Abstract
Aim
To evaluate the outcomes of combined intravitreal triamcinolone (IVTA) and photodynamic therapy (PDT) with verteporfin in the treatment of subfoveal choroidal neovascularisation (CNV) caused by age related macular degeneration (AMD).
Methods
48 eyes from 48 patients with subfoveal CNV caused by AMD were prospective recruited, with 24 eyes treated with combined PDT with IVTA and compared with a control group of 24 eyes which received PDT monotherapy. In the combined treatment group, IVTA was performed immediately after PDT as an outpatient procedure. The mean number of treatments, mean logMAR best corrected visual acuity (BCVA), mean line of visual acuity changes, and proportion of patients without moderate visual loss at 1 year were compared between the combined and monotherapy groups.
Results
At 1 year the logMAR BCVA for the PDT with IVTA group changed from 0.88 to 0.95 (p = 0.32 compared with baseline), whereas the logMAR BCVA for the monotherapy group reduced from 0.74 to 1.09 (p<0.001 compared with baseline). A significantly higher proportion of patients who had PDT with IVTA did not develop moderate visual loss at 1 year compared with the monotherapy group (70.8% and 33.3% respectively, p = 0.009). Eyes which had combined treatment had significantly fewer lines lost compared with monotherapy alone (0.7 and 3.5 lines respectively, p = 0.015). Subgroup analysis showed that PDT with IVTA is effective in preventing visual loss in both predominately classic and occult CNV groups. The mean number of treatments for the combined and monotherapy groups was 1.5 and 1.96 respectively (p = 0.076).
Conclusions
Combined PDT with IVTA appeared more effective statistically at 12 months for stabilisation of vision (<3 logMAR lines change) compared with PDT monotherapy. Further randomised control trials might be justified to conclude the efficacy of PDT with IVTA.
Keywords: photodynamic therapy, intravitreal triamcinolone, choroidal neovascularisation, age related macular degeneration
Photodynamic therapy (PDT) with verteporfin has been shown to be effective in the treatment of choroidal neovascularisation (CNV) secondary to age related macular degeneration (AMD).1,2 Despite the demonstrated efficacy, a substantial proportion of patients still developed moderate or severe visual loss after PDT. Moreover, results from patients with occult CNV larger than four disc areas and good visual acuity appeared less favourable.2 One of the reasons for the less favourable outcome in treating large lesion might be because of collateral damage to adjacent structures as choriocapillaris hypoperfusion and retinal pigment epithelium (RPE) atrophy after PDT have been reported.3,4,5 The associated damage results in retinal oedema and release of angiogenesis factors like vascular endothelial growth factor (VEGF).6,7 Functionally, some patients might develop transient visual disturbances shortly after PDT, with reduction in retinal function as demonstrated objectively by multifocal electroretinography.8 Therefore, it will be useful to identify agents that might increase and optimise the efficacy of PDT in the treatment of CNV.
Triamcinolone acetonide is a corticosteroid demonstrated to have potent anti‐angiogenic properties and can inhibit angiogenesis growth factors which affect interendothelial cell tight junctions and reduce cytokines release, cell migration, and proliferation.9,10,11,12,13,14,15 However, clinical studies using intravitreal triamcinolone acetonide (IVTA) alone in treating CNV secondary to AMD have failed to confirm the beneficial visual outcome.16,17,18 Therefore, combination therapy of PDT with IVTA might provide synergetic effects to improve the outcome of PDT. Preliminary results appeared promising as combined therapy was associated with lower re‐treatment rates with patients having visual improvements.19,20,21 However, since no control groups were available in previous studies, it was difficult to draw conclusion on the efficacy of combined PDT with IVTA. We therefore performed a prospective study to evaluate the efficacy of combined PDT with IVTA compared with a non‐concurrent control group with PDT monotherapy in the treatment of CNV caused by AMD.
