Abstract
Aims
To determine the long term outcome of Molteno implants inserted using a modified surgical technique that eliminates the need for a donor scleral graft.
Methods
Retrospective case series involving a medical record analysis of 35 consecutive patients undergoing first Molteno implant surgery for refractory glaucoma. The main outcomes included life table analysis of intraocular pressure control following surgery and frequency of intraoperative and postoperative complications.
Results
There were no complications related specifically to the modified method of tube placement. Medium term intraocular pressure control was similar to other series.
Conclusions
This simplified method for the insertion of Molteno implants eliminates the need for a donor scleral graft while maintaining the implant's ability to control intraocular pressure.
Keywords: surgical technique, Molteno implant, glaucoma, donor scleral graft
The use of a drainage seton is common in patients with refractory glaucoma and other complicated glaucomas. Molteno first described the use of his implant in 1969 and it has proved to be a reliable and effective device.1 There are now several other drainage setons including the Ahmed valve, Baerveldt device, and Krupin valve.2 All rely on a fine bore silicone tube that is placed into the anterior chamber at the limbus or through the pars plana into the vitreous cavity. The tube has a relatively long extrascleral course and is covered by donor material such as sclera, dura, or pericardium to prevent conjunctival erosion of the tube.3,4 Recently, concerns have been raised regarding the potential risk of iatrogenic transmission of variant Creutzfeldt‐Jakob disease (vCJD) via graft tissue.5
Ozdamar et al described the results of a scleral tunnel without an overlying scleral graft in six patients undergoing Krupin eye valve implants.6 In this study we describe the results using a scleral tunnel for tube placement of Molteno implants in a large series of patients with a long follow up. This technique eliminates of the need for a donor scleral graft to cover the site of tube placement.
Materials and methods
Patients for this study were recruited from two tertiary referral centres and consisted of consecutive patients operated upon by the authors over the period 1991 to 2002 using a modified surgical technique for the insertion of Molteno implants developed by one of the authors (HMAT).
Patients were selected for Molteno surgery because they had glaucoma uncontrolled on maximum tolerated medical therapy and were considered at high risk of failure for trabeculectomy or had previously failed trabeculectomy. Patient data collected included age, sex, diagnosis, number of preoperative glaucoma medications, preoperative visual acuity, and intraocular pressure (IOP). Postoperative data included visual acuity, IOP, and number of glaucoma medications at 1 week, 3, 6, 9, and 12 months postoperatively and for every subsequent postoperative visit. The postoperative IOP was taken as the mean of the values for each postoperative year. Any intraoperative or postoperative complication was recorded. All available follow up data were used. Institutional approval for this study was obtained from the hospital human ethics committee.
Modified surgical technique
This modified surgical technique eliminates the need for a donor patch graft and an appreciably shorter operative time may be anticipated by the surgeon.
A fornix based conjunctival flap is fashioned and the recti identified. A partial thickness scleral incision 2 mm in length and 5–6 mm posterior to the limbus is made at the midpoint of the quadrant in which the tube is to be inserted. A 20 gauge microvitreoretinal (MVR) knife is then carefully bent into a curve matching that of the globe. The MVR blade is introduced into the scleral incision and gently advanced towards the limbus creating a partial thickness scleral tunnel analogous to the construction of a scleral tunnel for phacoemulsification (fig 1). The MVR blade should be faintly visible within the sclera to give the correct depth. At the posterior border of the surgical limbus a “dimple down” manoeuvre equivalent to that made before anterior chamber entry in scleral tunnel phacoemulsification wound construction is performed. This allows anterior chamber entry of the knife in a plane parallel to the iris. Care is necessary to avoid trauma to the iris, ciliary body, and lens.
