Abstract
Aim
To attempt to validate two scoring systems for the prediction of intraoperative complication during phacoemulsification surgery.
Methods
The study population was patients attending Sunderland Eye Infirmary who underwent phacoemulsification surgery between 1 January 2001 and 31 December 2003. The authors applied each scoring system to a control group of 300 patients from this study population and extrapolated the results to give an estimate of the spread of scores for the entire population. They then applied the same scoring systems to all complicated cases from the same study population. Using these results they were able to calculate the risk of a complication for a particular score on each scoring system.
Conclusion
The application of these systems in clinical practice would allow appropriate selection of phacoemulsification cases for trainee surgeons, more accurate consent from patients for their phacoemulsification surgery, and the unbiased comparison of surgical outcomes from surgeons with differing case mix difficulties.
Keywords: phacoemulsification, posterior capsule rupture, scoring systems
Until now, prediction of the likelihood of a complication during phacoemulsification surgery has been based on a preoperative subjective assessment of the patient by the operating surgeon.
A more robust and objective system to determine the probability of a complication during such surgery would be desirable for three reasons: (1) it would allow appropriate selection of cases for trainee phacoemulsification surgeons, with lower risk cases being reserved for the trainees with least surgical experience; (2) it would help surgeons to inform patients appropriately as to the predicted risk relating to their proposed surgery; (3) it would permit better comparison of results from surgeons with differing case mix.
Two systems have been devised for the prediction of complication in phacoemulsification surgery (Muhtaseb et al, Moorfields Eye Hospital1 and Habib et al, Sunderland Eye Infirmary2). The aim of this study was to attempt to validate these systems.
Both systems are based on the same principle of allocating points for individual risk factors thought to increase the likelihood of a complication during surgery. The points are then summated to provide an overall score for each patient preoperatively—that is, a potential complication score. The points allocated to each risk factor using each system are shown in table 1.
Table 1 Point allocation for risk factors using Muhtaseb's and Habib's scoring systems.
| Risk factor | Score allocated | ||
|---|---|---|---|
| Muhtaseb's scoring system | Habib's scoring system | ||
| Miscellaneous risk assessed by the surgeon (eg, poor position of eye/patient) | 1 | – | |
| Unable to lie flat (spinal deformity, asthma, heart failure) | – | 1 | |
| Severe anxiety | – | 1 | |
| Head tremor | – | 1 | |
| Previous angle closure glaucoma | – | 1 | |
| History of complication in fellow eye | – | 1 | |
| Previous vitrectomy | 1 | 1 | |
| Corneal scarring/cloudiness | 1 | 1 | |
| Shallow anterior chamber | 1 | 1 | |
| Poor pupillary dilation and/or posterior synechiae | 1 | 1 | |
| Pseudoexfoliation | 3 | 1 | |
| Phacodonesis/weak zonules | 3 | 1 | |
| High ametropia (>6D myopia or hyperopia) | 1 | – | |
| High myopia (axial length >27 mm) | – | 1 | |
| High hypermetropia (axial length <20 mm) | – | 1 | |
| Age >88 years | 1 | – | |
| Nuclear density grade 1–2 | – | 1 | |
| Nuclear density grade 3 | – | 2 | |
| Mature/brunescent/white/dense/total cataract | 3 | 3 | |
| Posterior capsule plaque | 1 | – | |
| Posterior polar cataract | 1 | – | |
Muhtaseb et al describe the additional step of arranging patients into risk groups, where patients scoring 0 are in group 1, patients scoring 1–2 are in group 2, patients scoring 3–5 are in group 3, and patients scoring ⩾6 are in group 4.
By such methods, the higher the patient's score/risk group, the higher the likelihood of them sustaining a complication during surgery.