Patients and methods
This was a non‐randomised comparative study in which consecutive patients who received combined treatment were prospectively recruited from Hong Kong Eye Hospital and Prince of Wales Hospital from May 2003. The inclusion criteria included: (i) age 50 years or older; (ii) subfoveal CNV which was predominantly classic or occult without the classic component; (iii) best corrected visual acuity (BCVA) of 20/400 or better; (iv) leakage within CNV on fluorescein angiography (FA); and (v) greatest linear dimension of the lesion <5400 μm. Exclusion criteria included: (i) evidence of secondary CNV such as choroiditis and pathological myopia; (ii) previous CNV treatment including PDT, laser, or submacular surgery; and (iii) history of glaucoma. The combined treatment group was compared with a non‐concurrent group which received PDT alone from January 2002 to April 2003 based on the same inclusion and exclusion criteria, except glaucoma was not an exclusion criterion. Twenty eight eyes treated in the period were identified in which 24 eyes were selected for the control group based on the CNV lesion size and composition to match with the combined treatment group. The protocols were approved by an ethics committee and informed consents were obtained from all patients.
At baseline and post‐treatment visits, BCVA was measured with an ETDRS logMAR chart at 4 metres or a Snellen chart at 6 metres being converted to logMAR equivalent for calculation.22 Dilated fundal examination, fundus photography and fluorescein angiography (FA) were performed. Assessments of FA were performed by two unmasked ophthalmologists (TL and AW) and any disagreement was settled by consensus. The definitions and assessments of FA lesions were based on the Macular Photocoagulation Study (MPS) and the TAP study, particularly on lesion size, angiographic leakage, and lesion composition.1,23
PDT with verteporfin was performed according to the TAP and VIP studies.1,2 For patients in the combined group, IVTA injection was performed as an outpatient procedure 5 minutes after PDT under strict aseptic techniques. Local anaesthesia was achieved using 2% lidocaine hydrochloride jelly (Xylocaine, AstraZenec). Povidone‐iodine was applied followed by intravitreal injection of 0.1 ml of 4 mg triamcinolone acetonide (Kenacort‐A, Bristol‐Myers‐Squibb, Italy) using a 27 gauge needle 4 mm post‐limbus. Indirect ophthalmoscopy and tonometry were carried out after the procedure and anterior chamber paracentesis was performed in patients who had sustained post‐injection intraocular pressure (IOP) of 30 mm Hg or above. Patients were given topical levofloxacin 0.5% four times daily (Cravit, Santen, Japan) for 2 weeks.
Follow up visits were arranged every 3 months with BCVA testing, tonometry, fundal examination, and FA performed as with baseline. Additional visits at 1 week and 1 month were offered to the combined group for IOP and complication monitoring. Anti‐glaucomatous eye drops were used temporarily in patients with IOP of ⩾21 mm Hg. In cases with angiographic leakage in the follow up FA, repeated PDT with IVTA injection was performed in the combined group if IOP was normal (<21 mm Hg) and PDT alone in the monotherapy group. Further IVTA injections were performed in patients who developed short term IOP elevation if the IOP returned to normal (<21 mm Hg) after cessation of anti‐glaucomatous eye drops at the time of re‐treatment.
The primary outcome measure was the proportion of eyes that maintained stable vision (drop <3 logMAR lines). Other outcome measures included changes in logMAR BCVA, changes in number of lines, and the mean number of treatment required during the 1 year study period. Safety was assessed by recording any ocular or systemic adverse effects during follow up.
Statistical analysis was performed using SPSS v11.5. χ2 or Fisher's exact tests were used to compare the proportion of patients without moderate visual loss between the two groups. Serial changes in logMAR BCVA were compared using Wilcoxon signed ranks test. The mean number of treatment and lines of BCVA changes in the combined and monotherapy groups were compared using Mann‐Whitney U test. Subgroup analyses were also carried out to evaluate the treatment outcomes of classic and occult CNV.
Results
Patients demographics
Twenty four eyes of 24 patients in each of the combined and monotherapy groups were analysed. All completed the follow up at 12 months. The baseline demographics are summarised in table 1. Analyses showed all major baseline characteristics were comparable between the two groups (p>0.05).
