Abstract
Background
Nuclear factor‐κB (NF‐κB) is a key transcriptional regulator of inflammatory bowel disease (IBD).
Aim
To investigate the therapeutic potential of a locally administered “non‐viral” nuclear factor‐κB decoy (NFκBD) in multiple experimental models of IBD.
Methods
A fully phosphorothioated decoy oligonucleotide with improved stability that specifically binds NF‐κB and blocks inflammatory mediators regulated by this transcription factor without the help of viral envelope‐assisted delivery was developed. The therapeutic effects of NFκBD were studied in the trinitrobenzene sulphonic acid, oxazolone and dextran sodium sulphate induced colitis models.
Results
Intracolonic administration of NFκBD results in the delivery of NFκBD to inflammatory cells and a reduction of NF‐κB heterodimers. In the T helper cell 1‐driven trinitrobenzene sulphonic acid‐induced colitis model, mice receiving NFκBD treatment exhibit a dose‐dependent reduction in disease severity and a more rapid recovery to normal body weight, similar to a clinically relevant dose of budesonide. Clinical efficacy was corroborated by considerable reductions in colitis pathology and tissue levels of several pro‐inflammatory markers, including tumour necrosis factor α, interleukin 6, interleukin 1β and monocyte chemotactic protein 1. NFκBD also mitigates disease activity in the T helper cell 2‐like oxazolone colitis and epithelial injury‐related acute dextran sodium sulphate colitis models. Interestingly, restoration of tissue homeostasis is observed in NFκBD‐treated animals with the rapid re‐emergence of functional goblet cells and a return to normal patterns of cell proliferation in the mucosal epithelium and smooth muscle cell layers.
Conclusions
These data support the potential use of “naked” NFκBD as a cross‐functional therapeutic in IBD, and show for the first time that it can facilitate the restoration of colon homeostasis and function.
Inflammatory bowel disease (IBD) encompasses a number of chronic relapsing inflammatory disorders involving the gastrointestinal tract. The two most prevalent forms of IBD, Crohn's disease and ulcerative colitis, can be distinguished by unique histopathologies and immune responses.1,2 The limited efficacy and potential adverse effects of current treatments leave patients and doctors eager for new treatments to manage the chronic relapsing inflammatory nature of these diseases.3,4,5
Although the exact aetiologies leading to Crohn's disease and ulcerative colitis remain unknown, they are generally thought to result from an inappropriate and ongoing activation of the mucosal immune system against the normal luminal flora.6 As a result, resident macrophages, dendritic cells and T cells are activated and begin to secrete predominantly nuclear factor (NF)‐κB‐dependent chemokines and cytokines. NF‐κB‐mediated overproduction of key pro‐inflammatory mediators is attributed to the initiation and progression of both human IBD and animal models of colitis.7,8,9,10,11 In particular, macrophages of patients with IBD exhibit high levels of NF‐κB DNA binding activity accompanied by increased production of interleukin (IL) 1, IL6 and tumour necrosis factor (TNF)α.8 In addition, NF‐κB plays a vital role in activating T helper cell 1 (Th1) and T helper cell 2 (Th2) cytokines, both of which are required for promoting and maintaining inflammation.12 Because of the central role played by NF‐κB in IBD, extensive efforts have been made to develop treatments targeting this pathway.7,13,14,15 Well‐known inhibitors of this pathway are 5‐amino salicylic acid‐related compounds such as sulfasalazine and mesalamine,16,17,18 proteosome inhibitors,19,20 peroxisome proliferator‐activated receptor γ ligands,21,22 signal transduction inhibitors of mitogen‐activated protein kinase23 and Rho kinase,24 TNFα inhibitors25 and steroids.26,27,28 Long‐term side effects, in particular with potent steroids, which often result from off‐target events, tend to limit the usefulness of these compounds as therapeutics in a chronic, relapsing disease such as IBD.
We have developed a fully phosphorothioated nuclear factor‐κB decoy (NFκBD) oligonucleotide (ODN) that specifically binds NF‐κB and blocks the numerous pro‐inflammatory pathways controlled by p65, p50 and c‐Rel‐containing heterodimers. Transcription factor decoys are double‐stranded DNA ODNs that mimic the transcription factor binding sequence and competitively bind to the native transcription factor, thereby preventing its interaction with genomic DNA targets.29,30,31 Subsequently, they inhibit gene activation and, in the event of NF‐κB blockade, result in the suppression of key inflammatory genes critical for immune function and acute‐phase reactions.32,33 The treatment of inflammation with such an NF‐κB‐targeted decoy ODN has shown efficacy in both in vitro studies and in vivo murine inflammation models for a variety of clinical indications.30,34,35,36,37 Recently, this was also shown in IBD models.38 However, these studies relied on viral envelope‐assisted delivery of their decoy ODN.
The data reported here provide direct evidence that a chemically modified, “non‐viral” (or “naked”) NFκBD can be effectively delivered locally to inflamed lesions associated with IBD. In doing so, it is able to reduce disease symptoms and reverse molecular and histological pathology in a dose‐dependent manner in both Crohn's disease and ulcerative colitis‐related mouse models. This study also indicates that topical NFκBD treatment might be more efficacious than other currently available preferred treatments, such as steroids and 5‐amino salicylic acid compounds. Furthermore, the data suggest that this novel molecular treatment approach can promote tissue repair and homeostasis in the inflamed colon.
Materials and methods
Oligonucleotide synthesis
The NFκBD molecule is a 19bp (molecular weight of 13 kDa) double‐stranded DNA comprised of a random mixture of R and S chiral forms of oligonucleotide. The sequence of the NFκBD used in this study was 5′‐AGT TGA GGA CTT TCC AGG C‐3′ (CGTK 153) and 5′‐GCC TGG AAA GTC CTC AAC T‐3′ (CGTK 154). The scrambled ODN sequence was 5′‐CAG TAG TAT GTG AGC CTG C‐3′ (CGTK 103) and 5′‐GCA GGCTCA CAT ACT ACT G‐3′ (CGTK 104). All ODNs used were phosphorothioates and were annealed by combining equal molarities of each strand at room temperature. Concentrations of ODNs were determined by spectrophotometry.
