We describe a case of autoimmune hepatitis triggered by an acute hepatitis A infection. A young woman presented with a 10 day history of nausea and dark urine having returned from Tunisia a month previously. She had marked transaminitis. Viral serology demonstrated positive hepatitis A immunoglobulin M. Other viral serology was negative. Autoantibody screening revealed positive antismooth muscle antibodies (titre 1 in 80) but negative antinuclear (ANA), antimitochondrial, and antiliver, kidney and pancreas (LKM) antibodies. Immunoglobulin levels revealed normal IgA and IgG levels with a raised IgM at 5.53 g/l (range 0.60–2.50). Abdominal ultrasound scan was normal. She was diagnosed with acute hepatitis A.
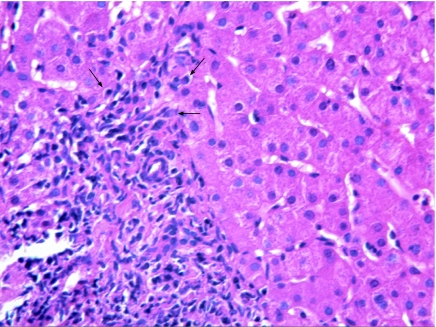
Liver function tests normalised within two months. One month later her alanine aminotransferase levels began to increase. Autoantibody screen was positive for ANA (titre 1 in 40) and SMA was negative. However, immunoglobulin G was raised at 18.6 g/l (range 6–16) and serum electrophoresis showed a polyclonal increase in gamma globulins. Liver histology showed interface portal inflammation with plasma cell (fig 1) associated interface hepatitis with involvement of lobular and perivenular hepatocytes, consistent with autoimmune hepatitis (AIH). She was successfully treated with immunosuppression.
Figure 1 Liver histology revealing multiple plasma cells (arrowed).
Studies suggesting triggering factors for the development of AIH have been reported in the past and include Epstein‐Barr virus,1 and hepatitis B and hepatitis A infection.2 Although SMA was initially positive in our patient, this was probably because of the viral infection.
Using the diagnostic scoring system of the American Association for the Study of Liver Diseases (AASLD) (see table 1) for the diagnosis of AIH, our patient scored 16 before steroid treatment (definite diagnosis is >15) and 18 after steroid treatment (definite diagnosis is >17). The sensitivity of this scoring system for the diagnosis of AIH is quoted by the AASLD as 97–100%.
Table 1 Diagnostic scoring system of the American Association for the Study of Liver Diseases.
| Category | Factor | Score |
|---|---|---|
| Sex | Female | +2 |
| ALP:AST (or ALT) ratio | >3 | −2 |
| <1.5 | +2 | |
| γ‐globulin or IgG (× above upper limit of normal) | >2.0 | +3 |
| 1.5–2.0 | +2 | |
| 1.0–1.5 | +1 | |
| <1.0 | 0 | |
| ANA, SMA or anti‐LKM1 titres | >1:80 | +3 |
| 1:80 | +2 | |
| 1:40 | +1 | |
| <1:40 | 0 | |
| AMA | Positive | −4 |
| Viral markers of active infection | Positive | −3 |
| Negative | +3 | |
| Hepatotoxic drugs | Yes | −4 |
| No | +1 | |
| Alcohol | <25 g/day | +2 |
| >60 g/day | −2 | |
| Concurrent immune disease | Any non‐hepatic disease of an immune nature | +2 |
| Other autoantibodies | Anti‐SLA/LP, actin, LC1, pANCA | +2 |
| Histological features | Interface hepatitis | +3 |
| Plasma cells | +1 | |
| Rosettes | +1 | |
| None of the above | −5 | |
| Biliary changes | −3 | |
| Atypical features | −3 | |
| HLA | DR3 or DR4 | +1 |
| Treatment response | Remission alone | +2 |
| Remission with relapse | +3 | |
| Pretreatment score | ||
| Definite diagnosis | >15 | |
| Probable diagnosis | 10–15 | |
| Post‐treatment score | ||
| Definite diagnosis | >17 | |
| Probable diagnosis | 12–17 |
ALP, alkaline phosphatase; ALT, alanine aminotransferase antinuclear; AMA, antimitochondrial antibodies; ANA, antinuclear antibodies; anti‐SLA/LP, antibodies to soluble liver antigen/liver panareas; anti‐LCq, antibodies to liver cytosol type 1; AST, aspartate aminotransferase; LKM, antiliver, kidney and pancreas antibodies; pANCA, perinuclear antineutrophil cytoplasmic antibodies.
Acute hepatitis secondary to hepatitis A infection is a common cause of viral hepatitis in humans and is usually self limiting and resolves within weeks. However, it may lead to fulminant liver failure in a small percentage of cases. Hepatitis A does not lead to chronic viral hepatitis. We have documented a patient with acute hepatitis A who subsequently went on to develop AIH. Hence diligent follow up of patients with acute hepatitis A needs to be carried out. Hepatitis A may not be, as has long been thought, an acute infection with no long term sequelae.
Footnotes
Competing interests: None.
References
- 1.Vento S, Guella L, Mirandola F.et al Epstein‐Barr virus as a trigger for autoimmune hepatitis in susceptible individuals. Lancet 1995346913. [DOI] [PubMed] [Google Scholar]
- 2.Rahaman S M, Chira P, Koff R S. Idiopathic autoimmune chronic hepatitis triggered by hepatitis A. Am J Gastroenterol 199489106–108. [PubMed] [Google Scholar]