Table 1 Baseline demographics of 48 patients who had combined PDT with IVTA or PDT monotherapy.
| All eyes (n = 48) | Combined PDT + IVTA (n = 24) | PDT monotherapy (n = 24) | p Value | |
|---|---|---|---|---|
| Mean age (years) (SD) | 73.6 (7.5) | 73.9 (8.2) | 73.3 (6.9) | 0.78* |
| Sex | ||||
| Male | 37 | 18 | 19 | 0.73† |
| Female | 11 | 6 | 5 | |
| Lens status | ||||
| Phakic | 37 | 19 | 18 | 0.73† |
| Pseudophakic | 11 | 5 | 6 | |
| Mean duration of symptoms (months) | 4.9 | 4.8 | 5.1 | 0.84* |
| CNV angiographic appearance | ||||
| Classic | 23 | 12 | 11 | 0.78† |
| Occult | 25 | 12 | 13 | |
| Mean baseline CNV greatest linear dimension (μm) (SD) | 2690 (830) | 2640 (910) | 2740 (760) | 0.66* |
| Mean baseline logMAR BCVA (Snellen equivalent) | 0.81 (20/129) | 0.88 (20/152) | 0.74 (20/110) | 0.21‡ |
| Mean baseline IOP (mm Hg) (SD) | 12.3 (2.5) | 12.1 (2.3) | 12.7 (2.8) | 0.44* |
*:Two tailed t test; †χ2 test; ‡Mann‐Whitney U test.
All subfoveal CNV lesions
For the 24 eyes treated with PDT and IVTA, the mean logMAR BCVA changed from 0.88 (Snellen equivalent of 20/152) at baseline to 0.95 (Snellen equivalent of 20/178) at 1 year. The reduction in BCVA at the 1 year follow up compared with baseline was not statistically significant (Wilcoxon signed ranks test, p = 0.32). For the PDT monotherapy group, the mean logMAR BCVA changed from 0.74 (Snellen equivalent of 20/110) at baseline to 1.09 (Snellen equivalent of 20/246) at 1 year and the reduction was statistically significant (Wilcoxon signed ranks test, p<0.001).
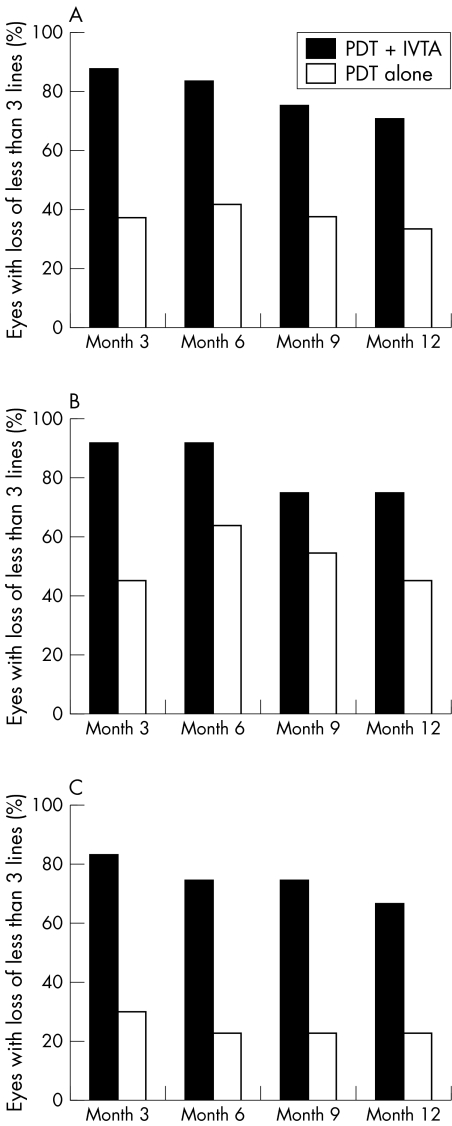
In terms of lines of BCVA changes, the mean number of lines reduced at 12 months for the combined and monotherapy groups was 0.7 and 3.5, respectively. Patients who received combined treatment had significantly fewer lines lost at 1 year compared with those who had monotherapy alone (Mann‐Whitney U test, p = 0.015). For the proportion of patients without moderate visual loss, 17 (70.8%) eyes in the combined group compared with eight (33.3%) eyes in the monotherapy group lost fewer than three lines of BCVA at 12 months (χ2 test, p = 0.009) (fig 1A).