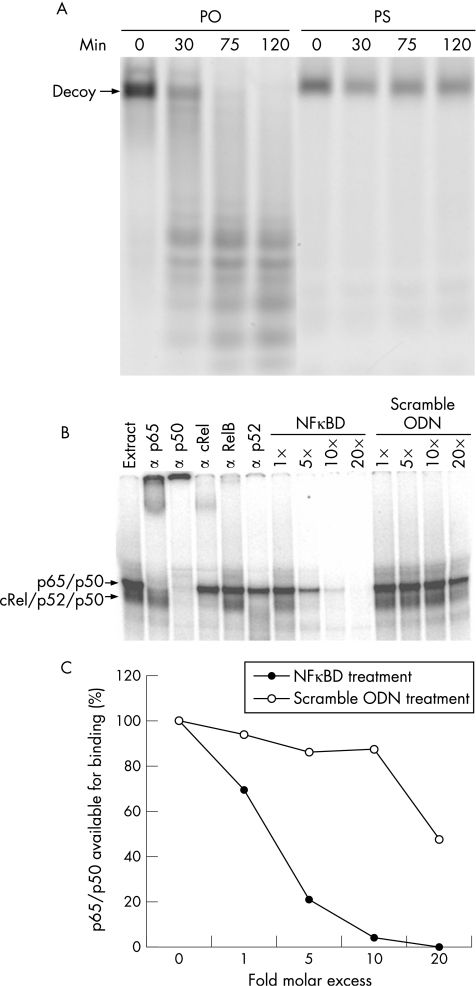
In vitro serum stability assay
Mouse serum (United States Biologicals) was diluted to a final working concentration of 70% using phosphate‐buffered saline. NFκBD containing either a phosphodiester or phosphorothioate backbone was diluted into serum for a final concentration of 4 μmol/l. Gentamycin was included to prevent bacterial growth. The reactions were incubated at 37°C, and 10‐μl aliquots were removed at 0, 30, 75 and 120 min The reactions were stopped by the addition of 1 μl 0.5 M EDTA and were quickly frozen on dry ice. The samples were loaded onto a 20% polyacrylamide gel and subjected to electrophoresis. The gels were imaged and quantified using a Typhoon 8600 Phosphor Imager (Amersham) and Image Quant software.
Electromobility shift assay
The NF‐κB electromobility shift assays (EMSAs) were performed as follows. A double‐stranded ODN containing a consensus NF‐κB binding site from the IL6 promoter (5′ TGT GGG ATT TTC CCA TGA CTC 3′) was end‐labelled with γ32P‐ATP using T4 polynucleotide kinase (Promega). A nuclear extract 1 μg prepared from lipopolysaccharide‐stimulated‐1 cells (human monocyte cell line) was incubated with 35 fmol of radiolabelled probe in the presence or absence of competing unlabelled phosphorothioate NF‐κB double‐stranded ODNs or scrambled ODN. The unlabelled competitors were added at 1, 5, 10 and 20‐fold molar excess over the radiolablled probe and allowed to preincubate for 10 min. The incubations were carried out at room temperature for 30 min in a 20 μl reaction volume composed of 10 mM TRIS‐HCl, pH 8, 100 mM KCl, 5 mM MgCl2, 2 mM dithiothreitol, 10% glycerol, 0.1% NP‐40, 0.025% bovine serum albumin and 1 μg poly‐dIdC (Roche). The reactions were loaded onto an 8% polyacrylamide gel, subjected to electrophoresis and dried. The dried gels were imaged and quantified using a Typhoon 8600 Phosphor Imager (Amersham) and Image Quant software. The identity of the NF‐κB proteins contained in complexes bound to the radiolabelled ODN probe were identified by preincubating the reactions for 10 min with individual antibodies specific for each member of the NF‐κB family before the addition of the radiolabelled probe (all antibodies were purchased from Active Motif (p65 and p50) or Santa Cruz Biotechnology (p52, RelB and, cRel).
Animal models
Animal studies were conducted with the approval and supervision of an animal subjects committee following Institutional Animal Care and Use Committee regulations at Corgentech. All strains of mice were supplied by Jackson Laboratories (Bar Harbor, Maine, USA). Trinitrobenzene sulphonic acid (TNBS) colitis was induced in 5–6‐week‐old male SJL/J mice as described by Fuss et al,39 with the following modifications. A volume of 150 μl of 2.5 mg/ml of TNBS in 45% alcohol was administered by intrarectal catheter. On days 2 and 4 after induction, the animals were treated intrarectally with 150 µl of vehicle, specified dose of NFκBD or scramble ODN, or 0.3 mg/kg budesonide (Sigma, St Louis, Missouri, USA). Changes in body weight were monitored daily and mice were killed after 7–10 days to harvest tissues for histological examination, mRNA isolation and protein extraction.
Oxazolone‐induced colitis was initiated as described by Heller et al40 with C57BL/10 mice with the exception of using 1.5% oxazolone. The mice were treated intrarectally with a single dose of 1.5 or 5 mg/kg NFκBD the day before oxazolone challenge. Body weights were monitored daily and colons were harvested on day 6.
To induce dextran sodium sulphate (DSS) colitis, female BALB/C mice were fed 5% DSS (35–45 kDa; MP Biomedicals) dissolved in drinking water for 10 days. Animals were treated with 2.5 mg/kg NFκBD, scramble ODN or vehicle every other day by intrarectal administration. A Disease Activity Index (DAI) was calculated on day 10 on the basis of the summation of scores evaluating weight loss, blood in stool and stool consistency, as described by Myers et al.41
Histological analysis and confocal microscopy
Harvested colons were formalin‐fixed in a Swiss‐roll orientation, embedded in paraffin wax, sectioned longitudinally and stained with haematoxylin and eosin, and periodic acid–Schiff. The colon sections were scored in a blinded fashion by an independent veterinary pathologist using criteria described previously.42A comprehensive histopathological semiquantitative scoring system was used based on several pathological hallmarks of IBD, including lymphocyte infiltration, changes in mucosal architecture, goblet cell depletion and thickening of the muscularis layer. The immunohistochemical staining was carried out using an Autostainer (Dako, Carpinteria, California, USA) with rabbit monoclonal anti‐Ki67 (LabVision, Freemont, California, USA), peroxidase‐conjugated mouse anti‐smooth muscle actin, EPOS‐SMA (Dako), goat anti‐intestinal trefoil factor (ITF; Santa Cruz Biotechnologies, Santa Cruz, California, USA) and mouse anti‐CD45 (BD Pharmingen, La Jolla, California, USA). The primary antibodies were localised using anti‐rabbit SuperPicture‐HRP reagent (ZYMED, South San Francisco, California, USA), biotinylated anti‐goat IgG, biotinylated anti‐rat IgG and avidin‐biotin complex conjugated to horseradish peroxidase (Vector Laboratories, Burlingame, California, USA). The sections were counterstained with haematoxylin before coverslips were applied.