Materials and methods
For the study, we examined the case notes of selected patients from a study population of all patients undergoing uncombined phacoemulsification surgery by any consultant in a single site eye hospital between 1 January 2001 and 31 December 2003 (inclusive). It should be noted that this population differed significantly from the population examined by Habib et al in order to formulate their “potential difficulty score” (a population undergoing cataract surgery between 1996 to 2001), and that we did not use any data from the 528 case notes used in their study.2
In order to calculate the risk of a complication associated with a particular preoperative potential complication score, three steps were required: (1) establish the prevalence of that score in the entire study population; (2) ascertain the number of complicated cases in the entire study population who had the same score; (3) from these results the percentage risk of complication for a particular preoperative score could be calculated.
An outline of these methods is as follows:
(1) To estimate the prevalence of each score in the entire population we used a randomised sample group of 300 patients from the entire population (100 patients from each year). Randomisation of patients for inclusion in the control group was achieved by applying a randomisation computer program (www.randomization.com‐“third generator”) to the hospital database for all patients in the study population.
Using both Muhtaseb and Habib's scoring systems, we then established potential complication scores for each patient of the control sample by retrospective analysis of the patients' preoperative case notes, without reference to the operative notes.
We then extrapolated the potential complication scores in the control sample group to the entire population using the following calculation.
For a particular score:
Extrapolated number of patients in the entire population with that score = (Number of patients in the control group with that score × Number of patients in study population)/Number of patients in the control group (n = 300)
(2) From the same study population, we were also able to identify all patients who sustained an intraoperative complication(s), by analysis of the hospital surgical database and theatre diaries. Both scoring systems were applied to each of these patients, again by retrospective analysis of the patients' preoperative case notes, and the potential complication score for each patient was calculated. A complication was defined as posterior capsule rupture and/or vitreous loss with or without loss of nucleus/nuclear fragments.
(3) With knowledge of the (extrapolated) potential complication scores for the entire study population and the potential complication scores for all of the complicated cases in the entire study population we were able to determine the percentage risk of complication for any particular score from the following calculation:
For a particular score:
Risk of complication (%) = (Number of complicated cases in entire population with that score/Extrapolated number of patients in the entire population with that score) ×100
Results
The total number of cases in our study population was 11 913.
During case note retrieval for the control group, three sets of case notes could not be located (two from 2001 and one from 2002), and three more patients were randomly selected (two from 2001 and one from 2002) using the same randomisation process to give a control sample of 300 patients.
All of the case notes for complicated cases from the study period were located—there being 27 cases from 2001, 36 from 2002, and 32 from 2003 (total of 95 complicated cases from the 3 year study period).
The results for scores in the control group, complicated cases, and calculated risk according to score are shown in table 2.
Table 2 Potential complication scores for patients in the control group and complication group, and the calculated risk of complication according to the potential complication score.
| System | Potential complication score | Comparative results for control group (n = 300) | Comparative results for all complicated cases (n = 95) | Complication risk (95% CI) | |
|---|---|---|---|---|---|
| Number of patients in control group with that score | Extrapolated to entire study population (n = 11 913) | ||||
| Muhtaseb et al | 0 | 213 | 8458 | 54 | 0.64% (0.48% to 0.83%) |
| 1 | 67 | 2661 | 20 | 0.75% (0.46% to 1.16%) | |
| 2 | 9 | 357 | 2 | 0.56% (0.07% to 2.01%) | |
| 3 | 9 | 357 | 11 | 3.08% (1.55% to 5.45%) | |
| 4 | 2 | 80 | 7 | 8.75% (3.59% to 17.2%) | |
| 5 | 0 | 0 | 1 | Not calculable | |
| Habib et al | 1 | 218 | 8657 | 51 | 0.59% (0.44% to 0.77%) |
| 2 | 52 | 2065 | 19 | 0.92% (0.55% to 1.43%) | |
| 3 | 26 | 1032 | 17 | 1.65% (0.96% to 2.62%) | |
| 4 | 3 | 119 | 6 | 5.04% (1.87% to 10.65%) | |
| 5 | 1 | 40 | 2 | 5.00% (0.61% to 16.92%) | |
Table 3 shows complication risk in relation to potential complication group as described in Muhtaseb et al's study, in which patients were stratified into four risk groups according to their total score from summating the points for their individual risk factors.