Figure 1 The proportion of eyes without moderate visual loss (less than three lines of visual acuity) at each follow up visit. (A) All 48 eyes; (B) 23 eyes with predominately classic CNV, and (C) 25 eyes with occult CNV.
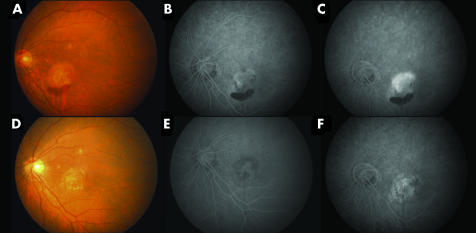
Although the combined therapy group did receive fewer mean treatment sessions than the monotherapy group, 1.50 and 1.96 treatments, respectively, in the first year, the difference was not statistically significant (Mann‐Whitney U test, p = 0.076). An illustrative case of a patient treated with combined PDT with IVTA is displayed in figure 2.
Figure 2 (A) Pretreatment fundus photograph of a patient with subfoveal CNV and haemorrhage at the inferior border. The patient's best corrected visual acuity was 20/200. (B) Early phase of fluorescein angiogram demonstrated a predominately classic subfoveal CNV with (C) leakage in the late phase. (D) Fundus photograph 3 months after a single session of combined PDT with IVTA showing resolution of the haemorrhage with fibrosis of the CNV. The patient's vision improved to 20/100. (E) Early and (F) late phases of fluorescein angiogram showed resolution of the CNV with no evidence of leakage.
Subgroup: predominantly classic CNV
The mean logMAR BCVA of the combined therapy group improved slightly from 0.92 (Snellen equivalent of 20/166) at baseline to 0.89 (Snellen equivalent of 20/155) at 1 year, while the monotherapy declined from 0.78 (Snellen equivalent of 20/121) to 1.01 (Snellen equivalent of 20/205). The change in logMAR BCVA at 1 year was not statistically significant for the combined treatment group (Wilcoxon signed ranks test, p = 1.0). For the monotherapy group, the logMAR BCVA was significantly worse at 1 year compared with baseline (Wilcoxon signed ranks test, p = 0.031). In terms of the mean line of BCVA changes at 1 year, the combined therapy group improved by 0.3 lines, while the monotherapy group decreased by 2.4 lines but the difference was not statistically significantly (Mann‐Whitney U test. p = 0.10). Nine (75.0%) eyes in the combined PDT with IVTA compared with five (45.5%) eyes treated with PDT monotherapy lost fewer than three lines of BCVA 1 year after treatment (Fisher exact test, p = 0.21) (fig 1B). The mean number of treatment for the 12 eyes with predominately classic CNV which had combined treatment and the 11 eyes which had monotherapy was 1.67 and 1.91, respectively. No significant difference in the number of PDT sessions was found between the two groups (Mann‐Whitney U test, p = 0.55).
Subgroup: occult CNV
There were 12 and 13 eyes with occult CNV in the combined and monotherapy groups respectively. The mean logMAR BCVA declined from 0.85 (Snellen equivalent of 20/142) at baseline to 1.01 (Snellen equivalent of 20/205) at 12 months for the combined therapy group, and reduced from 0.71 (Snellen equivalent of 20/103) to 1.16 (Snellen equivalent of 20/289) for the monotherapy group. The reduction in logMAR BCVA was not statistically significant at 1 year for the combined treatment group (Wilcoxon signed ranks test, p = 0.051), whereas for the monotherapy group, the reduction in logMAR BCVA was statistically significant (Wilcoxon signed ranks test, p = 0.006). Eight (66.7%) eyes in the combined PDT with IVTA group compared with three (23.1%) eyes treated with PDT monotherapy lost fewer than three lines of vision 1 year after treatment (Fisher exact test, p = 0.028) (fig 1C). The mean number of treatment for the combined and monotherapy groups was 1.33 and 2.00 respectively (Mann‐Whitney U test, p = 0.056).