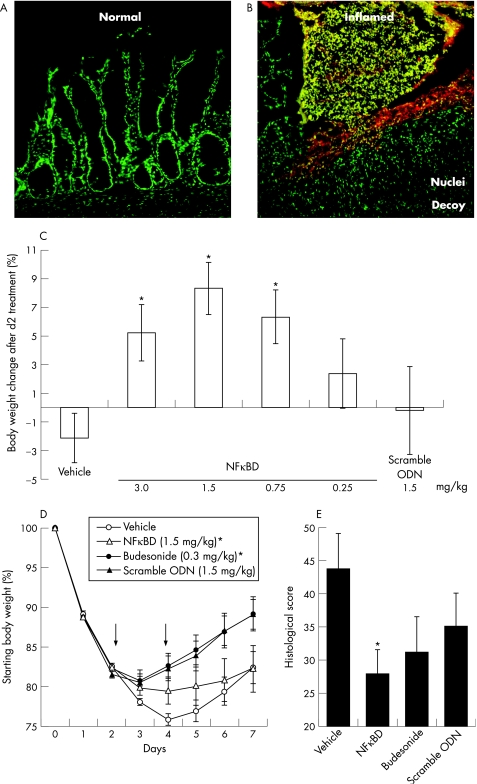
For decoy localisation studies, 6‐carboxy‐2′,4,4′,5′,7,7′‐hexachlorofluorescein‐labelled NFκBD (HEX‐NFκBD) was applied in an enema form in TNBS‐treated mice. The colon harvested after 6 h was embedded and frozen in Tissue‐Tek OCT following formalin fixation and sucrose infiltration steps. Frozen sections were stained with Sytox Green (Molecular Probes, Eugene, Oregon, USA), mounted in glycergel (Dako) and photographed using a Nikon laser scanning confocal microscope (Nikon USA, New Jersey, USA).
NF‐κB TransAM assay
Nuclear extracts prepared from colon tissue were evaluated for transcription factor levels using the NF‐κB TransAM assay (Active Motif; Carlsbad, California, USA) according to the manufacturer's instructions.
Myeloperoxidase assay
To measure myeloperoxidase (MPO) activity, frozen colonic tissue was pulverised and homogenised in tissue‐protein extraction reagent (Pierce; Rockford, Illinois, USA). Homogenates were centrifuged at 16 000 g for 15 min, then MPO activity was measured as described previously.43 Absolute MPO activity was determined on the basis of generation of a standard curve and normalised with protein concentrations as determined by the bicinchoninic acid assay (Pierce).
Cytokine mRNA quantification
Harvested colons were flushed to remove faecal material and flash‐frozen in liquid nitrogen and stored at −80°C. Total RNA was isolated from the colons using Qiazol (Qiagen; Valencia, California, USA). The expression of the mouse genes were assayed by real‐time quantitative polymerase chain reaction (PCR) with an ABI Prism 7900 Sequence Detector System (Applied Biosystems, Foster City, California, USA) using TaqMan PCR reagent kits (Applied Biosystems). Cytokine mRNA levels are expressed relative to ubiquitin mRNA levels.
Statistics
Data are presented as mean (standard error of the mean) values. Statistical significance was determined using Student's unpaired t test for two group analysis and analysis of variance with post hoc comparisons by Dunnett's multiple comparison test for multiple group analysis (GraphPad Software, San Diego, California, USA).
Results
Topical non‐viral NFκBD is effectively delivered to inflamed regions of the colon and efficacious in the TNBS colitis model
A high‐affinity ODN decoy for the NF‐κB transcription factor was designed on the basis of a consensus‐binding sequence. To increase ODN stability, the normal phosphodiester backbone was modified to contain phosphorothioate linkages. In vitro ODN characterisation verified that the NFκBD has improved stability owing to the chemically modified backbone (fig 1A) and binds the proinflammatory NF‐κB heterodimeric complexes in a dose‐and sequence‐specific manner (fig 1B). Intrarectal administration of fluorescent labelled NFκBD (HEX‐NFκBD) in TNBS‐induced colitis mice showed decoy accumulation specifically at sites of inflammation (fig 2A,B). Colocalisation studies with Sytox Green nuclear counterstain showed that HEX‐NFκBD delivered to cells within the inflamed lesions is in fact primarily localised in the cell nuclei after 6 h. We find that topical NFκBD is primarily taken up by neutrophils, macrophages and CD4+ T cells (data not shown).
Figure 1 Nuclear factor‐κB decoy (NFκBD) is resistant to serum nucleases and binds the nuclear factor‐κB (NF‐κB) family of transcription factors. (A) Phosphorothioate (PS) NFκBD is stable to nucleases contained in mouse serum compared with a phosphodiester (PO) counterpart. (B) Competition NF‐κB electromobility shift assays (EMSA) showing the ability of the NFκBD to bind specifically to NF‐κB subunits compared with a scramble phosphorothioated NFκBD oligonucleotide (ODN). Identification of the complexes is shown by antibody supershift. (C) Quantification of NF‐κB EMSA.
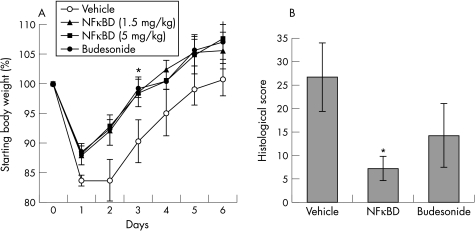
Figure 2 Nuclear factor‐κB decoy (NFκBD) effectively delivered to inflamed regions of the colon is efficacious in the trinitrobenzene sulphonic acid (TNBS) model. Sytox green nuclear counterstaining overlaid with the red hexachlorofluorescein (HEX)‐labelled NFκBD indicates the absence of NFκBD in relatively normal colonic regions (A) and a concentrated localisation in inflamed lesions (B) throughout the colon. (C) Dose–response efficacy in the TNBS colitis model. Values represent mean percentage of body weight change between the day 2 end point and the first day of treatment. (D) Optimal dose of NFκBD (1.5 mg/kg) compared directly with budesonide over 7 days in the TNBS model. Values represent percentage of body weight relative to start of disease induction. Arrows indicates treatment days. Efficacy results are representative of 3–5 independent experiments totalling 30–40 animals per group. (E) Quantitative histopathological scoring of colon sections from TNBS‐induced animals (5–10 animals/group). Data are represented as mean (SEM). * Significant difference compared with saline‐treated group (p<0.05).ODN, phosphorothioated NFκBD oligonucleotide.
