Abstract
Aim
To report on a new postoperative finding after delamination of the internal limiting membrane (ILM) for the treatment of different macular pathologies.
Methods
Seven patients are described with paracentral retinal holes, all located temporally to the macula, which developed after pars plana vitrectomy and uncomplicated ILM removal for cystoid macular oedema (n = 3), macular pucker (n = 3), and macular hole (n = 1) with the use of indocyanine green (n = 4), trypan blue (n = 1), triamcinolone acetonide (n = 1), or without dye (n = 1).
Conclusion
The use of dyes has been incriminated in causing iatrogenic damage to the retina. In this series, the new observation of retinal holes in the macular area is thought to be related to the removal of the ILM itself. The authors speculate that ILM delamination may cause a retinal weakening by Müller cell damage; this may be followed by a structural breakdown and, consequently, hole formation.
Keywords: internal limiting membrane, retinal holes, trypan blue
Delamination of the internal limiting membrane (ILM) has become a widespread and popular technique for the treatment of macular holes or macular oedema during the past years.1,2,3,4,5,6 The controversy about possible retinal damage focuses mainly on the use of different dyes.7,8,9,10 The removal of the ILM itself as the cause for retinal damage has not been raised as a possibility.
We describe seven cases of paracentral retinal holes all located temporally to the macula that developed after pars plana vitrectomy and seemingly atraumatic ILM peeling with indocyanine green (ICG), triamcinolone acetonide (TA), trypan blue (TB), or no dyes for different macular pathologies (table 1). Perhaps less attention has been focused upon the removal of the ILM as a possible cause of retinal damage.
Table 1 Summary of cases.
| Sex/age | Diagnosis | Procedure | Paracentral hole occurrence |
|---|---|---|---|
| F 68 | macular pucker, CMO | Vity, ILM/ICG | one hole, 2 months postop |
| F 68 | macular hole stage III | Vity, ILM/TB | multiple holes, 3 months postop |
| F 35 | PDRP, CMO | Vity, ILM/ICG | one hole, 3 months postop |
| F 57 | macular pucker | Vity, ILM | multiple holes, 2 months postop |
| M 67 | PDRP, CMO | Vity, ILM/ICG | one hole, 16 months postop |
| M 76 | vitreomacular traction syndrome, CMO, BRVO | Vity, ILM/ICG | one hole, 15 months postop |
| M 68 | macular pucker | Vity, ILM/TA | multiple holes, 3 weeks postop |
M, male, F, female, ICG, indocyanine green, TB, trypan blue, TA, triamcinolone acetonide, ILM, internal limiting membrane, Vity, vitrectomy, CMO, cystoid macular oedema, PDRP, proliferative diabetic retinopathy; BRVO, branch retinal vein occlusion.
Case reports
Patient 1
A 68 year old woman underwent membrane peeling followed by ICG assisted ILM delamination for idiopathic macular pucker associated with macular oedema in her left eye. The ICG (ICG‐Pulsion, Munich, Germany) was dissolved in 5% glucose to obtain a concentration of 0.05%. Approximately 0.1 ml was injected over the macular area under constant irrigation with Ringer solution and subsequently remnants were aspirated using the ocutome and the flute needle. Two months postoperatively a paramacular round retinal hole with a detached rim occurred (fig 1). Since no evident traction was present the hole was left untreated and no further problems occurred during a follow up of 6 months.