Complications
None of the patients developed ocular or systemic complications related to PDT. Eight (33.3%) of the 24 eyes in the combined treatment group developed a transient increase in IOP ⩾21 mm Hg following IVTA injection and all were managed with anti‐glaucomatous eye drops. Seven of the eight eyes which developed IOP elevation did not require subsequent PDT and one eye with normal IOP after cessation of anti‐glaucomatous drops underwent repeat PDT with IVTA. Five (26.3%) of the 19 phakic patients in the combined therapy group also developed an increase in cataract of which three (15.8%) subsequently required cataract surgery. No serious complications such as endophthalmitis and retinal detachment developed after IVTA injection.
Discussion
Corticosteroids may be a useful therapeutic agent in the treatment of CNV because of their dual anti‐inflammatory and anti‐angiogensis actions.9,10,11,12,13,14,15 As the anti‐angiogensis effects of PDT with verteporfin are usually transient, a combination of PDT with an intermediate acting corticosteroid like triamcinolone acetonide may be a promising treatment option by creating longer lasting and possible synergistic effects on the CNV.19 Spaide et al reported the use of combined PDT with IVTA in 26 patients with CNV secondary to AMD.19,21 At the 12 month follow up, the mean acuity improved by 2.4 lines in patients newly treated with PDT, and by 0.3 lines in patients who had previous PDT.21 Rechtman et al also evaluated the use of IVTA as an adjunct to PDT in 14 patients with CNV caused by AMD.20 At 1 year after treatment, eight (57%) patients had stable or improved vision and six (43%) patients suffered a loss of 15 letters or more. From these studies, the visual outcomes appeared more superior compared with the results in the TAP and VIP studies.1,2 However, both the above studies had the limitations of a lack of control group for comparison and it was difficult to determine the treatment efficacy.
In this comparative study our results showed that combined PDT with IVTA appeared to have more favourable results compared with PDT alone. Patients who underwent PDT with IVTA had no significant reduction in logMAR BCVA, whereas those who had PDT monotherapy still developed significant reduction in logMAR BCVA. After 12 months of follow up, patients in the combined treatment group had significantly better visual outcome in terms of lines of BCVA changes. Moreover, patients who had combined PDT with IVTA were less likely to suffer moderate visual loss compared with PDT alone, which was the primary outcome of the study. For the number of treatment sessions, patients who had combined therapy had 1.5 sessions, compared with 1.96 sessions for the monotherapy group. Although the difference was not statistically significant, it appeared that IVTA might reduce the re‐treatment rate in PDT. The low retreatment was also observed in the study by Spaide et al,20 when the mean number of treatments given in the first year was 1.24 in the newly treated group.
Subgroup analysis also demonstrated that combined PDT with IVTA was effective in both classic and occult CNV as no significant reductions in BCVA were observed after combined therapy. PDT with IVTA appeared particularly useful for occult CNV as significantly higher proportion of eyes in the combined therapy group did not have moderate visual loss; with only 33% of patients lost three or more lines after combined treatment. As demonstrated in the VIP study,2 the visual outcome of PDT for occult CNV in AMD was generally compromised as more than 50% of verteporfin treated eyes developed visual loss of three or more lines after 1 year. Therefore, combined PDT with IVTA might be particularly useful in patients with occult CNV.