To establish the therapeutic efficacy of locally administered NFκBD in IBD, studies were initiated in three different mouse models of acute colitis that show unique features related to human IBD. When mice induced with Th1‐like TNBS colitis were treated with NFκBD on days 2 and 4, a sequence‐dependent and dose‐dependent recovery in body weight was observed compared with vehicle or scramble ODN (p<0.001, n = 30–40 mice/group; fig 2C) treatment. Although significant recovery was observed at doses between 0.75 and 3 mg/kg, maximum efficacy was achieved at 1.5 mg/kg dose, which resulted in an approximately 10% increase in mean body weight at day 7, compared with vehicle control (mean (SEM) 8.3 (1.8) v −2.1 (1.7), respectively; p<0.01). Treatment with 1.5 mg/kg scramble ODN containing a nonspecific sequence resulted in little to no change in the percentage of body weight recovery compared with vehicle control. In a direct comparison with a clinically relevant steroid, budesonide, the 1.5 mg/kg dose of NFκBD was equally effective in reducing TNBS‐induced body weight loss over the entire 7‐day disease course (fig 2D). Gross anatomical assessment of colonic inflammation revealed that colons from 1.5 mg/kg NFκBD‐treated mice show a reversal in the colonic swelling, erythema and stool softening associated with TNBS colitis. In addition, quantification of wet tissue weights indicated a 15–20% reduction in the NFκBD‐treated group compared with vehicle controls (data not shown). More importantly, comprehensive histopathological scoring confirmed a significant therapeutic effect of topical NFκBD treatment (p<0.05, n = 5–10/group; fig 2E). The 1.5 mg/kg NFκBD treatment dose showed a 40% reduction in mean colitis score compared with saline vehicle‐treated controls at the day 7 end point (27.9 (5.9) v 46.8 (4), respectively). We later assessed the amount of drug delivered to the diseased colon using a quantitative pharmacokinetic‐PCR assay. When animals were treated with 1.5 mg/kg NFκBD on day 2, 0.27% of the applied drug was detected 6 h after treatment (420 (90) pg/mg tissue) which was sustained for 24 h (450 (130) pg/mg). A marked decline of the drug concentration was observed at 72 h (40 (10) pg/mg; data not shown).
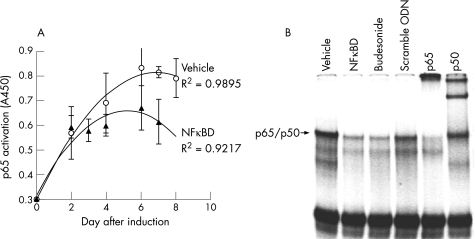
NFκBD reduces key inflammatory mediators in colonic tissue
To verify the targeted blockade of NF‐κB function on NFκBD treatment, colons from TNBS‐induced mice were analysed for tissue NF‐κB levels at various time points after treatment using an ELISA‐based TransAM assay. Binding of p65 in the vehicle‐treated animals increased through day 6, reaching a peak level of 0.82 (0.02) A450 units, and remained increased through day 8 (fig 3A). By contrast, the amount of p65 available for binding was mitigated on treatment with 1.5 mg/kg NFκBD beginning on day 2, and after a second dose at day 4, p65 levels remained substantially lower than vehicle controls through day 7 (0.61 (0.09) A450 units). Reduction in NF‐κB levels at the day 7 timepoint was qualitatively confirmed by gel‐shift assay (fig 3B). Regression analysis of the curve fits for each of these datasets showed the differences in p65 activation to be significant (p = 0.03), thus indicating that a naked phosphorothioated NFκBD is able to significantly reduce levels of this key transcription factor in vivo.
Figure 3 Topical nuclear factor‐κB decoy (NFκBD) treatment reduces the amount of activated nuclear factor‐κB (NF‐κB) in the colon. (A) Colons from trinitrobenzene sulphonic acid (TNBS)‐induced mice were analysed for tissue NF‐κB levels over an 8‐day period using an ELISA‐based TransAm assay. Time course data were graphed with trend line and assessed by regression analysis. (B) Electrophoretic mobility shift assay using 32P‐labelled probe and nuclear extracts prepared from the colons of mice of the indicated treatment groups at the day 7 time point. ODN, phosphorothioated NFκBD oligonucleotide.
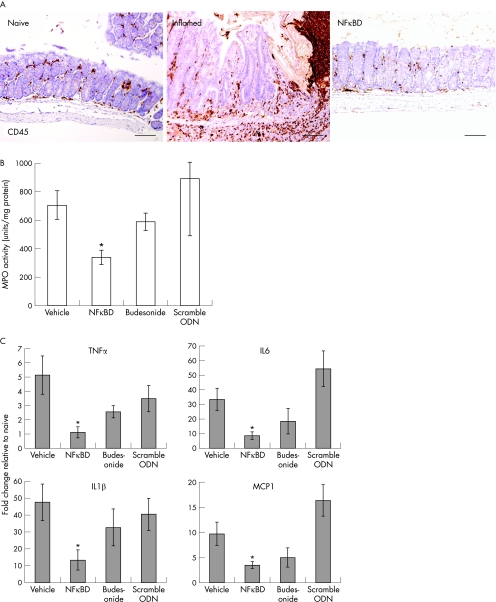
We further tested the inhibition of cellular and molecular activity in the colon of mice treated with 1.5 mg/kg NFκBD on days 2 and 4 after disease induction. Using CD45 as a pan‐leucocyte marker, we evaluated the level of inflammatory cell accumulation by immunohistochemical analysis (fig 4A). Seven days after TNBS‐induced colitis, the amount of inflammatory cell infiltration was clearly reduced in mice treated intrarectally with 1.5 mg/kg NFκBD compared with saline vehicle controls. When colonic MPO activity was measured to assess neutrophil infiltration, a 52% decrease in enzyme activity was observed on day 7 with decoy treatment (n = 5–8/group; p<0.05; fig 4B). The high MPO activity observed in vehicle‐treated colons was not significantly reversed by budesonide or scramble ODN treatment. As determined by real‐time PCR, treatment of NFκBD but not the scrambled ODN resulted in a 2–5‐fold reduction in the mRNA levels of TNFα, IL6 and IL1β and monocyte chemotactic protein (MCP)‐1 (p<0.05, n = 5–8/group; fig 4C) in the tissue harvested on day 7. Interestingly, budesonide treatment had a lower down‐regulatory effect on the transcription of TNFα and IL1β.