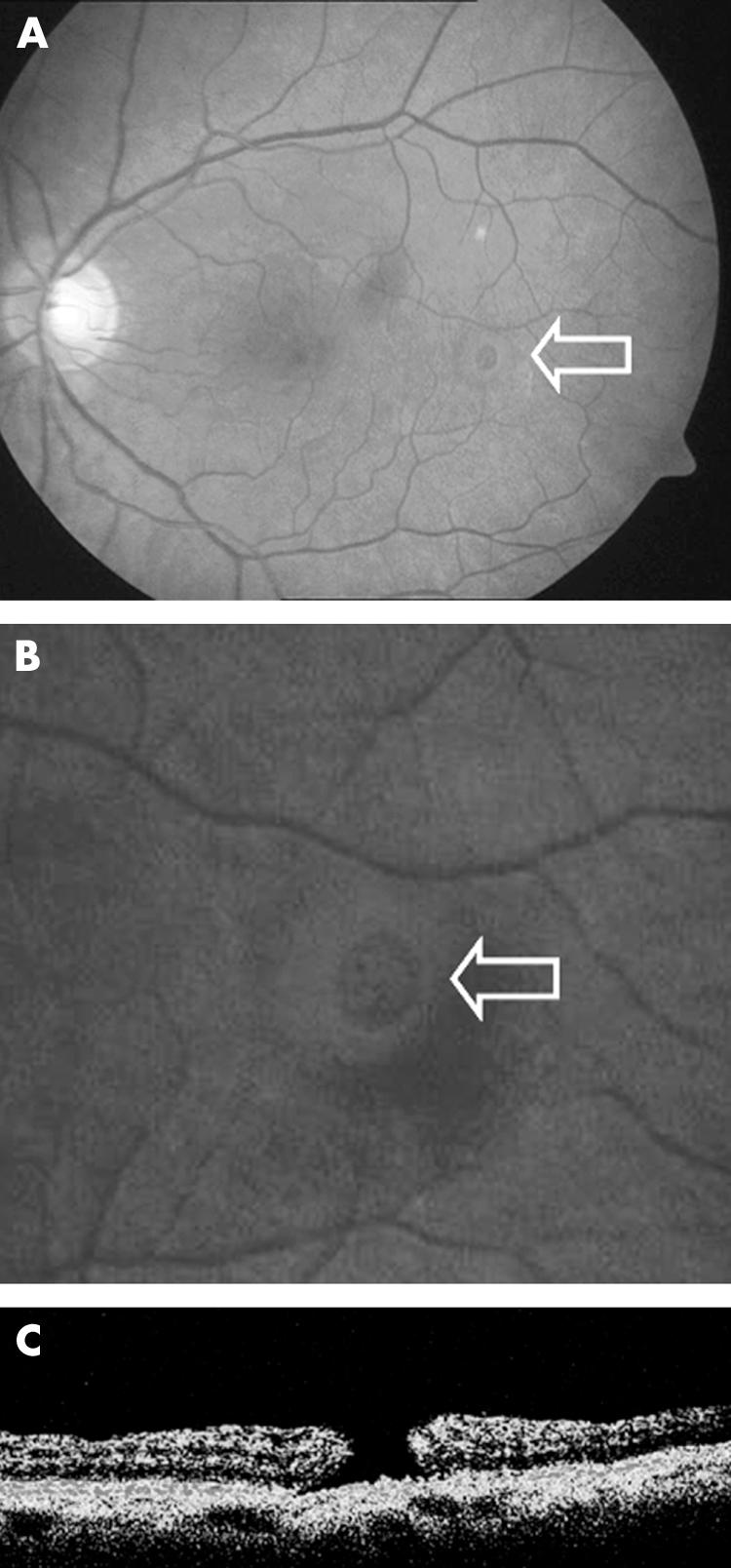
Figure 1 (A) Patient 1: paracentral hole after epiretinal membrane and ILM peeling. (B) Magnification of (A). (C) Corresponding optical coherence tomography scan showing a full thickness retinal hole.
Patient 2
A 68 year old woman underwent pars plana vitrectomy, posterior vitreous detachment, TB assisted ILM delamination, and 15% C2F6 endotamponade for a stage III macular hole in her left eye. Approximately 0.1 ml TB (Membrane Blue, Dorc International, Zuidland, Netherlands) with a concentration of 0.16% was applied over the posterior pole under constant irrigation with Ringer solution. Immediately after application, TB remnants were washed out as described above. At the 6 week follow up the macular hole was found to be open. No further holes were identified at this visit. She was scheduled for a second vitrectomy 4 weeks later. At surgery, multiple paracentral retinal holes were found, all located temporal to the original macular hole (fig 2). Fluid‐air exchange was carried out and the paracentral holes were treated with endophotocoagulation. No further retinal holes were observed thereafter during a further follow up period of 16 months.
