Abstract
Aim
To examine the range of monocular crowded logMAR acuity and cycloplegic refraction of children aged 3 years and 4 years without strabismus.
Methods
Data were collected prospectively. All children had full orthoptic and ophthalmic examination. Inclusion principally required the absence of strabismus, symptoms, and ocular pathology. Criteria were used to categorise the refraction findings as normal, borderline, or abnormal.
Results
118 children aged 3 years (mean 3 years 6 months (SD 2 months) and 67 children aged 4 years (mean 4 years 4 months (SD 3 months) fulfilled the inclusion criteria. For the children with normal refraction, the mean monocular logMAR acuity was 0.200 (SD 0.09) for 3 year olds (n = 84) and 0.140 (SD 0.08) for 4 year olds (n = 45); the mean interocular acuity difference (IAD) was 0.03 (SD 0.06) for 3 year olds and 0.03 (SD 0.04) for 4 year olds. The 95% confidence limits were calculated for monocular acuity and IAD and compared to the acuity scores of the children with borderline (n = 17) and abnormal refractive error (n = 38). 15 borderline and 16 abnormal cases had a visual acuity within these limits.
Conclusion
A wide range of refraction may be associated with a good level of visual acuity in children aged 3 years and 4 years.
Keywords: visual acuity, refractive error, strabismus, logMAR vision
It is agreed that a constant or intermittent strabismus or poorly controlled heterophoria are abnormal and treatment is required. The need for treatment for the asymptomatic child with no strabismus is not clearcut. The age emmetropia is reached is uncertain,1,2,3 the effect of spectacle wear on emmetropisation is unresolved,4,5,6,7 the degree of refractive error that requires correction in the non‐squinting child is “ill defined”8 and an overprescription of glasses for children has been reported.9
The aim of spectacle correction is primarily to treat and prevent amblyopia but how can the clinician be sure amblyopia is present? A child's acuity can be difficult to interpret because of many factors such as age, ability, and attention. Frequently, young children with visual acuity less than 6/6 are given spectacles for a small degree of refractive error because the acuity is considered to be subnormal. However, as the percentage of children reported to have achieved a 6/6 level of linear vision is low, being 42%1 and 40%10 for children aged 6 years, it seems likely that acuity less than 6/6 may be “normal” for young children; but how much less than 6/6 is normal?
Our aim was to examine the range of monocular crowded logMAR acuity and cycloplegic refraction of children, aged 3 years and 4 years, without strabismus.
Methods
Data were collected prospectively for children aged 3 years and 4 years who presented as new referrals to the orthoptic clinic. All had full orthoptic and ophthalmic evaluation. All vision assessments were obtained using the Keeler crowded logMAR test.11 The order of eye tested was random. Cycloplegic refraction, fundus, and media examination were performed a minimum of 40 minutes after instillation of one drop of cyclopentolate 1% into each eye. Data were analysed for those children who fulfilled the following inclusion criteria:
Normal eye alignment—that is, no constant, intermittent, or micro manifest strabismus; no heterophoria of >8 prism dioptres
Ocular motility within normal limits
Normal response to 20 dioptre prism test
Monocular acuity obtained each eye using Keeler crowded logMAR test
Foveal fixation of each eye determined using the visuscope
Normal fundus and media
No history of treatment for refractive error, strabismus or ocular abnormality, and no symptoms
Neurologically and developmentally normal.
A child was categorised as having a normal, borderline, or abnormal refraction,8,12,13,14,15 (see table 1). Refraction values reported are full cycloplegic amounts with allowance for working distance removed. All vision values reported are uncorrected acuity.
Table 1 Refractive criteria based on the literature.
| Refractive error | Normal refraction | Borderline refractive error | Abnormal refractive error |
|---|---|---|---|
| Hypermetropia | <+3.00 DS | +3.00 to < +4.00 DS | ⩾+4.00 |
| Myopia | <−1.00 DS | −1.00 to −2.00 DS | >−2.00 DS |
| Astigmatism | <−1.00 DC | −1.00 to <1.50 DC | ⩾−1.50 DC |
| Anisometropia | <1.00 DS/DC | <1.00 DS/DC | ⩾1.00 DS/DC |
Clinically cylinder errors are recorded in minus cylinder form, hence the cylinder criteria are in minus values. A child's refraction was categorised on the basis of the eye with the greatest error—for example, right +3.50/−1.00, left +3.50/−1.50 would be categorised as an abnormal refractive error on the basis of the left eye.
Results
A total of 185 children fulfilled the inclusion criteria. Of these, 118 were aged 3 years (mean 3 years 6 months (SD 2 months)); 51 were male and 67 female. The remaining 67 children were aged 4 years (mean 4 years 4 months (SD 3 months)); 37 were male and 30 female.