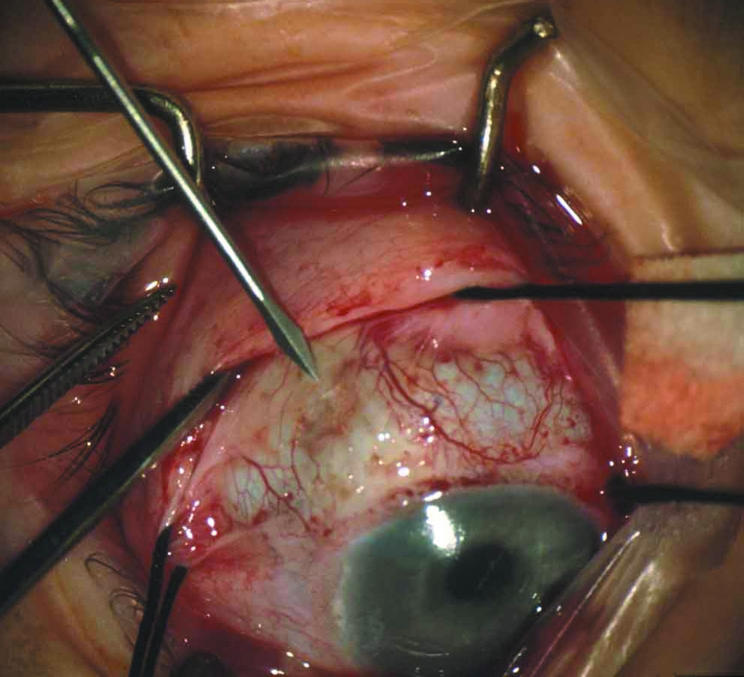
Figure 1 A partial thickness scleral incision is made at the midpoint of the quadrant in which the plate is to be inserted.
The MVR blade is removed and the Molteno plate(s) then attached to the globe (fig 2). A Vicryl tie or ripcord suture can be used. The Molteno tube is trimmed and inserted down the tunnel into the anterior chamber using fine tying forceps (fig 3). The conjunctiva is then closed.
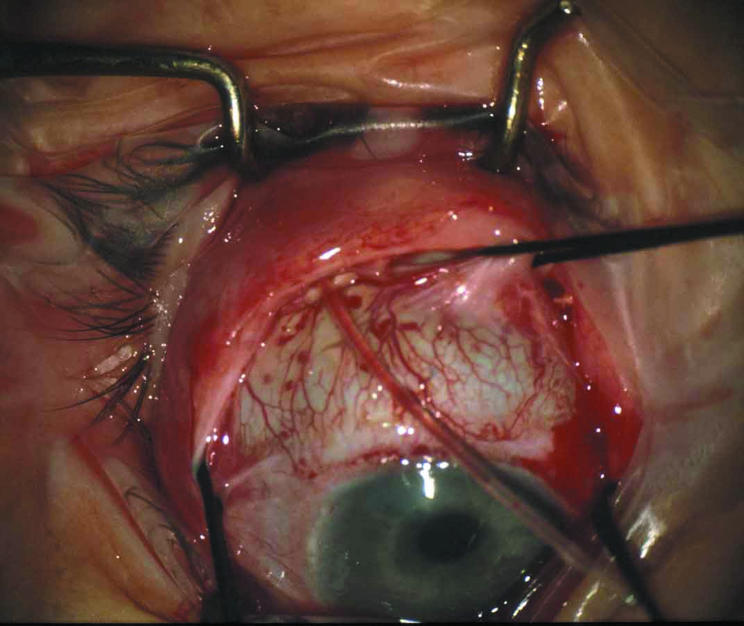
Figure 2 The Molteno plate is attached to the globe.
