Abstract
Aims:
To evaluate, in a prospective, randomized, single-institution trial, the role of early laparoscopy in the management of nonspecific abdominal pain (NSAP) in young women.
Patients and Methods:
Women aging from 13 to 45 years, admitted for NSAP at the emergency department, were included in the study. Exclusion criteria were pregnancy, previous appendectomy, contraindications to laparoscopy, diagnosis of malignancy, or chronic disease. NSAP was defined as an abdominal pain in right iliac or hypogastric area lasting more than 6 hours and less than 8 days, without fever, leukocytosis, or obvious peritoneal signs and uncertain diagnosis after physical examination and baseline investigations including abdominal sonography. Patients were randomly assigned to early (<12 hours from admission) laparoscopy group (LAP) or to clinical observation group (OBS). After discharge a follow-up was carried out.
Results:
From January 2001 to February 2004, 508 female patients without previous abdominal surgery were evaluated in admitting area for acute right iliac or hypogastric abdominal pain, in 373 patients diagnosis was established for obvious signs or with baseline investigations. Of the remaining 135 patients, 31 were excluded from study for various reasons, 53 patients were randomly assigned to LAP and 51 to OBS. Groups were similar for age, mean BMI, white blood cell count, and duration of pain. During hospitalization diagnosis was established in 83.4% of the LAP and in 45.1% of OBS (P < 0.05). Twenty patients of OBS (39.2%) were operated during observation because of worsening of symptoms or appearance of peritoneal sign. Diagnoses in LAP were appendicitis in 16 patients (30.1%), pelvic inflammatory disease in 7 (13.2%), carcinoid in 1 (1.9%), other in 18 (33.9%), no diagnosis in 11 (20.7%); diagnoses in OBS were appendicitis in 3 patients (5.8%), pelvic inflammatory disease in 8 (15.6%), other in 12 (23.5%), and no diagnosis in 28 (54.9%). Mean length of hospital stay was 3.7 ± 0.8 days in LAP and 4.7 ± 2.4 days in OBS (P < 0.05); no differences were found regarding mortality, morbidity, radiation dose, and analgesia. Mean follow-up time was 29.3 months (range, 12–60 months) for LAP and 30.6 months for OBS (range, 12–60 months). After 3 months from discharge, 20% of patients in LAP and 52% in OBS had recurrent abdominal pain (P < 0.05); after 12 months, 16% in LAP and 25% in OBS (P = not significant). Six patients in OBS required readmission for surgery.
Conclusions:
Compared with active clinical observation, early laparoscopy did not show a clear benefit in women with NSAP. A higher number of diagnosis and a shorter hospital stay in the LAP group did not led to a significant reduction in symptoms recurrences at 1 year.
When compared with active clinical observation, early laparoscopy did not show a clear benefit in women with nonspecific abdominal pain. A higher number of diagnoses and a shorter hospital stay in the laparoscopy group did not lead to a significant reduction in symptom recurrences at 1 year.
Acute nonspecific abdominal pain (NSAP), generally defined as acute abdominal pain of under 7 days’ duration, and for which there is no diagnosis after examination and baseline investigations, is a common cause of emergency surgical hospitalization.1 Among young women, for anatomic, physiologic, and pregnancy motivations, NSAP can be caused by a great number of conditions, including pelvic inflammatory disease (PID), appendicitis, ectopic pregnancy, torsion of adnexa, etc.2
Hospitalization followed by active clinical observation, traditionally defined as “wait and see,” has been the most widely used method of clinical management of patients with nontypical clinical signs. The predictive value of clinical diagnosis reached with this method, which varies with the underlying cause, has been estimated between 68% and 92%.3–6 On the one hand, this method entails risk to patients because of possible complications such as peritonitis, hemorrhage, or infertility; on the other hand, laparotomy might be unnecessarily performed.2,7
Computer-aided diagnostic questionnaires,8 abdominal ultrasound (US),9 abdominal computed tomography (CT) scan,10 and early laparoscopy have all been described as potential methods for improving diagnosis. The role of early laparoscopy compared with the traditional “wait and see” policy in the management of NSAP has been recently evaluated by 2 randomized controlled trials (RCTs).11,12 Because each of these studies presented in our opinion at least one major defect such as limited number of patients,11 insufficient preoperative evaluation,12 enrolling males and females,12 and no long-term follow-up,11 we designed the present RCT to compare, in young women with NSAP, early laparoscopy to active clinical observation in terms of number of diagnosis, length of hospital stay, percentage of symptom recurrence, percentage of hospital readmission, and costs.
METHODS
Female patients of reproductive age were eligible for the trial if they had been admitted for acute abdominal pain of less than 7 days’ duration with uncertain diagnoses after clinical examination and baseline investigations, including a full blood count, blood urea, amylase and bilirubin, serum electrolytes, urinalysis, pregnancy test, abdominal radiograph, and abdominal US. A specific informed-consent form approved by our Institution's Ethics Committee and signed by the candidates was required before inclusion in the trial.