Figure 4 Nuclear factor‐κB decoy (NFκBD) reduces key inflammatory mediators in colon tissue. (A) Colons from trinitrobenzene sulphonic acid (TNBS)‐induced mice were evaluated for inflammatory infiltrate levels by immunohistochemical analysis using the pan‐leucocyte CD45 marker. Bars represent 100 μm. (B) Neutrophil infiltration was assessed by measuring myeloperoxidase (MPO) levels in the TNBS‐induced colons. Results are expressed as units of MPO activity/mg protein in colons (5–8 animals/group). (C) Ubiquitin‐normalised mRNA levels of tumour necrosis factor (TNF)α, IL6, IL1β and MCP‐1 from colon tissue in the TNBS model were determined by real‐time polymerase chain reaction analysis. Data are plotted as mean (SEM; n = 5–8 mice/group) from two independent experiments. *Significant difference relative to vehicle control group (p<0.05). ODN, phosphorothioated NFκBD oligonucleotide.
NFκBD treatment promotes restoration of colonic tissue homeostasis
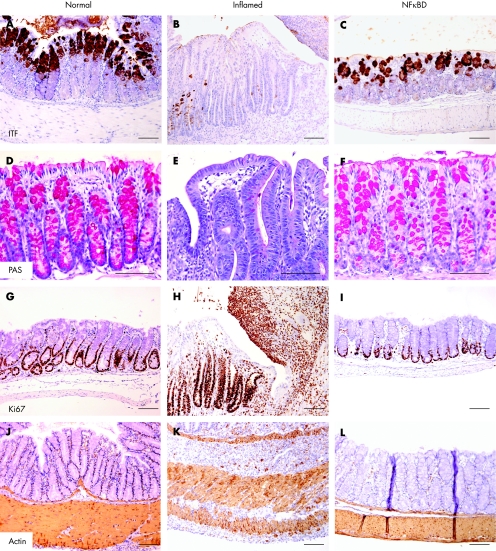
Immunohistochemical assessment of ITF, known to play an essential role in protecting the mucosal epithelium,44 showed low levels of staining in TNBS‐inflamed colons compared with normal colons (fig 5Bv A). After two treatments of 1.5 mg/kg NFκBD, the production of ITF by goblet cells was pronounced in the mucosal epithelium at day 7 after TNBS induction (fig 5C). Re‐emergence of secretory granules from goblet cells is evident in the haematoxylin and eosin‐stained sections from mice treated with NFκBD, and the ability of these highly differentiated cells to produce mucopolysaccharides was determined by peroidic acid‐Schiff staining of colonic tissues (fig 5D–F). The colons from mice treated with NFκBD showed a dramatic increase in the levels of mucopolysaccharide production in the tissue compared with saline controls.
Figure 5 Nuclear factor‐κB decoy (NFκBD) treatment restores tissue homeostasis in the trinitrobenzene sulphonic acid (TNBS) model. Representative sections of intestinal trefoil factor (ITF), mucopolysaccharide, Ki‐67 and smooth muscle actin staining in the colon from normal colons (A, D, G, J), vehicle‐treated (B, E, H, K) and 1.5 mg/kg NFκBD‐treated (C, F, I, L) mice 7 days after induction of TNBS colitis. Bars represent 100 μm. PAS, peroidic acid–Schiff.
To assess changes in cell proliferation due to NFκBD treatment, colons from TNBS‐induced mice were stained for Ki‐67 (fig 5G–I). Increased proliferation was observed in the mucosal epithelium lining the crypts and throughout the lamina propria and muscularis layers of inflamed colons (fig 5H). NFκBD‐treated mice have a restricted cell proliferation pattern in the base of the crypts, as seen in the normal mucosa (fig 5I). In addition, although inflamed colons showed greatly disrupted actin patterns associated with increased intercellular space, the muscularis of NFκBD‐treated mice was uniform and well compacted (fig 5J–L). Collectively, these findings support the ability of NFκBD to help in the repair of damaged intestinal epithelium and restore colon function in IBD.
NFκBD reverses disease activity in the oxazolone and DSS colitis models
Mice treated with NFκBD or budesonide were less affected by the oxazolone challenge and began recovering body weight by day 2, whereas the vehicle group remained unresponsive (fig 6A). A significant difference between treated and vehicle groups was observed at day 3, at which point the NFκBD‐treated and budesonide‐treated groups had returned to their approximate starting weights, whereas the vehicle group was still down 12% from its original mean weight (p<0.01, n = 25–35 mice/group). Histological assessment indicated a >70% reduction in the level of colitic damage between NFκBD‐treated and vehicle‐treated controls (7.2 (2.6) v 26.7 (7.3), respectively) at day 6 (n = 5/group; fig 6B). Animals receiving NFκBD treatment showed even greater improvement than those given budesonide in most of the pathological parameters evaluated, including mucoid crypt cysts and abscesses, goblet cell depletion, oedema, mononuclear cell infiltration and transmural inflammation.
Figure 6 Nuclear factor‐κB decoy (NFκBD) reverses disease activity in the oxazolone‐induced colitis model. (A) Mean percentage of body weight of three independent experiments in the oxazolone colitis model (n = 25–35 mice/group). (B) Quantification of histological colitis scores in the oxazolone model. Bars represent the mean (SEM; n = 5/group). *Significant difference relative to the vehicle control group (p<0.05).
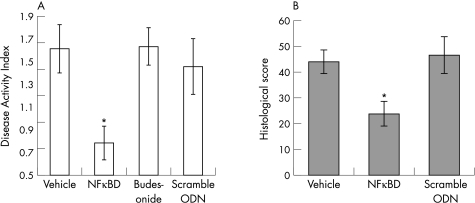
In the acute DSS model, animals receiving vehicle only or scramble ODN control treatment achieved mean (SEM) DAI scores of 1.6 (0.2) and 1.5 (0.3), respectively (fig 7A). Remarkably, the DAI was reduced over 50% in the NFκBD treatment group compared with vehicle and scramble controls, reaching a significant value of 0.78 (0.2; n = 15–25 mice/group; p<0.05). Surprisingly, we found the steroid treatment to be ineffective, in some cases even exacerbating in this model (data not shown). At the histological level, NFκBD‐treated colons had significantly reduced histopathological scores, decreased over 55% compared with vehicle controls (21.5 (5) v 47.9 (5.6), respectively; n = 6–14/group; fig 7B). The amelioration of disease in the oxazolone‐and DSS‐induced colitis models confirms the therapeutic potential of NFκBD in a mixed Th1/Th2‐mediated disease.