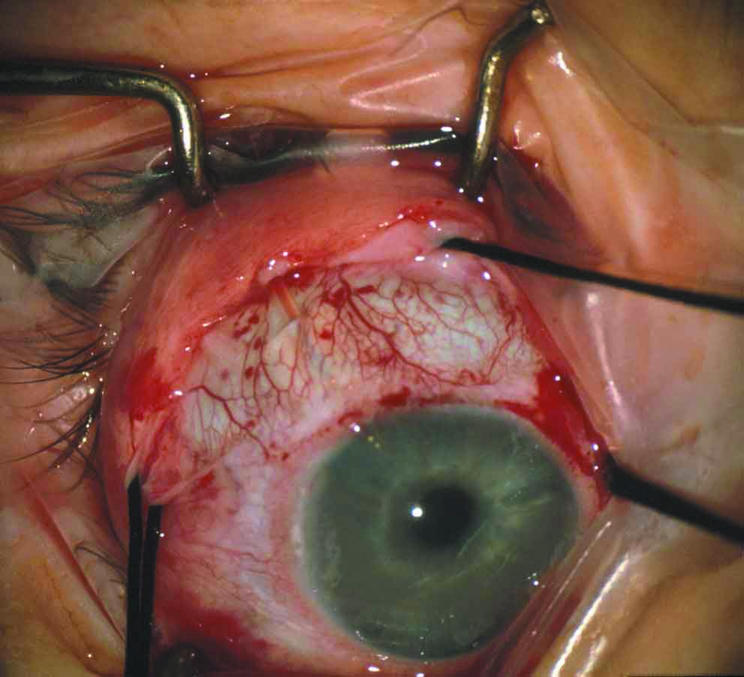
Figure 3 The Molteno tube is trimmed and inserted down the tunnel into the anterior chamber.
Definition of success
Complete success was defined as an IOP between 6 mm Hg and 21 mm Hg without additional ocular hypotensive medications. Qualified success was defined as an IOP between 6 mm Hg and 21 mm Hg with or without additional topical medication. Failure was defined as persistent IOP >21 mm Hg, hypotony <6 mm Hg, a requirement for cyclodestructive procedure, or further glaucoma surgery. A transient elevation of IOP was permitted if the mean IOP for the 12 month period was less than 21 mm Hg and the subsequent IOP was <21 mm Hg. If it remained elevated the time of failure was taken as the first date the elevation was recorded.
Statistical methods
Repeated measures using generalised estimating equations (GEE) were used to assess the IOP between pre‐Molteno and post‐Molteno eyes, as this approach accounts for variable follow up and potential missing data. This approach may be thought of as a repeated measures t test. p Values of <0.05 were considered as being significant; 95% confidence intervals were used to assess plausible ranges of true differences. Standard tests confirming normal distribution of data were used before performing all statistical analyses.
Using the above definitions of success, time to event methods involving Kaplan‐Meier appraisal were used to describe the time to IOP outcome in patients undergoing Molteno surgery. To avoid the effects of correlation only the first procedure of patients undergoing bilateral procedures was included in the analysis. In order to conduct survival analysis all patients who received Molteno implants were included in this analysis, including those who had less than 6 months of follow up. In patients who had not experienced an event, censoring was at their last follow up visit. Additionally, patients not reviewed in the 12 months before collecting the data were considered lost to follow up and censored at the time of their last visit.
To test whether there was a different time to outcome in the two main subgroups of patients, the log rank test (utilising time to event methods) and differences were expressed as hazard ratios. Confidence intervals were obtained to ascertain the plausible magnitude of effects.
Results
During the study period 35 consecutive patients underwent Molteno implant surgery with this modified surgical technique. The records of one patient were unable to be located for review and eight patients had not been reviewed in the 12 months before collecting the data. The male to female ratio was 1:1 and the mean age was 62.5 years (range 21–85 years). The mean duration of follow up was 49.9 months. The patient demographic data according to diagnostic group are shown in table 1.