Inclusion criteria were as follows:
Women between the age of 13 and 45 years
Abdominal pain lasting more than 6 hours and less than 7 days
Abdominal pain localized or prevalent in right iliac or suprapubic areas, not accompanied by fever, or leukocytosis (WBC >10,000 cell/mm3), or clinical signs of peritonitis, or hemodynamic instability, or other obvious clinical presentation requiring urgent intervention.
Exclusion criteria were as follows:
Previous appendectomy or major abdominal surgery
Pregnancy
Diagnosis of malignancy or chronic disease
Contraindications to pneumoperitoneum
Patient's refusal to enter the study
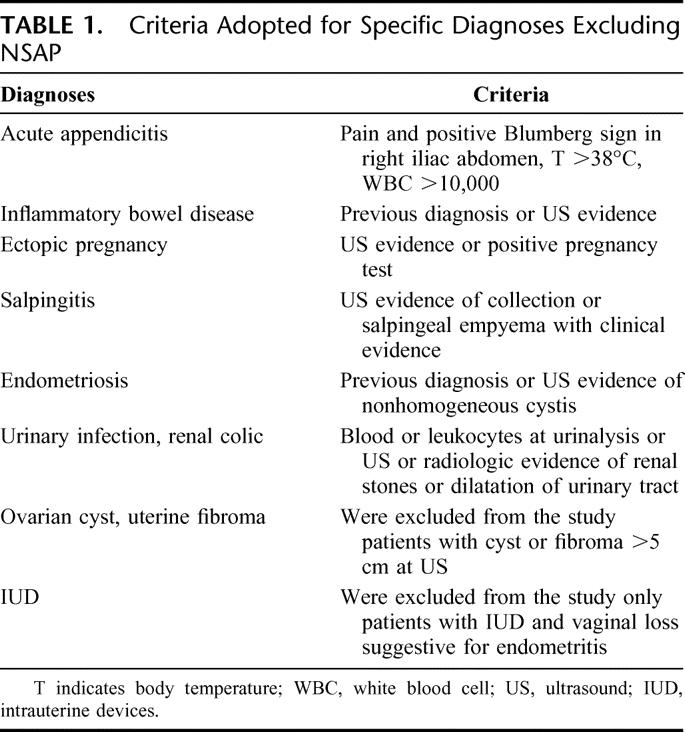
Precise diagnoses after baseline investigations (the criteria we adopted to make a specific diagnosis are reported in Table 1).
TABLE 1. Criteria Adopted for Specific Diagnoses Excluding NSAP
Patients with NSAP fulfilling inclusion criteria, were randomly assigned to 2 different groups: early laparoscopy (LAP) or active clinical observation (OBS).
Group 1: Early Laparoscopy
The patients randomized to early laparoscopy underwent surgery within 12 hours. Laparoscopy was performed using an open Hasson technique for the first port placement in the umbilical area. Once 12 mm Hg CO2 pneumoperitoneum was created, 2 5-mm trocars were inserted in midline suprapubic area and left iliac area. The abdominal cavity was accurately explored in all patients, including a complete mobilization of the entire small bowel. An attempt to treat laparoscopically all surgical pathologies diagnosed at laparoscopy (ie, appendicitis, endometriosis, complicated ovarian cyst, etc) was undertaken. The laparoscopic diagnoses of PID were reached following Hager's criteria.13 When no abnormality was identified at laparoscopy, appendectomy was performed on the basis that symptomatic appendicitis are not always evident at macroscopic examination.14 Whenever serous fluid was present in the abdominal cavity, it was aspirated and sent for microbiologic testing.
Group 2: Observation
The patients randomized to active clinical observation were admitted to the surgical ward. A complete clinical examination was repeated twice a day, baseline hematologic tests were repeated at 24 and 48 hours from admission, and complementary hematologic and/or radiologic investigations were performed on the basis of patient's clinical evolution. Whenever a clinical diagnosis could be defined, the appropriate medical or surgical treatment was immediately undertaken. In the presence of persistent or worsening pain at 48 hours from admission, a laparoscopic procedure was undertaken even in the absence of a diagnosis. On the other hand, in some patients clinical symptoms progressively weakened and finally disappeared before a precise diagnosis could be reached; in such cases, the asymptomatic patient with normal laboratory tests was dismissed undiagnosed.
Outcome Assessment
Variables collected for each group included patient age, sex, body mass index (BMI), white blood cells count (WBC) at admission, body temperature (T) at admission, in-hospital and 30-day morbidity and mortality, and length of hospital stay. In both groups, an estimation of the mean radiation dose (mSv) was undertaken considering the following parameters: 0.1 mSv for a plain thorax, 2 mSv for a plain abdomen, 20 mSv for a CT scan with contrast agent, and 10 mSv for a CT scan without contrast agent. In the LAP group, duration of surgical procedure, conversion rate, and rate of intraoperative diagnosis were recorded. In the OBS group, the number of radiologic investigations undertaken and duration and characteristics (ie, laparoscopic or laparotomic) of surgical procedures undertaken were recorded. Cost evaluation included the cost of baseline and second-line investigations, use of the operating room (nursing and technical staff, surgical devices, and maintenance), cost of hospital stay, and the cost of management of recurrences.