Table 3 Complication risk association with potential complication group using Muhtaseb et al's scoring system.
| Risk group (potential complication score) | Complication risk (95% CI) | |
|---|---|---|
| 1 (0) | 0.64% (0.48 to 0.86%) | |
| 2 (1–2) | 0.72% (0.46 to 1.10%) | |
| 3 (3–5) | 4.35% (2.64 to 6.71%) | |
| 4 (⩾6) | Not calculable |
As would have been expected, using each system, there was an inverse relation between the potential complication score and the number of cases in the control group attaining that score (table 1, column 3). Column 5 of table 1 shows the frequency of each potential complication score in all complicated cases over the 3 year study period using both scoring systems. When these figures are used to calculate the risk of complication associated with a particular score (table 1, column 6), there is a direct relation between the potential complication score and the incidence of complication—that is, the higher the potential complication score, the higher the likelihood of complication. This relation has a more continuous pattern using Habib's scoring system. However, when patients are grouped according to their difficulty scores, as described in Muhtaseb's original paper, there seems to be a direct relation between potential complication score and complication incidence (table 2).
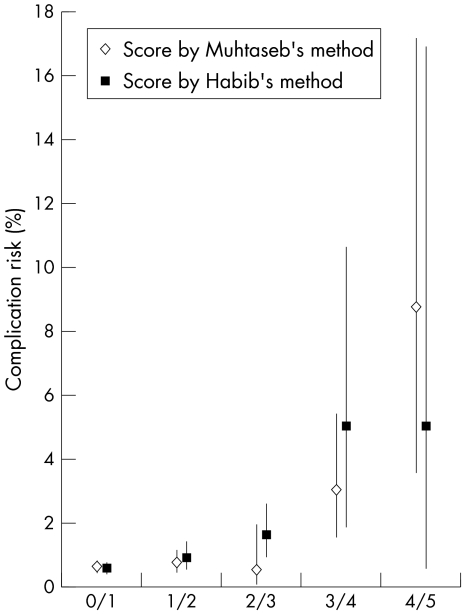
Figure 1 plots of the relation between the potential complication score and complication risk for each system, with the 95% confidence intervals indicated. As can be seen, there is a direct relation between potential complication score and complication risk using each system. This relation is more convincing with Habib's scoring system, with little apparent difference in risk for patients scoring 0–2 on Muhtaseb's system.
Figure 1 Graph showing the complication risk association with potential complication score using Muhtaseb's and Habib's scoring systems.
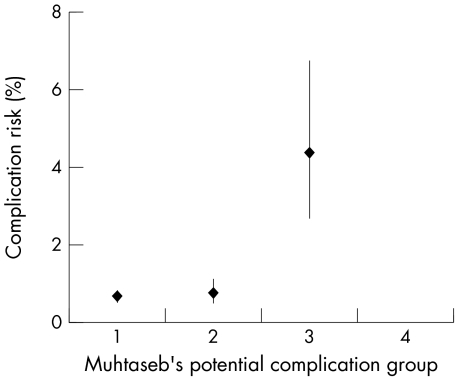
Using Muhtaseb's grouping system (fig 2) there is an increased risk of complication in patients in group 3 compared with that for patients in risk groups 1 or 2. However, there appears to be little difference in complication risk between risk groups 1 and 2.
Figure 2 Graph showing the complication risk association with potential complication group using Muhtaseb's scoring system..
Clearly, more accurate estimates of the complication risk associated with a particular score would be obtained if we had the resources to obtain exact scores for all 11 913 patients in the study population. For this study, 300 subjects were selected at random from all 11 913 patients in order to estimate the distribution of scores in the entire study population. The confidence intervals indicated in the above tables and graphs are derived with the assumption that the distribution of scores in this random sample correlates with that in the entire population. While this may contribute some additional uncertainty, we do not believe that this invalidates our calculation.
Discussion
Our results support the validity of the scoring protocol of Muhtaseb et al, and the “potential difficulty score” system of Habib et al. However, in applying the scoring system advocated by Habib et al, the potential complication scores seem to correlate more closely with the actual complication incidence than with Muhtaseb's system.