Table 1 Glaucoma diagnoses.
| Glaucoma diagnosis | Number of eyes | Mean age (years) (SD) | Sex (M:F %) | Mean follow up (months) (SD) |
|---|---|---|---|---|
| All patients | 34 | 62 (17) | 50:50 | 50 (41) |
| Neovascular | 11 | 67 (13) | 55:45 | 28 (22) |
| Uveitis | 10 | 49 (21) | 30:70 | 84 (47) |
| POAG | 4 | 77 (6) | 75:25 | 66 (31) |
| PKPG | 2 | 70 (1) | 100:0 | 63 (38) |
| Fuchs' corneal dystrophy | 2 | 62 (25) | 50:50 | 25 (18) |
| Pseudophakic | 1 | 67 | 0:100 | 42 |
| CCAG | 1 | 63 | 0:100 | 36 |
| ICE syndrome | 1 | 48 | 0:100 | 24 |
| Traumatic | 1 | 53 | 100:0 | 1 |
| Miscellaneous | 1 | 82 | 100:0 | 4 |
POAG, primary open angle glaucoma; PKPG, penetrating keratoplasty with associated glaucoma; CCAG, chronic closed angle glaucoma; ICE, iridocorneal endothelial.
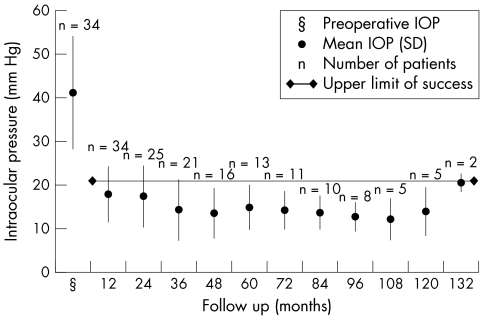
The mean (SD) preoperative IOP was 41.2 (13.0) mm Hg. This fell to 17.9 (6.4) mm Hg after 1 year and 17.4 (7.0) after 2 years. It fluctuated between 12.2 mm Hg and 14.9 mm Hg for the remaining follow up to 10 years (fig 4). At the end of the postoperative follow up period the mean IOP was 20.5 (2.1) mm Hg. The GEE analysis shows an average reduction from baseline and postoperative pressure (over the follow up period) of 23.5 mm Hg (95% confidence interval for the difference is 19.4–27.5 mm Hg), which was statistically significant, p<0.01.
Figure 4 Intraocular pressure versus time profile.
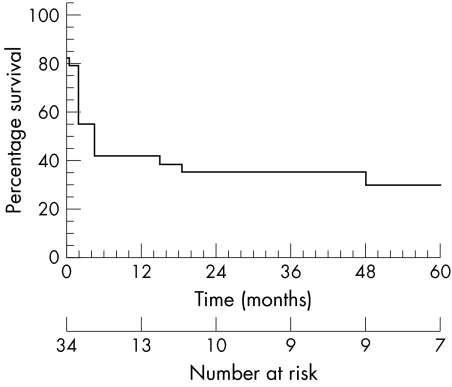
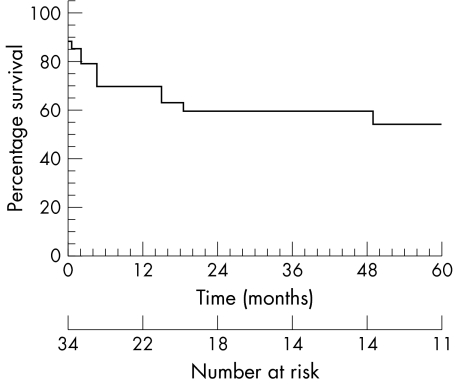
The Kaplan‐Meier survival curves for the probability of successful IOP control are shown in figures 5 and 6. The complete success rate at 1 year was 42%; this fell to 35% at 2 years and 30% at 5 years. The qualified success rates at 1, 2, and 5 years were 70%, 60%, and 54%, respectively. The small number of patients with more than 5 years of follow up prevented the determination of survival rates beyond 5 years.
Figure 5 Kaplan‐Meier survival analysis based on the definition of “Complete success.”
Figure 6 Kaplan‐Meier survival analysis based on the definition of “Qualified success.”