Follow-up visits and clinical examinations were scheduled 1 week after discharge and then at 3 and 12 months. The 2 groups were compared in terms of number of diagnosis at discharge (including histology), percentage of recurrence of symptoms at 3 and 12 months, percentage of readmission at 3 and 12 months’ follow-up, number of surgical interventions after discharge, and in-hospital costs.
Statistical Analysis
The primary endpoint of the study was 1-year symptom recurrence rate. Secondary endpoints were percentage of diagnosis at discharge and in-hospital costs. Appropriate sample size was calculated based on the assumption of a difference of 30% in recurrence of symptoms between LAP and OBS. This difference was considered relevant, and a sample size of 100 patients (50 in each group) was needed to prove this difference (α set at 0.05; β set at 0.2; power = 80%). The study protocol was approved by our Institution's Ethics Committee. Randomization was performed by means of sealed opaque envelopes containing computer-generated random numbers. Categorical variables were compared by χ2 test, with Yates correction and the Fisher exact test (2-tailed) when necessary. Continuous variables were compared by the Student t test or the Mann-Whitney U test, depending on distribution. All P values were 2-sided. A P value of <0.05 indicated a statistically significant difference. Data were analyzed on an intention-to-treat basis. All calculations were done with SPSS (version 10.0) (SPSS Inc. Chicago, IL).
RESULTS
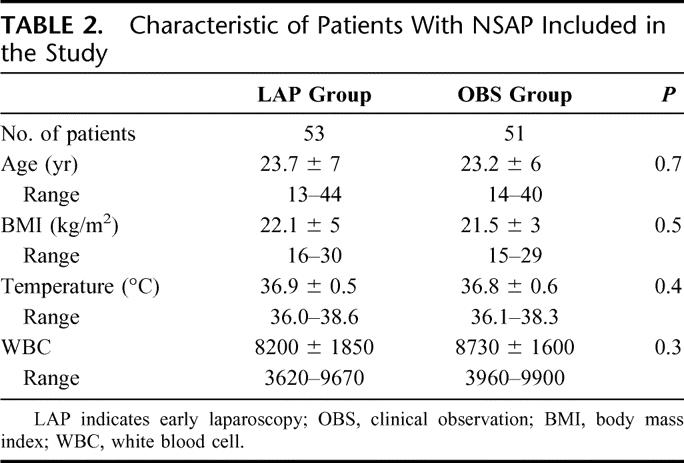
Between January 2001 and February 2004, 508 women without previous abdominal surgery presented the emergency department with acute abdominal pain localized or prevalent in right iliac or suprapubic areas. Among them after clinical examinations and baseline investigations, 135 patients were defined as NSAP (Fig. 1); 3 of them presented a contraindication to pneumoperitoneum (1 glaucoma, 2 pulmonary atelectasia). Therefore, a total of 132 eligible patients were approached and 28 refused to enter the study. This was either because they refused any surgery or because they insisted on early laparoscopy. A total of 104 patients were randomized to either early laparoscopy (53 patients) or active clinical observation (51 patients). The age, mean BMI, mean body temperature, and white blood cell count in the 2 groups were comparable (Table 2).
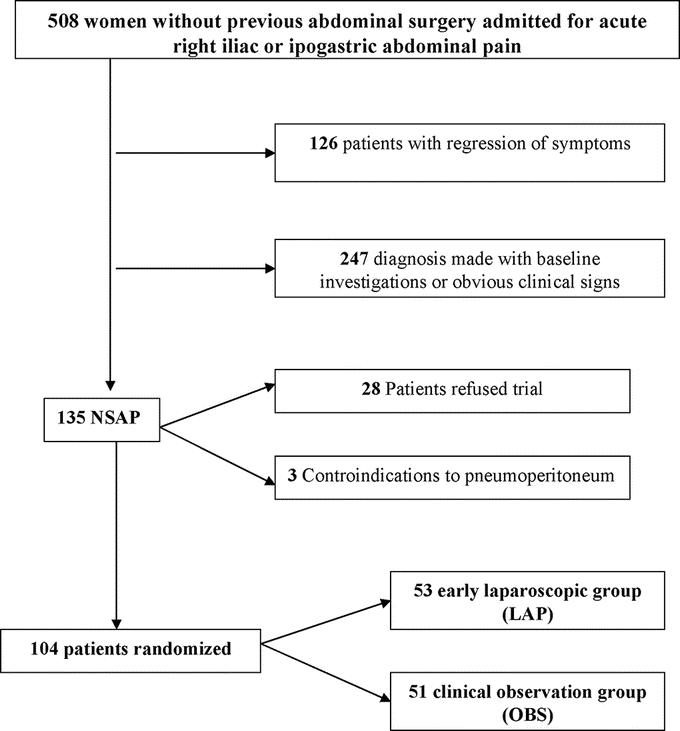
FIGURE 1. Study design according to the consort statement.
