs. This shift in triage process implied heavy loads on hospital imaging resources, resulting in the need to plan well the sequence of procedures a patient goes through.
Braverman et al18 report on yet another injurious element as a result of the explosion: the penetration of bone fragments from the human suicide bomber. In this report, the perpetrator had hepatitis B and the bone fragments were positive for HbsAG, resulting in the need to immunize active immunization against hepatitis B for all injured patients in such attacks. These different consequences raised the need for reviewing protocols for hospital preparedness. Furthermore, since injuries were different from those encountered previously, the pattern of demand for resources, and the medical proficiency necessary for treating terror victims were different from before.4,9 Kluger15 sets the term “multidimensional injury” for suicide bomber explosion casualties and says that damage control surgery is the logical concept governing the treatment of these patients.
The most severe and fatal injuries occur in closed and confined areas such as busses,10,15 but even in open environment, injuries from suicide bomber explosion were more severe than other trauma types and affects a mass of people. These results are also higher in severity than reported in incidents from past periods of increase in terror activity. Lynn et al describe terror events in Israel between 1994 and 1997 and report 10% severe injuries19; this study found much higher percents, largely attributed to the new mechanisms involved, namely, suicide bombers, crowded locations, and metal pieces included with explosives.
Differences in the nature of injury between suicide bomber explosion casualties and patients with other trauma, affect the distribution of first hospitalization department. Due to less fractures and more internal injuries and open wounds we found reduced use of orthopedic wards and increased need for debridement of wounds and for surgical beds. Excess proportions of nerve and blood vessel injuries pose a need for unique subspecialties to be on call and become available to treat once a mass casualty explosion terror event occurs. While children were injured, these were mostly youth (15–17 years of age)20–22; thus, they were usually treated by general surgeons and hospitalized in the general wards.
In grasping the whole picture, it is important to note that registry data do not contain information on casualties that die on the scene. While this does not reflect on what hospitals need to be prepared for, and in that respect it is beyond the scope of this paper, it is still an interesting inquiry.
CONCLUSION
Bombs containing metal fragments detonated by suicide bombers in crowded locations change patterns of injury type and injury severity in a civil population. Specific injuries will require tailored approaches, an open mind, and close collaboration and cooperation between trauma centers across the country, and across the world, to share experience, opinions, and ideas. Findings presented have implications for triage, treatment, diagnosis, hospital organization, and the definition of surge capacity.
ACKNOWLEDGMENTS
The authors thank Dr. Michael Stein, Director of Trauma at the Rabin Medical Center Beilinson Campus, for providing some very important input as well as the photographs.
Footnotes
The Israel Trauma Group (ITG) includes all heads of trauma units participating in the national trauma registry: Drs. R. Alficci, J. Jeroukhimov, B. Kessel, Y. Klein, M. Michelson, A. Rivkind, G. Shaked, D. Simon, D. Soffer, M. Stein, I. Waxman.
Reprints: Limor Aharonson-Daniel, PhD, Gertner Institute for Epidemiology and Health Policy Research, Tel Hashomer, Israel. E-mail: limorad@gertner.health.gov.il.