According to the log rank test there was insufficient evidence to demonstrate a significant difference in the survival of the neovascular or uveitis patients using either definition of success.
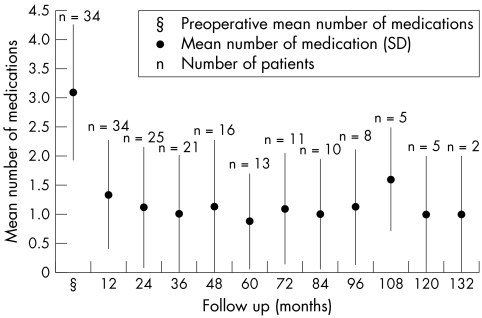
The mean (SD) number of glaucoma and steroid medications being used preoperatively was 3.1 (1.2). At the end of the first year the mean (SD) number of medications had dropped to 1.3 (0.9) and fluctuated between 0.8 and 1.6 for the duration of follow up (fig 7).
Figure 7 Mean number of medications versus time profile.
At the patient's last follow up visit the visual acuity outcomes, defined as a change of two or more Snellen lines, were improved in 15.6%, unchanged in 62.5%, and worse in 21.9% when compared to their preoperative visual acuities.
There were no intraoperative complications. In the immediate postoperative period (<1 month) complications included two cases of flat AC, two cases of hyphaema, and one case of hypotony requiring reformation of the AC and tying off of the Molteno tube. Other complications are listed in table 2, the most frequent complication being corneal decompensation which required corneal grafting in four cases. No cases of cornea tube touch were noted. Breakdown of the conjunctiva over the Molteno plate occurred in one patient 12 months postoperatively; it was unable to be repaired and this implant was removed and resited in another quadrant. There was no erosion of the conjunctiva overlying the tube portion of the Molteno implants or tube migration in any patient in the study.
Table 2 Complications.
| Complication | Number of patients (%) |
|---|---|
| Tube related | |
| Corneal decompensation | 7 (20.6%) |
| Corneal graft failure | 2 (5.9%) |
| Corneal ulcer/abscess | 2 (5.9%) |
| Significant hyphaema | 2 (5.9%) |
| Cataract | 2 (5.9%) |
| Tube obstruction | 1 (2.9%) |
| Eroded plate | 1 (2.9%) |
| IOP related | |
| Flat anterior chamber | 2 (5.9%) |
| Hypotony | 2 (5.9%) |
Discussion
Since the introduction of Molteno implants there have been modifications to the device and improvements to the surgical implantation technique. To overcome the complication of conjunctival erosion leading to tube exposure and the associated risk of endophthalmitis,7 scleral flaps and donor scleral grafts are used by most surgeons.4,8 Sclera and dura are no longer available in the United Kingdom owing to the risk of CJD and variant CJD.5,9 The simplified technique described in this paper successfully eliminates the need for a donor scleral graft and decreases the required operating time. The surgical manoeuvres required in this technique are familiar to anterior segment surgeons and similar to those required in fashioning other glaucoma and cataract surgical wounds. Surgeons simply need to ensure that the entry point of the curved MVR blade into the nterior chamber is sited correctly and, most importantly, is parallel to the plane of the iris to minimise the risk of corneal endothelial touch.
Ozdamar et al described the use of a two step 10 mm scleral tunnel for the insertion of Krupin eye valve in six patients with a mean of 7 months' follow up.6 They observed a reduction in mean IOP without any conjunctival erosion or tube displacement. They proposed that a 10 mm scleral tunnel would improve stability and prevent migration of the tube; however, our experience suggests, for Molteno implants, a 5–6 mm scleral tunnel may be sufficient.
In the current series there was a significant reduction in the mean IOP following surgery, which was sustained over the duration of the follow up and was associated with a decrease in the number of glaucoma medications required. There were no intraoperative complications and no complications directly attributable to the lack of a scleral graft over the Molteno tube.