TABLE 2. Characteristic of Patients With NSAP Included in the Study
LAP Group
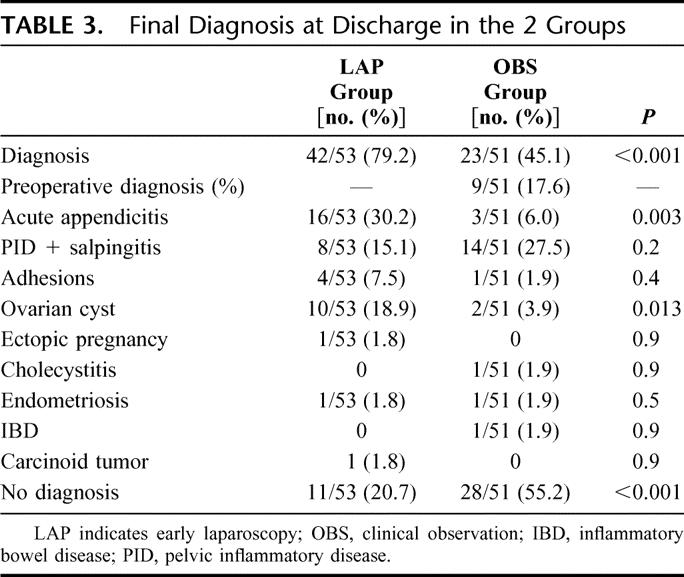
Patients in this group underwent laparoscopy 3 to 12 hours after hospital admission (mean, 7.5 hours). There were no conversions to open surgery. Mean operative time was 60.1 ± 18.6 minutes (range, 30–120 minutes). A clinical macroscopic diagnosis was possible in 42 patients (79.2%) (Table 3). In 11 patients (20.7%), laparoscopy did not reveal any pathologic finding. In 52 cases (98%), a laparoscopic appendectomy was carried out. In all cases, a histologic examination was performed revealing a pathologic appendix in 17 cases (32%), including 1 carcinoid tumor and 16 acute appendicitis according to Carr and Path.15 There was no mortality; morbidity was limited to 2 cases (3.7%): 1 urinary tract infection and 1 trocar site infection. The duration of hospital stay was 3.7 ± 0.8 days (range, 2–5.4 days). Mean radiation dose per patient was 1.1 ± 1 mSv (range, 0.1–2.1 mSv).
TABLE 3. Final Diagnosis at Discharge in the 2 Groups
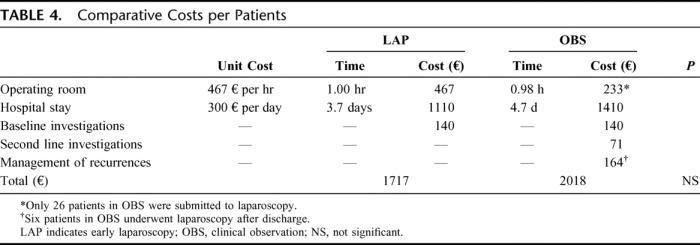
Mean costs per patient are reported in Table 4.
TABLE 4. Comparative Costs per Patients
Mean follow-up was 29.3 months (range, 12–60 months). At the 3-month follow-up, 5 patients (9.4%) were lost. Abdominal pain persisted in 10 of 48 patients (20.8%); 8 patients (16.6%) presented to the emergency department during this period. Among the 10 patients with persisting NSAP, 3 had been dismissed without a diagnosis, 2 had a histologic diagnosis of acute appendicitis, 3 had a complicated ovarian cyst, 1 was dismissed with a diagnosis of PID, and 1 was dismissed with a diagnosis of adhesions. The remaining 38 patients (79.2%) remained completely asymptomatic during this period.
At the 12-month follow-up, 9 patients were lost (16.9%). Abdominal pain persisted in 7 of 44 patients (15.9%); 3 patients presented to the emergency department during this period. Among the 7 patients with persisting NSAP, 3 have been dismissed without diagnosis, 2 presented a diagnosis of adhesions, 1 a diagnosis of PID and 1 a complicated ovarian cyst; 37 patients (84.1%) related a complete regression of symptoms. No surgical procedures were performed in the LAP group during the entire follow-up period.
OBS Group
In this group, a clinical diagnosis was possible in 23 of 51 patients (45.1%) (Table 3): 17 diagnosis were established during a delayed laparoscopy and 6 with other nonsurgical methods (an abdominal CT scan in 2 patients, a transvaginal US in 3, and an abdominal magnetic resonance in 1).
Twenty patients (39.2%) underwent a laparoscopic procedure as a consequence of the persistence or worsening of abdominal pain. Laparoscopic exploration was undertaken 69.1 ± 50.9 hours (range, 15–168 hours) after admission. There were no conversions to open surgery. Mean operative time was 58.9 ± 14.8 minutes (range, 30–90 minutes). A clinical macroscopic diagnosis during laparoscopy was possible in 17 patients (85%). In 3 patients (15%), laparoscopy did not reveal any pathologic finding. In 17 cases (85%), a laparoscopic appendectomy was carried out. In all cases, a histologic examination was performed, revealing an acute appendicitis in 3 cases (17.6%) according to Carr and Path.15 There was no mortality; morbidity was limited to 1 case of severe anemia (1.9%). The duration of hospital stay was 4.7 ± 2.4 days (range, 2–10 days). Radiologic investigations undertaken during active observation included 14 abdominal US, 9 transvaginal US, 4 CT scan, 1 abdominal RMN, and 3 plain abdominal radiography. Mean radiation dose per patient was 2.2 ± 5.1 mSv (range, 0–22 mSv).