Frequency distribution
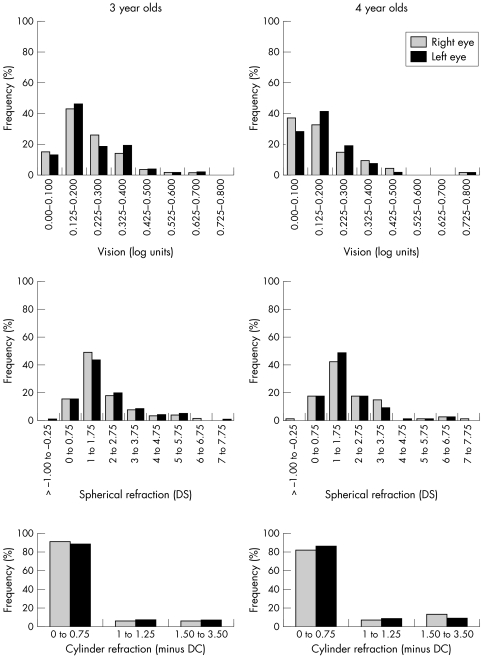
The distribution for vision and refraction for right and left eyes of the 3 year old and 4 year old children is shown in figure 1. For both age groups data were skewed to better acuity and lower spherical and cylinder refraction values.
Figure 1 Frequency distribution of vision scores in log units scored by line (top row), spherical refraction (middle row), and cylinder refraction (bottom row), for the right eye (shaded) and left eye (solid) of all 3 year old (left column) and 4 year old (right column) children who fulfilled the inclusion criteria. All vision scores are uncorrected acuity. Refraction values shown are for full cycloplegic refraction with allowance for working distance removed. Cylinder values were recorded in minus form. (Snellen equivalents values: 0.00 = 6/6; 0.100 = 6/7.5; 0.200 = 6/9; 0.300 = 6/12; 0.400 = 6/15; 0.500 = 6/19; 0.600 = 6/24; 0.700 = 6/30; 0.800 = 6/38.)
Comparison of vision and refraction score for individuals
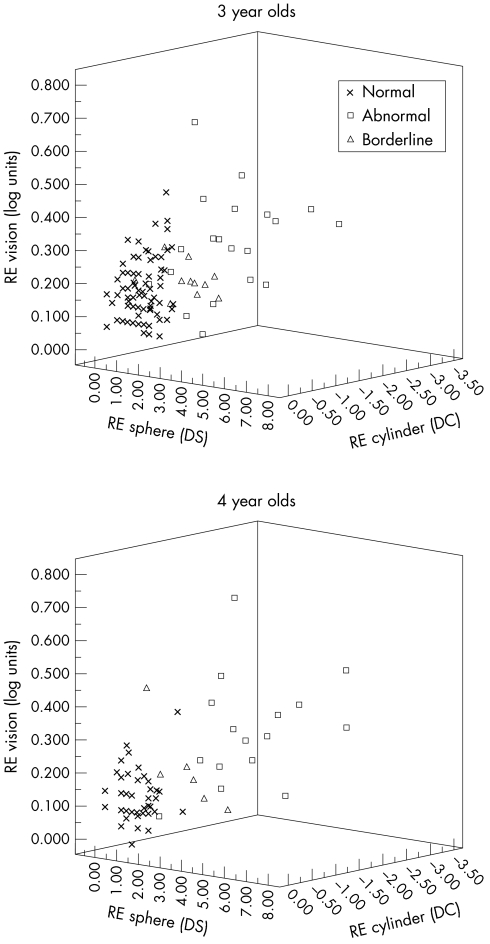
Figure 2 shows a three dimensional plot of spherical and cylinder refraction against visual acuity for right eye data in the refractive categories of normal, borderline and abnormal for the two age groups. For both groups there was a wide range of vision score associated with a given spherical/cylinder refraction.
Figure 2 A three dimensional plot of spherical and cylinder refraction against visual acuity for right eye data of the 3 year old (top) and 4 year old children (bottom). Data are shown in the refractive categories of normal, borderline, and abnormal. A child's refraction was categorised on the basis of the eye with the greatest error. All vision scores are uncorrected acuity. Refraction values shown are for full cycloplegic refraction with allowance for working distance removed.
Monocular acuity associated with a normal refraction
A summary of the analysis of the acuity data of children categorised as having a normal refraction is shown in table 2.