Postoperative complications of Molteno tube surgery are relatively common and the frequency and pattern of complications in this series are similar to previous reports (table 2).2,10 The most frequent complication, corneal decompensation (20.6%), is a well documented complication occurring after Molteno implantation.2,11,12 In a report published by Lim et al,2 which included cumulative complication rates, corneal decompensation was the most common postoperative complication, occurring in 14% of cases. Although the exact role implants have in corneal decompensation often remains undefined, Lim et al suggest it may result from suboptimal tissue compatibility and possibly micromotion from the tube element leading to corneal endothelial cell loss.2 Although not occurring in this series, some cases of corneal decompensation and graft failure have also been directly attributed to cornea tube touch.11
There was no displacement of the anterior tube or cases of conjunctival erosion in this series of patients over a mean follow up period of 49.9 months. The partial thickness of the scleral tunnel used in this technique proved sufficient to prevent conjunctival dehiscence and tube exposure. This outcome may be related to an absence of the immune mediated processes proposed for thinning and melting of full thickness patch grafts.3
Success rates for Molteno implants vary considerably and comparison of reported success rates is complicated by variation in definitions of success, differing cohorts of patients, and variable follow up. Of particular interest are papers based on long term follow up and that include life table analyses (table 3). Using strict definitions of success our qualified success rates of 70%, 60%, and 54% for the 1, 2, and 5 year follow up respectively, are similar to those in other series.10,12,13,14,15,16,17
Table 3 Success rates.
| Molteno | Investigator | Year | Diagnosis | Eyes | Mean follow up (months) | Definition of success | QS | |||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 year | 2 years | 5 years | 10 years | |||||||
| SP/DP | Leong | Mixed (32% neovascular) | 34 | 49.9 | 6<IOP<21 | 70 | 60 | 54 | ||
| SP | Heuer13 | 1992 | Mixed (non‐neovascular) | 50 | 14.9 | 6⩽IOP⩽21 | 55 | 46 | – | – |
| DP | Heuer13 | 1992 | Mixed (non‐neovascular) | 51 | 16.4 | 6⩽IOP⩽21 | 86 | 71 | – | – |
| SP | Mermoud14 | 1993 | Neovascular | 60 | 24.7 | IOP⩽21 | 62 | 53 | 10 | |
| SP/DP | Mills12 | 1996 | Mixed (26% neovascular) | 77 | 44† | IOP⩽22 | 88* | 79* | 54 | – |
| SP/DP | Valimaki15 | 1998 | Mixed (17% neovascular) | 87 | 24 | 6<IOP<22 | 90 | 75 | 50‡ | – |
| SP/DP | Broadway10 | 2001 | Mixed (16% neovascular) | 119 | 43 | 6⩽IOP⩽22 | 79* | 70* | 57* | 34* |
| SP/DP | Molteno16 | 2001 | Uveitis | 40 | 85.2 | 6<IOP⩽21 | 95 | 87 | 87 | 77 |
| DP | Ayyala17 | 2002 | Mixed (17% neovascular) | 30 | 21.2 | 4<IOP<22 | 73 | 56 | – | – |
SP, single Molteno plate; DP, double Molteno plate; QS, qualified success. IOP control with or without medications, *Values extrapolated directly from Kaplan‐Meier Curves where exact values not stated, †Median follow up (months), ‡Value at 4.5 years.
This study describes a simplified alternative surgical technique for the insertion of Molteno implants. The main advantage of this technique is that it successfully eliminates the requirement for a donor scleral graft and therefore the potential for transmission of CJD and other infections. The technique is not associated with additional intraoperative or postoperative complications and the implant continues to provide equivalent IOP control in the first 5 postoperative years based on comparison with other series in the literature.
Acknowledgements
We thank associate professor Val Gebski, head of biostatistics and research methodology, NHMRC Clinical Trials Centre, for assistance with the statistical analysis.