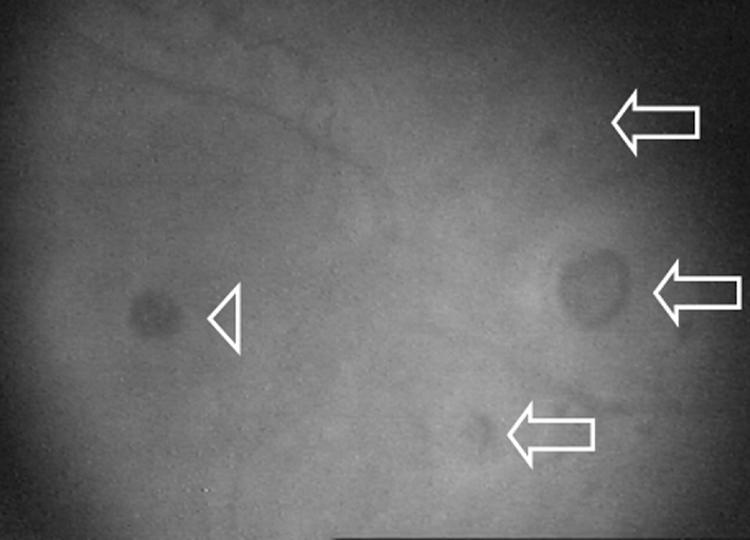
Figure 2 Patient 2. Intraoperative image: multiple paracentral holes (arrows) next to a persistent macular hole (arrowhead) after ILM removal with TB staining.
Patient 3
A 35 year old woman underwent vitrectomy, epiretinal membrane removal, and ICG assisted ILM delamination (as described above) for diabetic cystoid macular oedema in the left eye. Three months postoperatively a paramacular hole with surrounding intraretinal cysts in the detached rim was observed (fig 3). The hole was not treated, remained opened and the retina attached at follow up 12 months postoperatively.
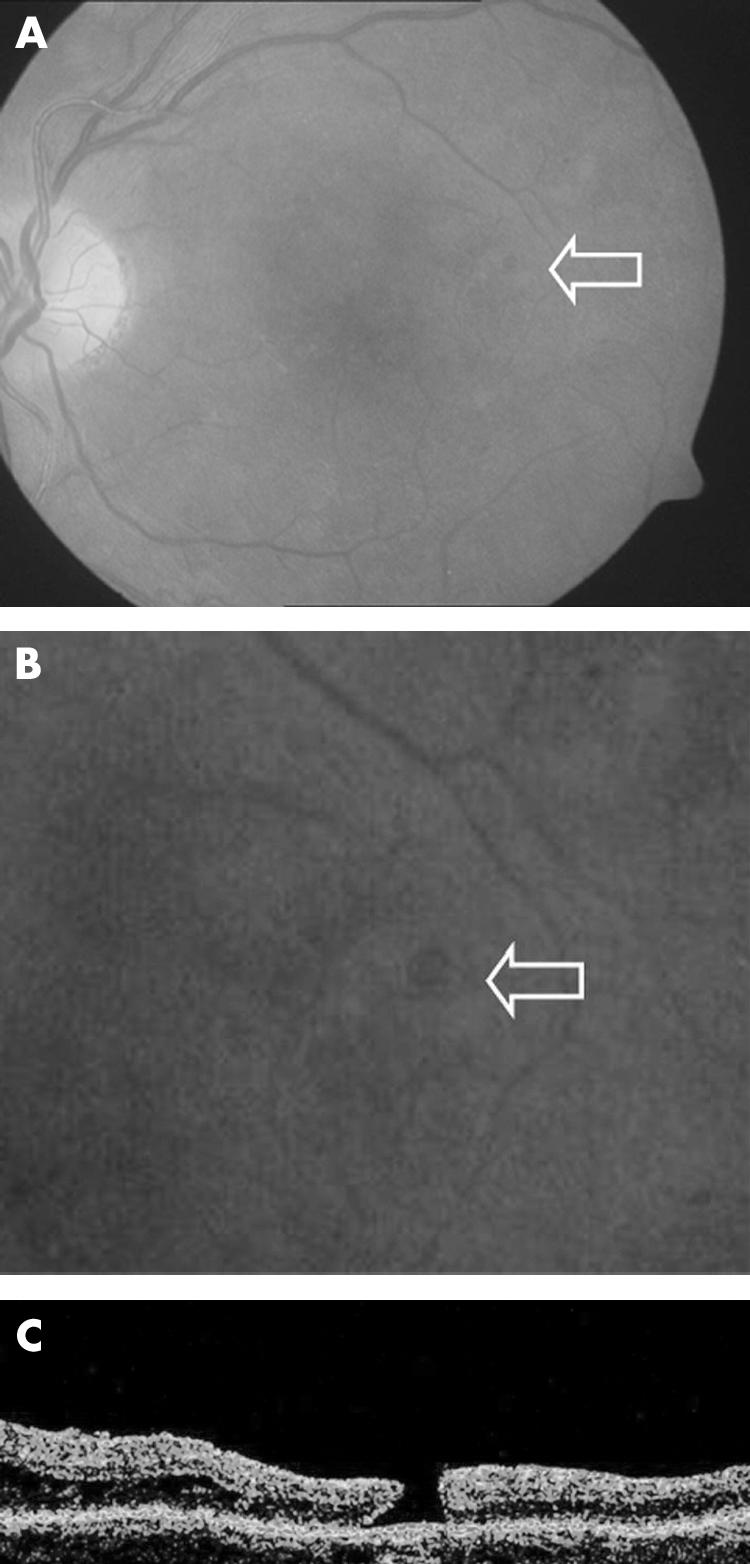
Figure 3 (A) Patient 3. Paracentral hole following ICG assisted ILM removal for cystoid macular oedema in a diabetic patient. (B) Magnification of (A). (C) Corresponding optical coherence tomography scan showing a full thickness retinal hole.
Patient 4
A 57 year old woman underwent epiretinal membrane peeling and ILM delamination (without the use of any dye) for macular pucker that developed following multiple retinal procedures used to treat a complicated rhegmatogenous retinal detachment in the right eye. Two months postoperatively a secondary round retinal hole was found temporal to the macula and this was treated with argon laser coagulation. No problems were observed thereafter during a further follow up of 48 months.
Patient 5
A 67 year old male diabetic patient underwent vitrectomy with ICG assisted ILM delamination (as described above) for severe proliferative diabetic retinopathy and cystoid macular oedema. Eight months postoperatively cataract surgery was performed and thereafter a paramacular round retinal hole could be observed. This was not treated and the retina remained attached at follow up of 11 months.
Patient 6
A 76 year old man had vitreoretinal traction syndrome associated with macular oedema; the underlying cause was a branch retinal vein occlusion in the left eye. He underwent vitrectomy; posterior hyaloid was detached and ILM was stained with ICG (as described above) and removed. Triamcinolone (4 mg, Hexal, Holzkirchen, Germany) was injected as an adjuvant at the end of surgery. Fifteen months postoperatively, a paramacular round hole was observed and this was treated with argon laser coagulation. No further problems occurred during a follow up of 7 months.
Patient 7
A 68 year old man was treated with vitrectomy, epiretinal membrane, and triamcinolone (4 mg, Kenalog, Squibb) assisted ILM peel for macular pucker. At his routine follow up appointment 3 weeks postoperatively multiple paramacular holes temporal to the fovea were found. These were not treated. The holes remained opened and the retina attached at follow up 14 months postoperatively.