Table 2 Mean, standard deviation (SD), and 95% confidence limits (mean (SD 2.00) for right and left eye visual acuity and interocular difference (IAD) for children categorised as having a normal refraction.
| Analysis | 3 year olds (n = 84) | 4 year olds (n = 45) | ||
|---|---|---|---|---|
| Right eye | Left eye | Right eye | Left eye | |
| Mean acuity (SD) | 0.200 (0.09) | 0.200 (0.08) | 0.140 (0.08) | 0.144 (0.07) |
| Median acuity | 0.180 | 0.200 | 0.100 | 0.125 |
| 95% confidence limits | 0.020 to 0.380 | 0.040 to 0.360 | −0.02 to 0.300 | 0.004 to 0.284 |
| Percentiles limits | 0.075 to 0.400 | 0.078 to 0.400 | 0.008 to 0.325 | 0.000 to 0.300 |
| Mean IAD (SD) | 0.03 (0.06) | 0.03 (0.04) | ||
| Median IAD | 0.00 | 0.025 | ||
| 95% confidence limits IAD | −0.09 to 0.150 | −0.05 to 0.110 | ||
| Percentiles limits IAD | 0.00 to 0.262 | 0.000 to 0.167 | ||
As the data were not normally distributed the median value and percentile limits (2.5th to 97.5th percentile) are also presented.
For each eye the mean and median acuity differed by less than one letter (0.025) for 3 year olds (n = 84), and less than two letters for 4 year olds (n = 45). With the exception of the left eye data of the 3 year olds, the upper limits of monocular acuity differed by one letter or less.
The IAD associated with a normal refraction
There was no significant difference between right and left eye acuity of individuals (3 year olds p = 0.385, 4 year olds p = 0.761, Wilcoxon signed rank test). The median, mean, and limits of the IAD are shown in table 2. Mean and median values were in agreement, but percentiles produced a higher upper limit for both age groups.
Application of the acuity limits calculated on the basis of a normal refraction
If we accept that the acuity limits calculated above represent a normal variant of visual acuity for children aged 3 years and 4 years who have a normal refraction, then a subnormal acuity would be a one scale increment (that is, one letter value 0.025) or more above the upper limit. Using the 95% confidence limits this would be ⩾0.400 for 3 year olds and ⩾0.325 for 4 year olds for monocular acuity, and ⩾0.175 for 3 year olds and ⩾0.150 for 4 year olds for IAD.
Comparison of the monocular acuity and IAD 95% confidence limits with borderline refraction (3 year olds, n = 11; 4 year olds, n = 6)
Fifteen children with borderline refractive error had visual acuity well within the monocular and IAD limits. One child had an IAD of 0.200, no anisometropia, and at retest acuity was 0.100 right and left. One child had borderline myopic astigmatism, reduced acuity at retest and to date is the only child with borderline refraction to have spectacles prescribed.
Comparison of the monocular acuity and IAD 95% confidence limits with abnormal refraction (3 year olds, n = 22; 4 year olds, n = 16)
Sixteen children with abnormal refractive error had visual acuity within the limits. The refraction was spherical (n = 2), with the rule (plus or minus 10°) cylinder ⩾1. 50DC (n = 7), or anisometropia (n = 7; five had ⩽1.50DS difference). In accordance with department policy all children with an abnormal refraction were prescribed spectacles.
Children with low cylinder refractions (<1.00DC) and acuity outside the limits had spherical refractions >+4.00DS. Children with low spherical refractions and acuity outside the limits had cylinder refractions ⩾−2.00DC.
All children with normal refraction and acuity outside the limits or within the upper limits achieved a significantly improved acuity of ⩾0.225 log units when retested16 3–6 months later, with no spectacles having been prescribed.
Discussion
The mean monocular acuity for children with normal refraction was 0.200 (SD 0.09) for 3 year olds and 0.140 (SD 0.08) for 4 year olds. This compares well with reports of 0.09 (SD 0.100) for 4.9 year olds16 and 0.100 (SD 0.08) for 5.4 year olds11 obtained using the same vision test and 0.200 for 3 year olds, 0.175 for 4 year olds, and 0.100 for 5 year olds collated from a wide variety of uncrowded and crowded picture and letter vision tests.17 The refraction of children in these studies11,16,17 was not reported and it is possible that some had borderline or abnormal refractive error.
The purpose of screening is to identify a problem and a definitive vision score is the pass criteria. However, high under‐referral or over‐referral rates undermine the credibility of screening10 so it is important to determine whether amblyopia is present and ensure that those referred are not treated inappropriately. In many areas of clinical practice a statistically defined normal range of measurement is accepted. We propose our acuity limits represent a normal variant of acuity in children aged 3 years and 4 years who are asymptomatic, without strabismus with normal refraction.
The children with normal refraction and acuity outside the limits or acuity within the upper limits at initial assessment achieved a significantly improved acuity on retest without spectacle correction. This suggests they did not have amblyopia at initial clinical assessment.
Fifteen children with borderline refraction did not require spectacle correction to attain and maintain acuity within the limits, suggesting these refractions had not caused amblyopia. This is supported by a study that concluded treatment of mild vision (6/9–6/12) loss did not significantly benefit the children studied18 and the refractive error treated was probably physiological.19
Sixteen children with abnormal refraction had acuity within the limits. All children with an abnormal refractive error were prescribed spectacles. It is possible that amblyopia and/or symptoms may have developed if these refractions were left uncorrected.