REFERENCES
- 1.DePalma RG, Burris BG, Champion HR, et al. Blast injuries. N Engl J Med. 2005;352:13:1335–1342. [DOI] [PubMed] [Google Scholar]
- 2.Philips YY. Primary blast injuries. Ann Emerg Med. 1986;15:1446–1450. [DOI] [PubMed] [Google Scholar]
- 3.Katz E, Ofek B, Adler J, et al. Primary blast injury after a bomb explosion in a civilian bus. Ann Surg. 1989;209:484–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kluger Y, Peleg K, Aharonson-Daniel L, et al. The special injury pattern in terrorist bombings. J Am Coll Surg. 2004;199:875–879. [DOI] [PubMed] [Google Scholar]
- 5.Arnold JL, Tsai MC, Halpern P, et al. Mass casualty, terrorist bombings: I. Epidemiological outcomes, resource utilization and the time course of emergency needs. Prehospital Disaster Med. 2003;18:220–234. [DOI] [PubMed] [Google Scholar]
- 6.Halpern P, Tsai MC, Arnold JL, et al. Mass casualty, terrorist bombings: II. Implications for Emergency Department and hospital emergency response. Prehospital Disaster Med. 2003;18:235–241. [DOI] [PubMed] [Google Scholar]
- 7.Peleg K, Aharonson-Daniel L, Stein M, et al. Gunshot and explosion injuries: characteristics, outcome and Implications for care of terror-related injuries in Israel. Ann Surg. 2004;239:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frykberg ER, Tepas JJ. Terrorist bombings lessons learned from Belfast to Beirut. Ann Surg. 1988;208:569–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peleg K, Aharonson-Daniel L, Stein M, et al. Patterns of injury in hospitalized terrorist victims. Am J Emerg Med. 2003;21:258–262. [DOI] [PubMed] [Google Scholar]
- 10.Feigenberg Z. Multicasualty incidents caused by terrorist bombing explosions treated by Magen David Adom in Israel [Abstract]. 11th World Congress on Emergency and Disaster Medicine. www.pdm.medicine.wisc.edu/wademtoc.htm#medical.
- 11.Einav S, Feigenberg Z, Waisman C, et al. Evacuation priorities in mass casualty terror related events: implications for contingency planning. Ann Surg. 2004;239:304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hogan DE, Waeckerie JF, Dire DJ, et al. Emergency department impact of the Oklahoma city terrorist bombing. Ann Emerg Med. 1999;34:160–167. [DOI] [PubMed] [Google Scholar]
- 13.Frykberg ER, Tepas JJ, Alexander RJ. The 1983 Beirut Airport terrorist bombing: injury patterns and implications for disaster management. Am Surgeon. 1989;55:135–141. [PubMed] [Google Scholar]
- 14.Stein M, Hirshberg A. Limited mass casualties due to conventional weapons: a daily reality of a level 1 trauma center. In: Shemer J, Shoenfeld Y, eds. Terror and Medicine. Berlin: Pabst Science, 2003:385 [Google Scholar]
- 15.Kluger Y. Bomb explosions in acts of terrorism: detonation, wound ballistics, triage and medical concerns. Isr Med Assoc J. 2003;5:235–240. [PubMed] [Google Scholar]
- 16.Almogy G, Belzberg H, Mintz Y, et al. Suicide bombing attacks: update and modifications to the protocol. Ann Surg. 2004;239:295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shaham D, Sella T, Makori A, et al. The role of radiology in terror injuries. Isr Med Assoc J. 2002;4:564–567. [PubMed] [Google Scholar]
- 18.Braverman I, Wexler D, Oren M. A novel mode of infection with hepatitis b: penetrating bone fragments due to the explosion of a suicide bomber. Isr Med Assoc J. 2002;4:525–529. [PubMed] [Google Scholar]
- 19.Lynn M, Farkash U, Maor R, et al. Epidemiological and medical aspects of terrorism [Abstract]. 11th World Congress on Emergency and Disaster Medicine. www.pdm.medicine.wisc.edu/wademtoc.htm#medical.
- 20.Aharonson-Daniel L, Waisman Y, Dannon YL, et al. Epidemiology of terror-related versus non-terror-related traumatic injury in children. Pediatrics. 2003;112:e280. [DOI] [PubMed] [Google Scholar]
- 21.Waisman Y, Aharonson-Daniel L, Mor M, et al. The impact of terrorism on children: a two year experience. Prehospital Disaster Med. 2003;18:242–248. [DOI] [PubMed] [Google Scholar]
- 22.Amir L, Aharonson-Daniel L, Peleg K, et al. The Israel Trauma Group: the severity of injury in children resulting from acts against civilian populations. Ann Surg. 2005;241:666–670. [DOI] [PMC free article] [PubMed] [Google Scholar]