Mean costs per patient are reported in Table 4.
Mean follow-up was 30.6 months (range, 12–60 months). At the 3-month follow-up, 5 patients (9.8%) were lost. Abdominal pain persisted in 24 of 46 patients (52.2%); 9 patients (19.6%) presented to the emergency department during this period. Among the 24 patients with persisting NSAP, 16 (66.6%) had been dismissed without a diagnosis, 3 had a diagnosis of salpingitis, 1 had a complicated ovarian cyst, 2 were dismissed with a diagnosis of PID, 1 with a diagnosis of adhesions and 1 of endometriosis (5 of these diagnosis had been the consequence of a laparoscopic exploration). Four (8.7%) patients underwent a laparoscopic exploration during the follow-up period: 3 appendicitis and 1 PID. The remaining 22 patients (47.8%) remained completely asymptomatic.
At the 12-month follow-up, 7 patients were lost (13.7%). Abdominal pain persisted in 11 of 44 patients (25%). During follow-up, 4 (9.1%) patients presented to the emergency department and 2 underwent a laparoscopic procedure (2 appendicitis). Among the 11 patients with persisting NSAP, 6 (54.5%) had been dismissed without diagnosis, 2 presented a diagnosis of salpingitis, 1 a diagnosis of PID, 1 a complicated ovarian cyst, and 1 an endometriosis. The recurrence rate was higher in the subgroup of patients not submitted to laparoscopy (35%; 11 of 31) compared with those submitted to delayed laparoscopy (0%). Thirty-three patients (75%) related a complete regression of symptoms.
Comparative Analysis
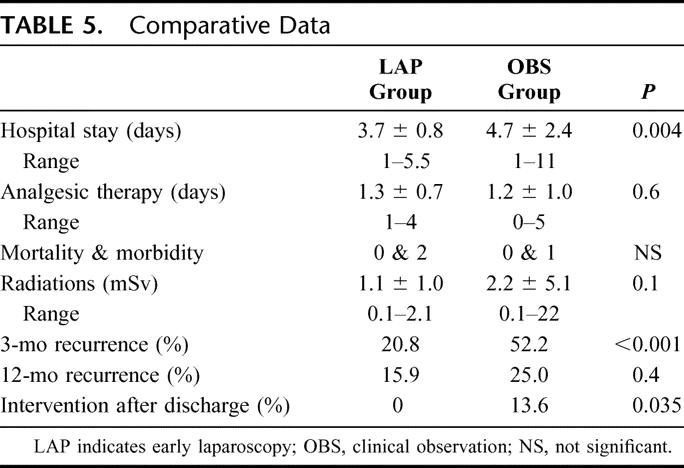
Comparative data are reported in Tables 3 and 5. There were no differences between the 2 groups in terms of mortality, morbidity, mean radiation dose, or costs. LAP group patients had a significantly reduced hospital stay, a significantly higher percentage of diagnosis, and a significantly lower percentage of recurrent abdominal pain at 3 months but not at the 1-year follow up.
TABLE 5. Comparative Data
DISCUSSION
NSAP is a significant problem in general surgery and accounts for an estimated 13% to 40% of emergency surgical admissions for acute abdominal pain.1,16 The mean hospital stay for patients admitted with NSAP ranges between 4 and 6 days, using the traditional “wait and see” management.2 This includes repeated clinical examination, radiologic investigation, and a gynecologic opinion. A delay in surgical intervention while further investigations are performed may increase morbidity and prolong hospital stay. The end result may be an unsatisfactory discharge from hospital after a prolonged stay, with a high percentage of patients leaving the hospital without a precise clinical diagnosis.
Many suggestions have been made about improving diagnostic rates in acute NSAP. DeDombal et al17 have suggested that the proportion of correct diagnoses can be greatly increased by the use of structured questionnaires and diagnostic programs on computers. Although computer-aided diagnosis can improve diagnostic rates by at least 20%, these programs are unpopular.8,18 Other researchers have suggested ultrasonography,9 thermography, peritoneal cytology, CT, and more recently spiral computer tomography.10 Nevertheless, none of these techniques seems to have been determinant in improving the clinical management of NSAP.
In the management of acute abdomen laparoscopy has both a diagnostic and a therapeutic role. The use of diagnostic laparoscopy in patients with acute abdominal pain is not new,19 and many studies have demonstrated an improvement in surgical decision making associated with its use, particularly when the need of operation is uncertain.2 Therefore, NSAP appears to be a good indication to early laparoscopy to improve diagnostic rates and reduce hospital stay and costs.
In the 1990s, 2 RCTs compared early laparoscopy to active clinical observation.11,12 Both trials showed that early laparoscopy clearly facilitated the establishment of a diagnosis with subsequent therapy (97% and 81% after early laparoscopy vs. 28% and 36% after clinical observation), whereas more patients in the control group left the hospital without a clear diagnosis. Furthermore, hospital stay was shorter in the laparoscopic group in both trials, while morbidity and mortality were similar. Although these trials had comparable results, their design presented in our opinion some limits. The study by Champault et al11 did not include abdominal ultrasound among the baseline examinations, presented results limited to the perioperative period and was limited in its statistical power due to a small number of patients (30 in each group). We think that nowadays abdominal ultrasound should be part of the baseline investigations of an acute abdomen,20 and that a minimum of 12 months of follow-up is essential to evaluate NSAP recurrence rate. Furthermore, while NSAP literature is focused exclusively on right iliac fossa pain in young women, the study by Decadt et al12 included men and women with acute abdominal pain regardless of pain localization.