Discussion
The beneficial effect on the anatomical and functional outcome of ILM removal for the treatment of various macular pathologies has been reported in several studies. There has been intense debate highlighting the possible toxic side effects of ICG; in contrast, retinal damage caused by the ILM removal has received less attention.7,9,11 Haritoglou et al described paracentral scotomata without biomicroscopically visible retinal defects in patients who had undergone ILM removal (without dyes) for macular hole surgery; the inference was that the removal of the ILM was in some way responsible for the visual defects.12 These defects were central and could also have been caused by direct and iatrogenic mechanical trauma of nerve fibres. Karacorlu et al presented chorioretinal lesions referred to as iatrogenic punctuate chorioretinopathy, caused by end gripping forceps but they did not report secondary holes.13
In our case series direct mechanical trauma is very unlikely, since the ILM peel was dye assisted in all but one patient. We did not observe any retinal haemorrhages, white retinal lesions, or any other signs of surgical trauma. All patients were operated by experienced vitreoretinal surgeons. Furthermore, all holes were located temporally to the macula and the starting point of ILM delamination was usually superior to the macula. Another argument against a mechanical cause is the long history of macular pucker surgery without ILM removal; there had never been any reported observation of secondary hole formation after “simple” pucker peeling. The more “aggressive” surgical approach involving ILM peeling for macular pucker is relatively recent. Part of the rationale of peeling ILM is to more completely excise the epiretinal retinal membrane. ILM staining enabled tissue to be removed over a much wider area. It is interesting to note that most of the secondary paracentral holes reported in this series are at some distance from the fovea.
Toxic effect of dyes has to be considered. The secondary paracentral holes in our patients occurred irrespective whether ICG, TB, TA, or no dye was used. Another important issue is the fact that four of the six patients presented with an initial cystoid macular oedema. ILM removal might have caused an opening of intraretinal cysts, although the biomicroscopic appearance of such ruptured cysts differs markedly from the observed secondary paracentral holes. Optical coherence tomography revealed no cystoid changes in the rim of the holes except in one eye with macular pucker and associated cystoid macular oedema (patient 1). Stalmans reported similar small retinal holes observed in one patient after ILM peeling, but in contrast with our findings the holes were located in an arcuate shape adjacent to the edge of the peeled area (Stalmans P, personal communication, 2005). He discussed contractions of the remaining ILM as a possible pathomechanism. The secondary holes seen in our patients were not located in an arcuate shape and were within the peeled area.
Stimulated by this clinical observation, we speculate about a weakening of the glial structure of the retina caused by the decapitation of the Müller cells since ultrastructural studies show remnants of Müller cell processes attached to the removed ILM with signs of necrosis.14,15,16
As Müller cells exchange waste products of active retinal neurons, ILM removal may result in a glial apoptosis and subsequent reduced retinal function after removal of the Müller cell plates.17,18,19 In the case of macular hole treatment, this cell damage may be necessary to activate regenerative mechanisms and to induce glial proliferation leading to hole closure; but it may be also responsible for the weakening of the glial structures of the central retina leading to retinal hole development.20 This theory is supported by the finding that all secondary paracentral holes developed in the area of ILM removal. It is unclear to us why these secondary holes developed temporal but not nasal to the macula.
Our report describes for the first time secondary central retinal hole formation as a possible complication of ILM removal in macular surgery. If these holes are indeed related to ILM peeling, perhaps there is an argument to limit the size of the area that we denude the retina of the ILM.