In contrast with the results reported by Spaide et al, which showed a mean improvement of 2.4 lines after PDT with IVTA,21 our results were more modest as patients who had combined therapy still developed a mean BCVA reduction of 0.7 lines. This might be due to differences in patients' duration of symptoms and CNV size but the exact reason is unclear as the baseline characteristics were not reported by Spaide et al. None the less, our results were superior compared with those reported by Rechtman et al. In their study, the mean visual acuity decreased by four lines at 1 year after PDT with IVTA.20 The inferior visual outcome might be due to delayed IVTA injection which was given within 6 weeks of PDT rather than on the same day. Since IVTA might reduce the inflammatory response as well as the choriocapillaris damage after PDT, immediate IVTA injection after PDT might therefore be more beneficial in improving the visual outcomes. The optimal timing of IVTA injection in combination with PDT therefore warrants further investigation.
In summary, our comparative study demonstrated that PDT with IVTA appeared to be more effective in the treatment of CNV secondary to AMD compared with PDT alone. Moreover, combined therapy appeared to be relatively safe as the side effects were relatively mild, with transient IOP elevation and cataract development in 33.3% and 26.3% of patients, respectively. These rates of complications were comparable to previous studies on combined PDT with IVTA and no serious complications such as endophthalmitis developed in our series.19,20,21 The main limitation of our study was only a small number of patients were available in the subgroup analysis based on lesion types and therefore the power of the subgroup analysis is limited. Another shortcoming was the lack of randomisation. In view of the encouraging results, further randomised controlled trials may be justified to determine the role of IVTA injection in PDT for the treatment of neovascular AMD.
Abbreviations
AMD - age related macular degeneration
BCVA - best corrected visual acuity
CNV - choroidal neovascularisation
FA - fluorescein angiography
IOP - intraocular pressure
IVTA - intravitreal triamcinolone
PDT - photodynamic therapy
RPE - retinal pigment epithelium
VEGF - vascular endothelial growth factor
Footnotes
Financial interest: nil.
Financial support: supported by Competitive Earmarked Research Grant #4140/02M
Competing interests: none declared
References
- 1.Bressler N M. Photodynamic therapy of subfoveal choroidal neovascularization in age‐related macular degeneration with verteporfin: two‐year results of 2 randomized clinical trials—TAP report 2. Arch Ophthalmol 2001119198–207. [PubMed] [Google Scholar]
- 2.Verteporfin in Photodynamic Therapy Report 2 Verteporfin therapy of subfoveal choroidal neovascularization in age‐related macular degeneration: two‐year results of a randomized clinical trial inkling lesions with occult with no classic choroidal neovascularisation. Am J Ophthalmol 2001131541–560. [DOI] [PubMed] [Google Scholar]
- 3.Moshfeghi D M, Kaiser P K, Grossniklaus H E.et al Clinicopathologic study after submacular removal of choroidal neovascular membranes treated with verteporfin ocular photodynamic therapy. Am J Ophthalmol 2003135343–350. [DOI] [PubMed] [Google Scholar]
- 4.Flower R W, von Kerczek C, Zhu L.et al Theoretical investigation of the role of choriocapillaris blood flow in the treatment of subfoveal choroidal neovascularization associated with age‐related macular degeneration. Am J Ophthalmol 200113285–93. [DOI] [PubMed] [Google Scholar]
- 5.Wachtlin J, Behme T, Heimann H.et al Concentric retinal pigment epithelium atrophy after a single photodynamic therapy. Graefes Arch Clin Exp Ophthalmol 2003241518–521. [DOI] [PubMed] [Google Scholar]