Both systems use similar scoring strategies, which are simple and quick to apply in the clinical setting. This is an important practical consideration if either system is to be employed in clinical practice.
The formulation of the design of each scoring system differed. Muhtaseb et al designed their system based on a Medline review of literature pertaining to complications/complication rates in phacoemulsification surgery. Characteristics that have been shown to increase the likelihood of intraoperative complications were identified as risk factors then allocated an appropriately weighted score. Habib et al designed their system based on a questionnaire to ophthalmic consultants in which risk factors predisposing to intraoperative complication were ranked. They also used information from previous work by Willerscheidt et al3 and Najjar and Awwad.4
Both of these methods appear to have resulted in systems which can be predictive of intraoperative complication by the use of information that is readily available from the preoperative notes and/or preoperative assessment of the patient. It would be desirable to establish the significance of individual risk factors by a more objective means, and allocate an appropriately weighted score for each risk factor accordingly. This, however, would require a large scale, prospective, multicentre study.
In each system there were anomalies in some of the scores allocated to certain risk factors.
It is surprising that both systems credit posterior polar cataract with a low score in terms of relative risk. Muhtaseb's scoring system allocated only one point to this risk factor and Habib's system did not allocate any points to this risk factor. Previous studies have indicated that the presence of posterior polar cataract alone is associated with a 26–40% risk of posterior capsule rupture during phacoemulsification surgery.5,6,7 While the risk of posterior capsule rupture in patients with posterior polar cataract can be reduced by modifying the surgical technique,8,9,10 we think that this is a major contributing factor to complications and that cases of posterior polar cataract should be given greater significance in any risk calculation.
Both systems scored for zonular weakness but neither system allocated a score for traumatic cataract, which, regardless of zonular integrity, may be associated with a higher risk of posterior capsule rupture.11 Indeed, in our study, three of the complicated cases had a history of significant ocular trauma, with significantly more advanced cataract in the traumatised eye, but no clinical evidence of zonular weakness/dehiscence. In such cases, phacoemulsification surgery should be undertaken with caution.
There is also evidence that previous complicated phacoemulsification surgery in the fellow eye is associated with an increased risk of complication during surgery to the second eye.12 Only Habib et al scored this as a risk factor.
Despite these anomalies, both of these scoring systems could be used as predictors of potential intraoperative complication.
The application of either of these validated scoring systems in clinical practice is of value for several reasons.
The use of such a system would allow appropriate selection of cases for trainee surgeons. This would effectively tailor cases to each surgeon based on that trainee's surgical experience. It has been argued that this would limit trainees' experience to only straightforward cases,13 but we would advocate that, using either system, surgeons with increasing experience can be introduced to more difficult cases with higher risk scores in a more controlled and graduated manner.
The use of either of these systems would allow surgeons to obtain accurate informed consent from patients, with those patients in higher risk groups being informed of their higher risk of complication and the poor outcome which could result. However, it should be borne in mind that, while posterior capsule rupture is undoubtedly associated with a poorer outcome in phacoemulsification surgery,14 many patients have excellent visual outcome despite intraoperative posterior capsule rupture.12,15,16 Also, other complications may occur, which may lead to adverse visual outcome such as wound leak, iris prolapse, suprachoroidal haemorrhage, or intraocular lens malposition. These potential adverse events may not be predicted using the potential complication scoring systems, but should be conveyed to the patient during consent.
These scoring systems could also be used to aid the unbiased comparison of results from surgeons with different case mix—that is, to compare the results from a surgeon performing surgery in predominantly “routine” cases with those of a surgeon performing predominantly “complex” cases. This would create a more level playing field when assessing the surgical outcomes of any surgeon and is an extremely important consideration during revalidation or appraisal of a particular surgeon.
Conclusion
We have attempted to validate two scoring systems for the prediction of complications during phacoemulsification surgery.