Our prospective RCT, focused on acute right iliac fossa pain in young women, confirms that early laparoscopy results in a higher diagnostic rate and in a shorter hospital stay compared with active observation, while morbidity, mortality, and costs are similar. However, while at 3 months LAP group patients had a significantly lower pain recurrence rate (20% vs. 52%; P < 0.001), such a difference is consistently reduced at 12 months (16 vs. 25%; P = not significant). Early laparoscopy produced a significantly higher rate of clinical diagnosis compared with active observation: 79.2% versus 45.1% (P < 0.001). In accordance to Champault et al11 and Decadt et al,12 this difference was mainly due to a higher rate of acute appendicitis in the LAP group: 30% versus 5.6% (P = 0.003). Is this 25% difference clinically relevant or mainly based on histology and the majority of poorly symptomatic appendicitis will spontaneously resolve in the follow-up period? The significant reduction in pain recurrence rate in OBS group during the follow-up period (25% at 12 months vs. 52% at 3 months) seems to be strongly in favor of the second hypothesis. In the LAP group, the policy to remove the appendix if no other clear cause of pain was found was adopted in accordance to data showing that external inspection of the appendix at laparoscopy is an unreliable guide to the presence of appendicitis.14 Furthermore, Greason et al21 showed that routine appendectomy during diagnostic laparoscopy does not increase morbidity and does not prolong hospital stay. Nevertheless, our study clearly shows that removing a “normal looking” appendix has a limited clinical role when the follow-up is adequate.
The overall incidence of pelvic disorders diagnosed in the 2 groups was similar (33.9% vs. 31.4%), but the final diagnosis differed with a higher incidence of ovarian cysts (18.9% vs. 3.9%) and a lower incidence of PID (15% vs. 27.5%) in the LAP group. These data confirm the difficulty of reaching an accurate clinical diagnosis in young women with NSAP and the high variability of specific diagnostic rates established with different diagnostic modalities11,12,22
A total of 26 patients (51%) in the OBS group underwent a surgical procedure (20 during the first admission, 6 during the follow-up period). These patients were all operated by laparoscopy, mean operative time was equal to mean operative time in LAP group and there was no morbidity or mortality. Therefore, delaying surgery in NSAP patients does not increase operative risks or jeopardize clinical results. Furthermore, 49% of patients in OBS group avoided a surgical procedure under general anesthesia; these data are similar to those reported by Decadt et al with 70% of patients in the active observation group that avoided surgery without increased morbidity.12 In a recent RCT comparing early laparoscopy to active observation in a group of 110 women treated in a maternity hospital, Gaitàn et al reached similar conclusions stating that, although patients treated by early laparoscopy had a shorter hospital stay (3.7 vs. 4.7 days) and more accurate diagnosis (83% vs. 45%), this greater accuracy did not show clear clinical benefits (recurrent pain at 12 months: 16% vs. 25%, not significant).22 They added that “laparoscopy might be more useful for patients who do not have a diagnosis within 48 hours of admission.”22
We agree with Poulin et al that the “management of acute NSAP needs to be periodically adjusted to get the best outcomes at the lowest costs and with the least invasive and most appropriate diagnostic tools.”23 The management of acute NSAP can be divided in 3 stages. The first stage is the initial history, physical examination, baseline investigations, and formulation of a working and differential diagnosis. As already stated, ultrasonography should at present be included among the baseline investigation in cases of acute abdominal pain.20 If at this stage a diagnosis is not made, the second stage involves the judicious use of radiologic techniques. An understanding of the limitations of different radiologic techniques is needed so that their use is appropriate for the patient and cost-effective, and avoids multiple procedures. For many centers, spiral CT has become the primary imaging technique for the evaluation of the patient with acute abdominal pain and a confused clinical picture.24 If the diagnosis is still uncertain, then the third stage is possibly laparoscopy under general anesthesia.22 Our study shows that delaying the clinical decision to submit the patient to laparoscopy 24 to 72 hours from admissions if symptoms persist without a diagnosis (observation group) could reduce the number of patient submitted to surgery without clinical negative effects.
A major point in the present series is that all patients submitted to surgery during the study period were treated by laparoscopy without the need for conversions. In accordance with other authors,2,11,12,21,22 we think that at present open surgery has a very limited role in the management of NSAP.
CONCLUSION
In the present study, early laparoscopy did not show a clear benefit in women with NSAP. A higher number of diagnoses and a shorter hospital stay in the LAP group did not led to a significant reduction in symptoms recurrence at 1 year. A selective indication to laparoscopy after a short period of active clinical observation reduces the need for surgery without significant clinical disadvantages.