Abbreviations
CCAG - chronic closed angle glaucoma
GEE - generalised estimating equations
ICE - iridocorneal endothelial
IOP - intraocular pressure
MVR - microvitreoretinal
PKPG - penetrating keratoplasty
POAG - primary open angle glaucoma
vCJD - variant Creutzfeldt‐Jakob disease
Footnotes
Competing interests: none declared
Ethics approval: Ethics approval for this study was obtained from the Royal Prince Alfred Hospital Ethics Review Committee, Camperdown, Sydney, Australia.
References
- 1.Molteno A C. New implant for drainage in glaucoma: clinical trial. Br J Ophthalmol 196953606–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lim K S, Allan B D, Lloyd A W.et al Glaucoma drainage devices; past, present, and future. Br J Ophthalmol 1998821083–1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith M F, Doyle J W, Ticrney J W., Jr A comparison of glaucoma drainage implant tube coverage. J Glaucoma 200211143–147. [DOI] [PubMed] [Google Scholar]
- 4.Freedman J. Scleral patch grafts with Molteno setons. Ophthalmic Surg 198718532–534. [PubMed] [Google Scholar]
- 5.Mehta J S, Franks W A. The sclera, the prion, and the ophthalmologist. Br J Ophthalmol 200286587–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ozdamar A, Aras C, Ustundag C.et al Scleral tunnel for the implantation of glaucoma seton devices. Ophthalmic Surg Lasers 200132432–435. [PubMed] [Google Scholar]
- 7.Krebs D B, Liebmann J M, Ritch R.et al Late infectious endophthalmitis from exposed glaucoma setons. Arch Ophthalmol 1992110174–175. [DOI] [PubMed] [Google Scholar]
- 8.Molteno A C, Straughan J L, Ancker E. Long tube implants in the management of glaucoma. S Afr Med J 1976501062–1066. [PubMed] [Google Scholar]
- 9.Armitage W J. Scleral substitutes: a cautionary note. Br J Ophthalmol 2002861459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Broadway D C, Iester M, Schulzer M.et al Survival analysis for success of Molteno tube implants. Br J Ophthalmol 200185689–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lloyd M A, Sedlak T, Heuer D K.et al Clinical experience with the single‐plate Molteno implant in complicated glaucomas: update of a pilot study. Ophthalmology 199299679–687. [DOI] [PubMed] [Google Scholar]
- 12.Mills R P, Reynolds A, Emond M J.et al Long‐term survival of Molteno glaucoma drainage devices. Ophthalmology 1996103299–305. [DOI] [PubMed] [Google Scholar]
- 13.Heuer D K, Lloyd M A, Abrams D A.et al Which is better? One or two?: a randomized clinical trial of single‐plate versus double‐plate Molteno implantation for glaucomas in aphakia and pseudophakia. Ophthalmology 1992991512–1519. [DOI] [PubMed] [Google Scholar]
- 14.Mermoud A, Salmon J F, Alexander P.et al Molteno tube implantation for neovascular glaucoma: long term results and factors influencing the outcome. Ophthalmology 1993100897–902. [PubMed] [Google Scholar]
- 15.Valimaki J, Tuulonen A, Airaksinen P J. Outcome of Molteno implantation surgery in refractory glaucoma and the effect of total and partial tube ligation on the success rate. Acta Ophthalmol Scand 199876213–219. [DOI] [PubMed] [Google Scholar]
- 16.Molteno A C, Sayawat N, Herbison P. Otago glaucoma surgery outcome study: long‐term results of uveitis with secondary glaucoma drained by Molteno implants. Ophthalmology 2001108605–613. [DOI] [PubMed] [Google Scholar]
- 17.Ayyala R S, Zurakowski D, Monshizadeh R.et al Comparison of double‐plate Molteno and Ahmed glaucoma valve in patients with advanced uncontrolled glaucoma. Ophthalmic Surg Lasers 20023394–101. [PubMed] [Google Scholar]