Figure 7 nuclear factor‐κB decoy (NFκBD), reverses disease activity in an acute dextran sodium sulphate (DSS), colitis model. (A) Mean Disease Activity Index (DAI) at day 10 in the acute DSS model. Data represent mean (SEM; n = 15–25 mice/group) from three independent experiments. (B) Histological colitis scores from the acute DSS model. Bars represent the mean (SEM; n = 6–14/group). *Significant difference relative to the vehicle control group (p<0.05).
Discussion
In this study, we showed that local, non‐viral administration of NFκBD ameliorates colitis‐related disease activity in several well‐established mouse models of IBD. Firstly, intracolonic administration of NFκBD is delivered to sites of inflammation. Secondly, NFκBD is efficacious in Th1‐mediated and Th2‐mediated colitis. Thirdly, treatment reduces the level of NF‐κB and decreases the expression of pro‐inflammatory cytokines. Fourthly, NFκBD treatment promotes healing of colonic tissue and restores goblet cell function. Finally, NFκBD treatment shows efficacy comparable with the clinically available steroid budesonide.
The role of NF‐κB as a rate‐limiting step in the inflammatory cascade has made it an attractive target for drug treatment.2 Earlier studies with NF‐κB antisense oligonucleotide7 and the recent report by Fichtner‐Feigl et al38 using an NF‐κBD delivered with a viral envelope have shown efficacy in animal models of IBD. However, viral‐assisted delivery may not be a viable clinical option in humans because of potential immunogenic challenges after repeated exposure in a target population that requires multiple treatments. Here, we showed that phosphorothioated NFκBD was effectively delivered to sites of inflammation in the TNBS colitis model without assisted delivery, probably because of the improved stability and chemistry of the decoy, which allows sufficient time for the uptake of intact drug by inflammatory cells. In the skin, immunohistological analysis with fluorescently labelled decoy showed an uptake of NF‐κBD by several key inflammatory cells. The colocalisation of NF‐κBD was detected in langerin‐positive, resident antigen‐presenting cells and antigen‐presenting Langerhans cells, CD117‐positive mast cells, CD4 T cells and MCP1‐positive macrophages.45 Moreover, NF‐κBD treatment in the skin led to induction of apoptosis which may help regulate many of these key immune cells. The phosphorothioate chemistry has been used successfully with antisense therapeutics and has proved effective for several antisense molecules aimed specifically at colonic delivery,7,41,46 including intracellular adhesion molecule (ICAM)‐1 antisense (Alicaforsen), which is currently in phase II clinical trials for ulcerative colitis.47
In this study, we have shown the efficacy of NFκB in mouse colitis models representative of both Th1‐and Th2‐mediated immune responses. TNFα, IL1β, IL6 and MCP1 are strongly expressed in the colon mucosa during inflammation and are directly regulated by NF‐κB.48,49 Unlike previous studies that assessed cytokine levels in restimulated cells in vitro, we showed the ability of NFκBD treatment to reduce these key inflammatory mediators in inflamed tissue. Moreover, we show that NFκBD treatment reduces myeloperoxidase activity, which is an important factor for measuring neutrophil infiltration during colonic inflammation. On the basis of spectrum of cell types producing and being affected by these inflammatory mediators, we show a broad cellular and molecular effect with our NFκBD on the inflammatory response during this multifactorial disease. Taken together, our data support the therapeutic potential of topical NFκBD as a cross‐functional drug in both Crohn's disease and ulcerative colitis using a clinically feasible non‐viral mode of delivery.
Although resolution of the inflammatory process invoked in IBD is an important first step in reversing disease, tissue repair and regeneration are also critical for re‐establishing normal colon function. In looking at several different indicators of restitution and regeneration in the colon, we found that treatment with our NFκBD had positive effects on the restoration process. Trefoil factors are known to play an integral part in the restitution process for mucosal integrity and are functionally important in IBD.44,50 We found that NFκBD treatment leads to increased expression of ITF, which is accompanied by a reduction in the number of lesions in NFκBD‐treated colons. Moreover, the return of fully differentiated goblet cells producing high amounts of mucopolysaccharides, as evidenced by Alcian blue‐stained colonic sections, further supports the notion that NFκBD treatment leads to the regeneration of normal mucosal function and may help in the protection of disease relapse. The restricted expression of the Ki‐67 proliferation marker to the base of the mucosal crypts, and dense actin staining in the muscle layer of NFκBD‐treated mice, indicates a resolution of disease in the submucosa that may help the recovery of additional colon functions, such as alleviating the disrupted intestinal motility associated with IBD.
To directly assess the potential clinical utility of NFκBD, we evaluated its efficacy with existing treatment options. In comparison with the clinically used steroid, budesonide, we found NFκBD to be comparable if not better in the models tested in this study. Oligonucleotide‐based therapeutics are beginning to make their way into the clinic and further support the utility of this emerging drug class. We believe that direct targeting of NFκBD would provide a better therapeutic approach than going after individual factors such as ICAM‐1, TNFα, IL12. Expression of ICAM‐1, for example, is regulated by NF‐κB and therefore represents a downstream target, among many other important inflammatory mediators, that would be inhibited by NFκBD.51 Taking a therapeutic approach that interferes with a central player in inflammation, such as NF‐κB, could be more effective for long‐term treatment in a multifactorial chronic disease such as IBD. Antisense ODNs specifically targeting the p65 subunit of NF‐κB have also shown therapeutic efficacy in animal models of IBD7,14; however, NF‐κB transactivation is not entirely due to any specific NF‐κB family member. c‐Rel, for example, is essential for Th1‐cell differentiation,52 IL12 production in macrophages53 and the excessive Th1 response observed in nucleotide‐binding oligomerisation domain 2‐deficient mice.54 The advantage of the consensus binding sequence in our NFκBD allows for inhibition of binding and transcriptional activity for several major components of the NF‐κB family. Together, our data suggest that non‐viral NFκBD may be as or more effective with fewer side effects than current therapeutics in treating both Crohn's disease and ulcerative colitis, and capable of restoring mucosal integrity and function.
Acknowledgements
We thank Wanda Williamson and the animal care staff for their diligent maintenance of the mouse colonies, Dr Helle Bielefeldt‐Ohmann for histological scoring and Dr Tom Twaddell for his critical review of the manuscript.