- 6.Schmidt‐Erfurth U, Schlotzer‐Schrehard U, Cursiefen C.et al Influence of photodynamic therapy on expression of vascular endothelial growth factor (VEGF), VEGF receptor 3, and pigment epithelium‐derived factor. Invest Ophthalmol Vis Sci 2003444473–4480. [DOI] [PubMed] [Google Scholar]
- 7.Rogers A H, Martidis A, Greenberg P B. Puliafito CA. Optical coherence tomography findings following photodynamic therapy of choroidal neovascularization. Am J Ophthalmol 2002134566–576. [DOI] [PubMed] [Google Scholar]
- 8.Lai T Y, Chan W M, Lam D S. Transient reduction in retinal function revealed by multifocal electroretinogram following photodynamic therapy. Am J Ophthalmol 2004137826–833. [DOI] [PubMed] [Google Scholar]
- 9.Ishibashi T, Miki K, Sorgente N.et al Effects of intravitreal administration of steroids on experimental subretinal neovascularization in subhuman primate. Arch Ophthalmol 1985103708–711. [DOI] [PubMed] [Google Scholar]
- 10.Antoszyk A N, Gottlieb J L, Machemer R.et al The effects of intravitreal triamcinolone acetonide on experimental pre‐retinal neovascularization. Graefes Arch Clin Exp Ophthalmol 199323134–40. [DOI] [PubMed] [Google Scholar]
- 11.Ciulla T A, Criswell M H, Danis R P.et al Intravitreal triamcinolone acetonide inhibits choroidal neovascularization in a laser‐treated rat model. Arch Ophthalmol 2001119399–404. [DOI] [PubMed] [Google Scholar]
- 12.Wang Y S, Friedrichs U, Eichler W.et al Inhibitory effects of triamcinolone acetonide on bFGF‐induced migration and tube formation in choroidal microvascular endothelial cells. Graefes Arch Clin Exp Ophthalmol 200224042–48. [DOI] [PubMed] [Google Scholar]
- 13.Penfold P L, Wen L, Madigan M C.et al Modulation of permeability and adhesion molecule expression by human choroidal endothelial cells. Invest Ophthalmol Vis Sci 2002433125–3130. [PubMed] [Google Scholar]
- 14.Ciulla T A, Criswell M H, Danis R P.et al Choroidal neovascular membrane inhibition in a laser treated rat model with intraocular sustained release triamcinolone acetonide microimplants. Br J Ophthalmol 2003871032–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matsuda S, Gomi F, Oshima Y.et al Vascular endothelial growth factor reduced and connective tissue growth factor induced by triamcinolone in ARPE19 cells under oxidative stress. Invest Ophthalmol Vis Sci 2005461062–1068. [DOI] [PubMed] [Google Scholar]
- 16.Challa J K, Gillies M C, Penfold P L.et al Exudative macular degeneration and intravitreal triamcinolone: 18 month follow up. Aust N Z J Ophthalmol 199826277–281. [DOI] [PubMed] [Google Scholar]
- 17.Danis R P, Ciulla T A, Pratt L M.et al Intravitreal triamcinolone acetonide in exudative age‐related macular degeneration. Retina 200020244–250. [PubMed] [Google Scholar]
- 18.Gillies M C, Simpson J M, Billson F A.et al Safety of an intravitreal injection of triamcinolone: results from a randomized clinical trial. Arch Ophthalmol 2004122336–340. [DOI] [PubMed] [Google Scholar]
- 19.Spaide R F, Sorenson J, Maranan L. Combined photodynamic therapy with verteporfin and intravitreal triamcinolone acetonide for choroidal neovascularization. Ophthalmology 20031101517–1525. [DOI] [PubMed] [Google Scholar]
- 20.Rechtman E, Danis R P, Pratt L M.et al Intravitreal triamcinolone with photodynamic therapy for subfoveal choroidal neovascularisation in age related macular degeneration. Br J Ophthalmol 200488344–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spaide R F, Sorenson J, Maranan L. Photodynamic therapy with verteporfin combined with intravitreal injection of triamcinolone acetonide for choroidal neovascularization. Ophthalmology 2005112301–304. [DOI] [PubMed] [Google Scholar]
- 22.Holladay J T. Proper method for calculating average visual acuity. J Refract Surg 199713388–391. [DOI] [PubMed] [Google Scholar]
- 23.Macular Photocoagulation Study Group Subfoveal neovascular lesions in age‐related macular degeneration: guidelines for evaluation and treatment in the Macular Photocoagulation Study. Arch Ophthalmol 19911091242–1257. [PubMed] [Google Scholar]