Discussions
Dr. Andrew Kingsnorth: Thank you very much for giving me the opportunity to discuss this paper, which was a comprehensive analysis of a very well set up study. You gave us a lot of data and you also gave us a good overview of the background to the problem of NSAP. I would just like to go through one or two points. The first thing is the definition of NSAP, which is not really a single disease entity but is a presenting symptom of a large number of minor and self-limiting conditions. An important aspect is that often there is an underlying psychological basis for the symptoms. Therefore, could I have the first point on my slide? In 1990, Rahija called designated NSAP as “an expensive mystery,” which I think was very apposite. In your last slide, you showed us your cost implications of NSAP and the fact that you can save money by performing laparoscopy. If I could have the second point, what we've got to bear in mind is that laparoscopy is a fairly aggressive pursuit of the diagnosis since it involves a general anesthetic and obviously the occasional danger of a trocar injury to one of the abdominal viscera. Laparoscopy may avoid unnecessary surgery, and you showed that you avoided performing any laparotomies on your patients, which is clearly a cost-saving. The questions I have to ask you are: First, why did you exclude men, when we know that they actually account for about 25% of admissions with NSAP, and NSAP itself accounts for about 30% of acute surgical admissions. Therefore, it is a considerable number of patients that you have discounted from the study. Second, you did help us out with some of the discussions about the diagnosis of acute appendicitis, but I think you could take that a little bit further. You had 30% of patients who had histologic acute appendicitis in the laparoscopy group but only 6% in the control group, and this was very similar to the CAT study. Is this because it is only a histologic diagnosis or is it because 25% of our patients recover from early acute appendicitis? Were any of these patients put on antibiotics for some reason just because they had a pyrexia, and what was the follow-up in the patients? We know that, in fact, these patients who stay in hospital for 2 or 3 days may be admitted in the future and get their appendix removed for proven acute appendicitis. Did any of the observation group later undergo appendicectomy?
The final point I have to make is that an alternative strategy, which is the final point on this slide, is that perhaps laparoscopy is rather overaggressive and perhaps instead the judicious use of alternative radiology, such as CT scanning, should be used in selected cases and obviously with caution in young women. There is a difference between your abstract and what you told us just now. Most people will use the algorithm you've used at clinical examination and a number of tests, including ultrasound, but they don't use plain abdominal x-ray. What extra yield is that going to give you in this group of patients, who are young women whom you are exposing to radiation with a plain abdominal x-ray?
Dr. Mario Morino: Thank you for a very comprehensive discussion of my paper and for a number of questions. I will start with the last one, maybe the easiest one. Why did we undertake the plain abdominal radiography? Essentially because all the studies that have been published in the last 15 years put this among the baseline investigations, but I think that I agree with you that probably this should not be a routine examination since it did not add very much to the study. And along the same lines, you commented on CT scan. It is true that CT scan was proposed as one of the ways of improving the percentage of diagnoses. There are even some computed-based algorithms that help for diagnosis, but in previous publications the percentage of these improvements was not so significant. Moreover, I think that all over the world a CT scan is not available at all times in an emergency setting, so we were interested to propose laparoscopy also as a way to shorten the preoperative stage.
Concerning the question of gender, of the four studies in the literature, there is only one study, the one by Decadt, which included men, and it seemed to all the commentators and also to me that including men did make interpretation of these results more difficult. You need a larger number of patients, and at least, in my clinical experience and of my group, the real problems usually are in women of reproductive age. So I think that on this point there is consensus in the literature to focus on women in the reproductive age.
Finally, I think that you have identified that the main problem of the pathology in this study is the diagnosis of appendicitis. The difference was 25% at discharge but 6 patients had to be operated in the follow-up period, in the wait and see group, which is 13%, plus 6 making 20%; so the difference is 20% versus 30%. A 10% difference is not so high, and it seems from the present study that some cases of mild appendicitis do not require an operation and these patients will slowly recover in the postdischarge period. This is one of the reasons why we consider at present that, although laparoscopy is a minimally invasive procedure, avoiding surgery is even less invasive. Therefore, we prefer to have a short hospital surveillance of these patients and eventually to decide on laparoscopy in the first 48 hours.
Dr. Stefan Post: Congratulations for the nice study, but I just would like to challenge your view of routine appendectomy in these cases. I can completely agree that, if you don't find any other explanation for the pain, you might take out the appendix. However, you have more than 20 cases in your group that had an overt other explanation for the pain. They had adhesions, or they had complicated ovarian cysts, or even they had an inflammatory process in the pelvis such as salpingitis or PID and still you took out the appendix. I cannot understand this philosophy.
Dr. Mario Morino: It is difficult for me to give an overall answer. Therefore, in the protocol, we decided to do as many appendectomies as possible for the following reason: in the majority of cases, the surgeon at laparoscopy was not a 100% certain that, for example, adhesions or an apparent macroscopic diagnosis of PID or an ovarian cyst could justify the patient's symptoms. As a consequence, in such cases, the appendix was removed even in the presence of another potential diagnosis. Furthermore, the relationship between the macroscopic and the histologic appearances of the appendix are not very clear in the literature. Moreover, it was well demonstrated that appendectomy does not add any complication and does not modify hospital stay. I think that now we have correlated the appearance with the histology findings in these 50 patients, this has improved a little bit our appreciation of appendicitis. Probably we will improve on this side, doing less appendectomies during exploratory laparoscopy.