Abbreviations
DAI - Disease Activity Index
DSS - dextran sodium sulphate
EMSAs - electromobility shift assays
HEX - hexachlorofluorescein
IBD - inflammatory bowel disease
ICAM - intercellular adhesion molecule
ITF - intestinal trefoil factor
MCP - monocyte chemotactic protein
MPO - myeloperoxidase
NF‐κB - nuclear factor‐κB
NFκBD - nuclear factor‐κB decoy
ODN - phosphorothioated NFκBD oligonucleotide
PCR - polymerase chain rection
Th1 - T helper cell 1
Th2 - T helper cell 2
TNBS - trinitrobenzene sulphonic acid
Footnotes
Competing interests: None.
References
- 1.Bouma G, Strober W. The immunological and genetic basis of inflammatory bowel disease. Nat Rev Immunol 20033521–533. [DOI] [PubMed] [Google Scholar]
- 2.Podolsky D K. Inflammatory bowel disease. N Engl J Med 2002347417–429. [DOI] [PubMed] [Google Scholar]
- 3.Hanauer S B, Present D H. The state of the art in the management of inflammatory bowel disease. Rev Gastroenterol Disord 2003381–92. [PubMed] [Google Scholar]
- 4.Hibi T, Inoue N, Ogata H.et al Introduction and overview: recent advances in the immunotherapy of inflammatory bowel disease. J Gastroenterol 200338(Suppl 15)36–42. [PubMed] [Google Scholar]
- 5.Podolsky D K. The future of IBD treatment. J Gastroenterol 200338(Suppl 15)63–66. [PubMed] [Google Scholar]
- 6.Fiocchi C. Inflammatory bowel disease: etiology and pathogenesis. Gastroenterology 1998115182–205. [DOI] [PubMed] [Google Scholar]
- 7.Neurath M F, Pettersson S, Meyer zum Buschenfelde K H.et al Local administration of antisense phosphorothioate oligonucleotides to the p65 subunit of NF‐kappa B abrogates established experimental colitis in mice. Nat Med 19962998–1004. [DOI] [PubMed] [Google Scholar]
- 8.Neurath M F, Fuss I, Schurmann G.et al Cytokine gene transcription by NF‐kappa B family members in patients with inflammatory bowel disease. Ann N Y Acad Sci 1998859149–159. [DOI] [PubMed] [Google Scholar]
- 9.Schreiber S, Nikolaus S, Hampe J. Activation of nuclear factor kappa B inflammatory bowel disease. Gut 199842477–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spiik A K, Ridderstad A, Axelsson L G.et al Abrogated lymphocyte infiltration and lowered CD14 in dextran sulfate induced colitis in mice treated with p65 antisense oligonucleotides. Int J Colorectal Dis 200217223–232. [DOI] [PubMed] [Google Scholar]
- 11.Dubuquoy L, Jansson E A, Deeb S.et al Impaired expression of peroxisome proliferator‐activated receptor gamma in ulcerative colitis. Gastroenterology 20031241265–1276. [DOI] [PubMed] [Google Scholar]
- 12.Barnes P J, Karin M. Nuclear factor‐kappaB: a pivotal transcription factor in chronic inflammatory diseases. N Engl J Med 19973361066–1071. [DOI] [PubMed] [Google Scholar]
- 13.Wrighton C J, Hofer‐Warbinek R, Moll T.et al Inhibition of endothelial cell activation by adenovirus‐mediated expression of I kappa B alpha, an inhibitor of the transcription factor NF‐kappa B. J Exp Med 19961831013–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murano M, Maemura K, Hirata I.et al Therapeutic effect of intracolonically administered nuclear factor kappa B (p65) antisense oligonucleotide on mouse dextran sulphate sodium (DSS)‐induced colitis. Clin Exp Immunol 200012051–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karin M, Yamamoto Y, Wang Q M. The IKK NF‐kappa B system: a treasure trove for drug development. Nat Rev Drug Discov 2004317–26. [DOI] [PubMed] [Google Scholar]
- 16.Yan F, Polk D B. Aminosalicylic acid inhibits IkappaB kinase alpha phosphorylation of IkappaBalpha in mouse intestinal epithelial cells. J Biol Chem 199927436631–36636. [DOI] [PubMed] [Google Scholar]
- 17.Kaiser G C, Yan F, Polk D B. Mesalamine blocks tumor necrosis factor growth inhibition and nuclear factor kappaB activation in mouse colonocytes. Gastroenterology 1999116602–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wahl C, Liptay S, Adler G.et al Sulfasalazine: a potent and specific inhibitor of nuclear factor kappa B. J Clin Invest 19981011163–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alkalay I, Yaron A, Hatzubai A.et al Stimulation‐dependent I kappa B alpha phosphorylation marks the NF‐kappa B inhibitor for degradation via the ubiquitin‐proteasome pathway. Proc Natl Acad Sci U S A 19959210599–10603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elliott P J, Zollner T M, Boehncke W H. Proteasome inhibition: a new anti‐inflammatory strategy. J Mol Med 200381235–245. [DOI] [PubMed] [Google Scholar]
- 21.Ricote M, Li A C, Willson T M.et al The peroxisome proliferator‐activated receptor‐gamma is a negative regulator of macrophage activation. Nature 199839179–82. [DOI] [PubMed] [Google Scholar]
- 22.Su C G, Wen X, Bailey S T.et al A novel therapy for colitis utilizing PPAR‐gamma ligands to inhibit the epithelial inflammatory response. J Clin Invest 1999104383–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hollenbach E, Neumann M, Vieth M.et al Inhibition of p38 MAP kinase‐ and RICK/NF‐kappaB‐signaling suppresses inflammatory bowel disease. FASEB J 2004181550–1552. [DOI] [PubMed] [Google Scholar]
- 24.Segain J P, Raingeard de la Bletiere D, Sauzeau V.et al Rho kinase blockade prevents inflammation via nuclear factor kappa B inhibition: evidence in Crohn's disease and experimental colitis. Gastroenterology 20031241180–1187. [DOI] [PubMed] [Google Scholar]
- 25.Pimentel‐Muinos F X, Mazana J, Fresno M. Biphasic control of nuclear factor‐kappa B activation by the T cell receptor complex: role of tumor necrosis factor alpha. Eur J Immunol 199525179–186. [DOI] [PubMed] [Google Scholar]
- 26.Ardite E, Panes J, Miranda M.et al Effects of steroid treatment on activation of nuclear factor kappaB in patients with inflammatory bowel disease. Br J Pharmacol 1998124431–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Auphan N, DiDonato J A, Rosette C.et al Immunosuppression by glucocorticoids: inhibition of NF‐kappa B activity through induction of I kappa B synthesis. Science 1995270286–290. [DOI] [PubMed] [Google Scholar]