Both scoring systems would appear to be useful in predicting the likelihood of a complication, although Habib's “potential difficulty score” system appears to be a more reliable predictor.
Both of these scoring systems can easily be applied in clinical practice and are of practical use in the selection of cases for trainee surgeons, the informed consent of patients for their phacoemulsification surgery, and the fair comparison of surgical outcomes from different surgeons.
In using these scoring systems, we think that it would be appropriate to consider posterior polar cataracts and traumatic cataracts on their own merits, and would recommend that such cases always be performed by a surgeon with suitable experience.
Further prospective, multicentre studies are required to establish the influence of individual risk factors on surgical outcome.
Footnotes
Competing interests: none declared
Ethics approval for this study was obtained from Sunderland Local Research Ethics Committee on 24 January 2005. REC reference number: 05/Q0904/2.
References
- 1.Muhtaseb M, Kalhoro A, Ionides A. A system for preoperative stratification of cataract patients according to risk of intraoperative complications: a prospective analysis of 1441 cases. Br J Ophthalmol 2004881242–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Habib M S, Bunce C V, Fraser S G. The role of case mix in the relation of volume and outcome in phacoemulsification. Br J Ophthalmol. (in press) [DOI] [PMC free article] [PubMed]
- 3.Willerscheidt A B, Healey M L, Ireland M. Cataract surgery outcomes: importance of co‐morbidities in case mix. J Cataract Refract Surg 199521177–181. [DOI] [PubMed] [Google Scholar]
- 4.Najjar D M, Awwad S T. Cataract surgery risk score for residents and beginning surgeons. J Cataract Refract Surg 2003292035–2036. [DOI] [PubMed] [Google Scholar]
- 5.Vasavada A, Singh R. Phacoemulsification in eyes with posterior polar cataract. J Cataract Refract Surg 199925238–245. [DOI] [PubMed] [Google Scholar]
- 6.Osher R, Yu B C ‐ Y, Koch D. Posterior polar cataracts: a predisposition to intraoperative capsular rupture. J Cataract Refract Surg 199016157–162. [DOI] [PubMed] [Google Scholar]
- 7.Gavris M, Popa D, Caraus C.et al Phacoemulsification in posterior polar cataract. Oftalmologia 20044836–40. [PubMed] [Google Scholar]
- 8.Hayashi K, Hayashi H, Nakao F.et al Outcomes of surgery for posterior polar cataract. J Cataract Refract Surg 20032945–49. [DOI] [PubMed] [Google Scholar]
- 9.Fine I H, Packer M, Hoffman R S. Management of posterior polar cataract. J Cataract Refract Surg 20032916–19. [DOI] [PubMed] [Google Scholar]
- 10.Allen D, Wood C. Minimizing risk to the capsule during surgery for posterior polar cataract. J Cataract Refract Surg 200228742–744. [DOI] [PubMed] [Google Scholar]
- 11.Zhang Y, Zhang J, Shi S. [Determination of posterior lens capsule status in traumatic cataract with B‐ultrasonography]. (in Chinese) Zhonghua Yan Ke Za Zhi 199834298–299. [PubMed] [Google Scholar]
- 12.Mullhern M, Kelly G, Barry P. Effects of posterior capsular disruption on the outcome of phacoemulsification surgery. Br J Ophthalmol 1995791133–1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tyson S. A system for preoperative stratification of cataract patients according to risk of complications: a prospective analysis of 1441 cases—comment. Evidence‐Based Eye Care 20056121–123. [Google Scholar]
- 14.Ionides A, Minassian D, Tuft S. Visual outcome following posterior capsule rupture during cataract surgery. Br J Ophthalmol 200185222–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan F M, Mathur R, Ku J J.et al Short‐term outcomes in eyes with posterior capsule rupture during cataract surgery. J Cataract Refract Surg 200329537–541. [DOI] [PubMed] [Google Scholar]
- 16.Yap E Y, Heng W J. Visual outcome and complications after posterior capsule rupture during phacoemulsification surgery. Int Ophthalmol 19992357–60. [DOI] [PubMed] [Google Scholar]