If one accepts the concept of a normal range of vision, then based on careful consideration of the refraction data presented, hypermetropia of <4.00 DS, astigmatism of ⩽−1.50 DC, and anisometropia of <1.50 DS/DC did not appear to have caused amblyopia in the 3 year old and 4 year old children studied. The questions raised are, will a child remain symptom free with a normal level of visual acuity for age without any spectacle correction, and what is the natural history of a child's refraction and associated risk of developing amblyopia?
This study is limited because the small data sets lack statistical power when calculating 95% limits and the children do not represent a cross section of the wide population. In addition, it is difficult to draw any definitive conclusions on the distribution of refractions for age. Further study is therefore required to determine the risk of amblyopia for a given degree of refraction in young children.
Conclusion
A wide range of refraction maybe associated with a good level of visual acuity in children aged 3 years and 4 years.
Acknowledgements
We thank Amanda Chesworth and Jenni Spink for their assistance in data collection; Alison Firth for her comments on initial drafts of this paper; and Mark Muldoon (statistician) for reviewing the statistical analysis.
Abbreviations
IAD - interocular acuity difference
Footnotes
We have no competing interests.
The North West Wales NHS Trust ethics committee has approved this work. Investigation of patients was according to the guidelines of the Declaration of Helsinki.
References
- 1.Slataper F J. Age norms of refraction and vision. Arch Ophthalmol 195043466–479. [Google Scholar]
- 2.Gwiazda J, Thorn F, Bauer J.et al Emmetropisation and the progression of manifest refraction in children followed from infancy to puberty. Clin Vis Sci 19938337–344. [Google Scholar]
- 3.Zadnik K. Myopia development in childhood. Optom Vis Sci 199774603–608. [PubMed] [Google Scholar]
- 4.Wildsoet C F. Active emmetropisation—evidence for its existence and ramifications for clinical practice. Ophthal Physiol Opt 19974279–290. [PubMed] [Google Scholar]
- 5.Ingram R M, Arnold P E, Dally S.et al Emmetropisation, squint, and reduced visual acuity after treatment. Br J Ophthalmol 199175414–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ingram R M, Gill L E, Lambert T W. Effect of spectacles on changes of spherical hypermetropia in infants who did, and did not, have strabismus. Br J Ophthalmol 200084324–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Atkinson J, Anker S, Bobier W.et al Normal emmetropisation in infants with spectacle correction for hyperopia. Invest Ophthalmol Vis Sci 2000413726–3731. [PubMed] [Google Scholar]
- 8.Royal College of Ophthalmologists Guidelines for the management of strabismus and amblyopia in childhood. London: RCO, 2000
- 9.Donahue S P. How often are spectacles prescribed to ‘normal' preschool children? J AAPOS 20048224–229. [DOI] [PubMed] [Google Scholar]
- 10.Simons K. Visual acuity norms in young children. Surv Ophthalmol 19832884–92. [DOI] [PubMed] [Google Scholar]
- 11.Simmers A J, Gray L S, Spowart K. Screening for amblyopia: a comparison of paediatric letter tests. Br J Ophthalmol 199781465–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donahue S P, Johnson T M. Age‐based refinement of referral criteria for photoscreening. Ophthalmology 20011082309–2315. [DOI] [PubMed] [Google Scholar]
- 13.Ottar W L, Scott W E, Holgado S I. Photoscreening for amblyogenic factors. J Pediatr Ophthalmol Strabismus 199532289–295. [DOI] [PubMed] [Google Scholar]
- 14.Kohler L, Stigmar G. Vision screening of four‐year‐old children. Acta Paediat Scand 19736217–27. [DOI] [PubMed] [Google Scholar]
- 15.Miller J M, Harvey E R. Spectacle prescribing. Recommendations of AAPOS members. J Pediatr Ophthalmol Strabismus 19983551–52. [DOI] [PubMed] [Google Scholar]
- 16.Stewart C. Comparison of Snellen and log‐based acuity scores for school aged children. Br Orthopt J 20005732–37. [Google Scholar]
- 17.Fern K D, Manny R E. Visual acuity of the preschool child: a review. Am J Optom Physiol Opt 19865319–345. [DOI] [PubMed] [Google Scholar]
- 18.Clarke M P, Wright C M, Hrisos S.et al Randomised controlled trial of treatment of unilateral visual impairment detected at preschool vision screening. BMJ 20033271251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clarke M P. Correspondence. Response to comments on BMJ 2003327 pp 1251 Binoc Vis Strabismus Q 200419(No 1)7 [Google Scholar]