- 28.Scheinman R I, Cogswell P C, Lofquist A K.et al Role of transcriptional activation of I kappa B alpha in mediation of immunosuppression by glucocorticoids. Science 1995270283–286. [DOI] [PubMed] [Google Scholar]
- 29.Dzau V J, Mann M J, Morishita R.et al Fusigenic viral liposome for gene therapy in cardiovascular diseases. Proc Natl Acad Sci USA 19969311421–11425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morishita R, Sugimoto T, Aoki M.et al In vivo transfection of cis element “decoy” against nuclear factor‐kappaB binding site prevents myocardial infarction. Nat Med 19973894–899. [DOI] [PubMed] [Google Scholar]
- 31.Nakamura H, Morishita R, Kaneda Y. Molecular therapy via transcriptional regulation with double‐stranded oligodeoxynucleotides as decoys. In Vivo 20021645–48. [PubMed] [Google Scholar]
- 32.Finco T S, Baldwin A S. Mechanistic aspects of NF‐kappa B regulation: the emerging role of phosphorylation and proteolysis. Immunity 19953263–272. [DOI] [PubMed] [Google Scholar]
- 33.Lenardo M J, Baltimore D. NF‐kappa B: a pleiotropic mediator of inducible and tissue‐specific gene control. Cell 198958227–229. [DOI] [PubMed] [Google Scholar]
- 34.Cao C C, Ding X Q, Ou Z L.et al In vivo transfection of NF‐kappaB decoy oligodeoxynucleotides attenuate renal ischemia/reperfusion injury in rats. Kidney Int 200465834–845. [DOI] [PubMed] [Google Scholar]
- 35.Desmet C, Gosset P, Pajak B.et al Selective blockade of NF‐kappa B activity in airway immune cells inhibits the effector phase of experimental asthma. J Immunol 20041735766–5775. [DOI] [PubMed] [Google Scholar]
- 36.Nakamura H, Aoki M, Tamai K.et al Prevention and regression of atopic dermatitis by ointment containing NF‐kB decoy oligodeoxynucleotides in NC/Nga atopic mouse model. Gene Ther 200291221–1229. [DOI] [PubMed] [Google Scholar]
- 37.Tomita T, Takeuchi E, Tomita N.et al Suppressed severity of collagen‐induced arthritis by in vivo transfection of nuclear factor kappaB decoy oligodeoxynucleotides as a gene therapy. Arthritis Rheum 1999422532–2542. [DOI] [PubMed] [Google Scholar]
- 38.Fichtner‐Feigl S, Fuss I J, Preiss J C.et al Treatment of murine Th1‐ and Th2‐mediated inflammatory bowel disease with NF‐kappaB decoy oligonucleotides. J Clin Invest 20051153057–3071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fuss I J, Marth T, Neurath M F.et al Anti‐interleukin 12 treatment regulates apoptosis of Th1 T cells in experimental colitis in mice. Gastroenterology 19991171078–1088. [DOI] [PubMed] [Google Scholar]
- 40.Heller F, Fuss I J, Nieuwenhuis E E.et al Oxazolone colitis, a Th2 colitis model resembling ulcerative colitis, is mediated by IL‐13‐producing NK‐T cells. Immunity 200217629–638. [DOI] [PubMed] [Google Scholar]
- 41.Myers K J, Murthy S, Flanigan A.et al Antisense oligonucleotide blockade of tumor necrosis factor‐alpha in two murine models of colitis. J Pharmacol Exp Ther 2003304411–424. [DOI] [PubMed] [Google Scholar]
- 42.Fort M M, Mozaffarian A, Stover A G.et al A synthetic TLR4 antagonist has anti‐inflammatory effects in two murine models of inflammatory bowel disease. J Immunol 20051746416–6423. [DOI] [PubMed] [Google Scholar]
- 43.Bradley P P, Priebat D A, Christensen R D.et al Measurement of cutaneous inflammation: estimation of neutrophil content with an enzyme marker. J Invest Dermatol 198278206–209. [DOI] [PubMed] [Google Scholar]
- 44.Taupin D, Podolsky D K. Trefoil factors: initiators of mucosal healing. Nat Rev Mol Cell Biol 20034721–732. [DOI] [PubMed] [Google Scholar]
- 45.Dajee M, Muchamuel T, Schryver B.et al Blockade of experimental atopic dermatitis via topical NF‐kB decoy oligonucleotide. J Invest Dermatol 20061261792–1803. [DOI] [PubMed] [Google Scholar]
- 46.Bennett C F, Kornbrust D, Henry S.et al An ICAM‐1 antisense oligonucleotide prevents and reverses dextran sulfate sodium‐induced colitis in mice. J Pharmacol Exp Ther 1997280988–1000. [PubMed] [Google Scholar]
- 47.van Deventer S J, Tami J A, Wedel M K. A randomised, controlled, double blind, escalating dose study of alicaforsen enema in active ulcerative colitis. Gut 2004531646–1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reinecker H C, Steffen M, Witthoeft T.et al Enhanced secretion of tumour necrosis factor‐alpha, IL‐6, and IL‐1 beta by isolated lamina propria mononuclear cells from patients with ulcerative colitis and Crohn's disease. Clin Exp Immunol 199394174–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stevens C, Walz G, Singaram C.et al Tumor necrosis factor‐alpha, interleukin‐1 beta, and interleukin‐6 expression in inflammatory bowel disease. Dig Dis Sci 199237818–826. [DOI] [PubMed] [Google Scholar]
- 50.Wright N A, Poulsom R, Stamp G.et al Trefoil peptide gene expression in gastrointestinal epithelial cells in inflammatory bowel disease. Gastroenterology 199310412–20. [DOI] [PubMed] [Google Scholar]
- 51.Manning A M, Bell F P, Rosenbloom C L.et al NF‐kappa B is activated during acute inflammation in vivo in association with elevated endothelial cell adhesion molecule gene expression and leukocyte recruitment. J Inflamm 199545283–296. [PubMed] [Google Scholar]
- 52.Hilliard B A, Mason N, Xu L.et al Critical roles of c‐Rel in autoimmune inflammation and helper T cell differentiation. J Clin Invest 2002110843–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sanjabi S, Hoffmann A, Liou H C.et al Selective requirement for c‐Rel during IL‐12 P40 gene induction in macrophages. Proc Natl Acad Sci USA 20009712705–12710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Watanabe T, Kitani A, Murray P J.et al NOD2 is a negative regulator of Toll‐like receptor 2‐mediated T helper type 1 responses. Nat Immunol 20045800–808. [DOI] [PubMed] [Google Scholar]