Footnotes
Reprints: Mario Morino, MD, C.so A.M. Dogliotti, 14, 10126 Torino, Italy. E-mail: mario.morino@unito.it.
REFERENCES
- 1.Sheridan WG, White AT, Havard T, et al. Non specific abdominal pain: the resource implications. Ann R Coll Surg Engl. 1992;74:181–185. [PMC free article] [PubMed] [Google Scholar]
- 2.Paterson-Brown S. Emergency laparoscopy surgery. Br J Surg. 1993;80:279–283. [DOI] [PubMed] [Google Scholar]
- 3.Raheja SK, McDonald P, Taylor I. Non specific abdominal pain an expensive mystery. J R Soc Med. 1990;88:10–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hawthorn IE. Abdominal pain as a cause of acute admission to hospital. J R Coll Surg Edinb. 1992;37:389–393. [PubMed] [Google Scholar]
- 5.Sellors J, Mahony J, Goldsmith C, et al. The accuracy of clinical findings and laparoscopy in pelvic inflammatory disease. Am J Obstet Gynecol. 1991;164:113–120. [DOI] [PubMed] [Google Scholar]
- 6.Brown DL, Doulbilet PM. Transvaginal sonography for diagnosing ectopic pregnancy: positive criteria and performance characteristics. J Ultrasonogr Med. 1994;13:259–266. [DOI] [PubMed] [Google Scholar]
- 7.Olsen JB, Myrén CJ, Haahr PE. Randomized study of the value of laparoscopy before appendectomy. Br J Surg. 1993;80:922–923. [DOI] [PubMed] [Google Scholar]
- 8.Adams ID, Chan M, Clifford PC, et al. Computer aided diagnosis of acute abdominal pain: a multicentre study. BMJ. 1986;293:800–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allemen F, Cassina P, Rothlin M, et al. Ultrasound scans done by surgeons for patient with acute abdominal pain: a prospective study. Eur J Surg. 1999;165:966–967. [DOI] [PubMed] [Google Scholar]
- 10.Rao PM, Rhea JT, Novelline RA, et al. Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med. 1998;338:141–146. [DOI] [PubMed] [Google Scholar]
- 11.Champault G, Rizk N, Lauroy J, et al. Right iliac fosse in women: conventional diagnostic approach versus primary laparoscopy. A controlled study (65 cases). Ann Chir. 1993;47:316–319. [PubMed] [Google Scholar]
- 12.Decadt B, Sussman L, Lewis MO, et al. Randomized clinical trial of early laparoscopy in the management of acute non-specific abdominal pain. Br J Surg. 1999;86:1383–1386. [DOI] [PubMed] [Google Scholar]
- 13.Hager WD, Eschembach DA, Spence MR, et al. Criteria for diagnosis and grading of salpingitis. Obstet Gynecol. 1983;61:113–114. [PubMed] [Google Scholar]
- 14.Grunewald B, Keating J. Should the ‘normal’ appendix be removed at operation for appendicitis? J R Coll Surg Edinb. 1993;38:158–160. [PubMed] [Google Scholar]
- 15.Carr NJ, Path MRC. The pathology of acute appendicitis. Ann Diagn Pathol. 2000;4:46–58. [DOI] [PubMed] [Google Scholar]
- 16.Irvin TT. Abdominal pain: a surgical audit of 1190 emergency admission. Br J Surg. 1989;76:1121–1125. [DOI] [PubMed] [Google Scholar]
- 17.DeDombal FT, Leaper DJ, Horrocks JC, et al. Human and computer-aided diagnosis of abdominal pain: further report with emphasis on performance of clinicians. BMJ. 1974;1:376–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sutton GC. Computer-aided diagnosis: a review. Br J Surg. 1989;76:82–85. [DOI] [PubMed] [Google Scholar]
- 19.Sugarbaker PH, Bloom BS, Sanders JH, et al. Preoperative laparoscopy in diagnosis of acute abdominal pain. Lancet. 1975;1:442–445. [DOI] [PubMed] [Google Scholar]
- 20.Allemen F, Cassina P, Rothlin M, et al. Ultrasound scans done by surgeons for patients with acute abdominal pain: a prospective study. Eur J Surg. 1999;165:966–970. [DOI] [PubMed] [Google Scholar]
- 21.Greason KL, Rappold JF, Liberman MA. Incidental laparoscopic appendectomy for acute right lower quadrant abdominal pain. Surg Endosc. 1998;12:223–225. [DOI] [PubMed] [Google Scholar]
- 22.Gaitàn H, Angel E, Sànchez J, et al. Laparoscopic diagnosis of acute lower abdominal pain in women of reproductive age. Int J Gynecol Obstet. 2002;76:149–158. [DOI] [PubMed] [Google Scholar]
- 23.Poulin EC, Schlachta CM, Mamazza J. Early laparoscopy to help diagnose acute non-specific abdominal pain. Lancet. 2000;355:861–863. [DOI] [PubMed] [Google Scholar]
- 24.Gupta H, Dupuy DE. Advances in imaging of the acute abdomen. Surg Clin North Am. 1997;77:1245–1263. [DOI] [PubMed] [Google Scholar]