Abbreviations
ICG - indocyanine green
ILM - internal limiting membrane
TA - triamcinolone acetonide
TB - trypan blue
References
- 1.Gandorfer A, Messmer E M, Ulbig M W.et al Resolution of diabetic macular edema after surgical removal of the posterior hyaloid and the inner limiting membrane. Retina 200020126–133. [PubMed] [Google Scholar]
- 2.Brooks H L., Jr Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology 20001071939–48 discussion 1948–9. [DOI] [PubMed] [Google Scholar]
- 3.Mandelcorn M S, Nrusimhadevara R K. Internal limiting membrane peeling for decompression of macular edema in retinal vein occlusion: a report of 14 cases. Retina 200424348–355. [DOI] [PubMed] [Google Scholar]
- 4.Kumagai K, Furukawa M, Ogino N.et al Vitreous surgery with and without internal limiting membrane peeling for macular hole repair. Retina 200424721–727. [DOI] [PubMed] [Google Scholar]
- 5.Dillinger P, Mester U. Vitrectomy with removal of the internal limiting membrane in chronic diabetic macular oedema. Graefes Arch Clin Exp Ophthalmol 2004242630–637. [DOI] [PubMed] [Google Scholar]
- 6.Bovey E H, Uffer S, Achache F. Surgery for epimacular membrane: impact of retinal internal limiting membrane removal on functional outcome. Retina 200424728–735. [DOI] [PubMed] [Google Scholar]
- 7.Stalmans P, Van Aken E H, Veckeneer M.et al Toxic effect of indocyanine green on retinal pigment epithelium related to osmotic effects of the solvent. Am J Ophthalmol 2002134282–285. [DOI] [PubMed] [Google Scholar]
- 8.Kodjikian L, Richter T, Halberstadt M.et al Toxic effects of indocyanine green, infracyanine green, and trypan blue on the human retinal pigmented epithelium. Graefes Arch Clin Exp Ophthalmol 2005 [DOI] [PubMed]
- 9.Sippy B D, Engelbrecht N E, Hubbard G B.et al Indocyanine green effect on cultured human retinal pigment epithelial cells: implication for macular hole surgery. Am J Ophthalmol 2001132433–435. [DOI] [PubMed] [Google Scholar]
- 10.Gandorfer A, Haritoglou C, Kampik A. Retinal damage from indocyanine green in experimental macular surgery. Invest Ophthalmol Vis Sci 200344316–323. [DOI] [PubMed] [Google Scholar]
- 11.Gass C A, Haritoglou C, Schaumberger M.et al Functional outcome of macular hole surgery with and without indocyanine green‐assisted peeling of the internal limiting membrane. Graefes Arch Clin Exp Ophthalmol 2003241716–720. [DOI] [PubMed] [Google Scholar]
- 12.Haritoglou C, Ehrt O, Gass C A.et al Paracentral scotomata: a new finding after vitrectomy for idiopathic macular hole. Br J Ophthalmol 200185231–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karacorlu M, Karacorlu S, Ozdemir H. Iatrogenic punctate chorioretinopathy after internal limiting membrane peeling. Am J Ophthalmol 2003135178–182. [DOI] [PubMed] [Google Scholar]
- 14.Gandorfer A, Haritoglou C, Gass C A.et al Indocyanine green‐assisted peeling of the internal limiting membrane may cause retinal damage. Am J Ophthalmol 2001132431–433. [DOI] [PubMed] [Google Scholar]
- 15.Eckardt C, Eckardt U, Groos S.et al [Removal of the internal limiting membrane in macular holes. Clinical and morphological findings]. Ophthalmologe 199794545–551. [DOI] [PubMed] [Google Scholar]
- 16.Wolf S, Schnurbusch U, Wiedemann P.et al Peeling of the basal membrane in the human retina: ultrastructural effects. Ophthalmology 2004111(2)238–243. [DOI] [PubMed] [Google Scholar]
- 17.Winter M, Eberhardt W, Scholz C.et al Failure of potassium siphoning by Muller cells: a new hypothesis of perfluorocarbon liquid‐induced retinopathy. Invest Ophthalmol Vis Sci 200041256–261. [PubMed] [Google Scholar]
- 18.Newman E, Reichenbach A. The Muller cell: a functional element of the retina. Trends Neurosci 199619307–312. [DOI] [PubMed] [Google Scholar]
- 19.Newman E A. Regional specialization of retinal glial cell membrane. Nature 1984309155–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bringmann A, Reichenbach A. Role of Muller cells in retinal degenerations. Front Biosci 20011:6E72–E92. [DOI] [PubMed] [Google Scholar]


