Abstract
Aim
To determine the prevalence of the met and unmet need for spectacles and their associated factors in the population of Tehran.
Methods
6497 Tehran citizens were enrolled through random cluster sampling and were invited to a clinic for an interview and ophthalmic examination. 4354 (70.3%) participated in the survey, and refraction measurement results of 4353 people aged 5 years and over are presented. The unmet need for spectacles was defined as the proportion of people who did not use spectacles despite a correctable visual acuity of worse than 20/40 in the better eye.
Results
The need for spectacles in the studied population, standardised for age and sex, was 14.1% (95% confidence interval (CI), 12.8% to 15.4%). This need was met with appropriate spectacles in 416 people (9.3% of the total sample), while it was unmet in 230 people, representing 4.8% of the total sample population (95% CI, 4.1% to 5.4%). The spectacle coverage rate (met need/(met need + unmet need)) was 66.0%. Multivariate logistic regression showed that variables of age, education, and type of refractive error were associated with lack of spectacle correction. There was an increase in the unmet need with older age, lesser education, and myopia.
Conclusion
This survey determined the met and unmet need for spectacles in a Tehran population. It also identified high risk groups with uncorrected refractive errors to guide intervention programmes for the society. While the study showed the unmet need for spectacles and its determinants, more extensive studies towards the causes of unmet need are recommended.
Keywords: spectacle coverage, uncorrected refractive error, cross sectional study
Refractive errors are the fourth leading cause of blindness and, in many areas, they are the second cause of curable blindness, with cataract standing first, and are one of the most common causes of visual impairment.1 In light of its burden on the society and the remedy, refractive errors are one of the five priorities of the global initiative for elimination of avoidable blindness, Vision 2020, launched by the World Health Organization (WHO) and the International Agency for Prevention of Blindness.2 In addition to studies on the prevalence of refractive errors in different groups of various populations, some studies have focused on the role of refractive errors on visual impairment and have found that a significant percentage of visual impairment and blindness is attributable to refractive errors, especially in developing countries.1 A number of studies have shown that a considerable number of people with miscorrected vision can benefit from more appropriate corrections; this issue is considerable in developed countries, especially among particular groups such as elderly people or minority groups.3,4,5,6,7 The Baltimore Eye Study showed that with proper correction, the visual acuity increased by at least one line in 54% of people, and 7.5% could experience an increase of three lines or more.7 Visual impairment has been reported to be associated with higher rates of morbidity and mortality; in particular, uncorrected refractive errors increase morbidity.8,9,10,11,12 The onset age of refractive errors suggests that their burden, defined as person years affected by visual impairment or blindness, can be even greater than that of cataract.1 The global increase in prevalence of myopia may further add to the burden of refractive errors.13
The prevalence rates of refractive errors in Tehran have been reported previously.14 Based on the presenting vision and the definition of a visual acuity worse than 20/60 in the better eye, refractive errors are the second leading cause of visual impairment in Tehran.15 Considering the role of refractive errors in visual impairment despite their simple cure, we present in this report the prevalence of uncorrected refractive errors in a Tehran population, the met and unmet need for spectacles, and their associated factors such as age, sex, and education.
Materials and methods
The Tehran Eye Study is a cross sectional survey whose detailed methodology has been published.15,16 The survey was conducted by random cluster sampling in Tehran. Selected samples were invited to a clinic for an interview and eye visit in a door to door approach. All participants underwent complete ophthalmic examinations including measurement of visual acuity; lensometry; objective, subjective, and cycloplegic refraction; measurement of intraocular pressure; a slit lamp examination; and funduscopy.
Myopia was defined as a spherical equivalent refraction of −0.5 dioptre (D) or more. For further analysis, myopia was classified in three groups: mild (−0.5 to −3.0D), moderate (>−3.0 to −6.0D), and severe (>−6.0D). A spherical equivalent refraction of +0.5D or more was defined as hyperopia, and one between −0.5 and +0.5D was considered emmetropia. Likewise, three groups were assigned for hyperopia: mild (+0.5 to +2.0D), moderate (>2.0 to +4.0D), and severe (>+4.0D). A cylinder refraction greater than 0.5D was taken for astigmatism. Since the spherical equivalent refraction in the right and left eyes was highly correlated (r = 0.84, p<0.001), the refractive results of the right eyes were used to determine the type of refractive errors.
To determine the spectacle coverage, we used the definitions and equations presented by Bourne and colleagues.17 “Met need” for spectacles was defined as the number of subjects who wore spectacles and had visual acuity worse than 20/40 in the better eye without correction, but achieved 20/40 or better with their present spectacles. “Unmet need” was defined as the number of subjects who had a visual acuity worse than 20/40 in the better eye without correction and could achieve 20/40 or better in the better eye with correction, but either went without spectacles or did not achieve such correction with their present spectacles. With these definitions, spectacle coverage would be:
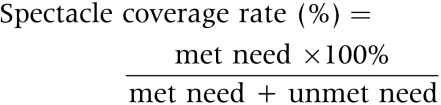 |
In the data analysis, the 95% confidence interval (CI) and standard error were computed considering the design effect, and results were adjusted for. All rates were directly standardised for age and sex according to the 1996 national census.18 Multivariate logistic regression was used to identify variables affecting the rate of spectacle utilisation and unmet need.
The study protocol and all the questionnaires were approved by the corresponding institutional review boards of the Noor Vision Correction Centre and the National Medical Research Centre of Iran. All participants provided informed consent.
Results
During the study period from July to November 2002, 4565 of the 6497 eligible people participated and had the interview and examinations (participation rate, 70.3%). The age and sex distribution of the participants was slightly different from that of the total city population; those under 10 years or over 40 years of age showed a higher rate of participation. For this reason, age and sex standardisation based on the 1996 national census was applied for calculating ratios. Here we present our findings pertaining to 4354 participants who were 5 years of age or older. In this group, the mean age was 31.4 years, ranging from 5–95 years. There were 1812 males, accounting for 41.6%, and 2542 females (58.4%).
A need for spectacles was identified in 646 participants. The age and sex standardised rate of spectacle need in the studied population was 14.1% (95% CI, 12.8% to 15.4%). In the studied sample, 416 people, accounting for 9.3% (95% CI, 8.2% to 10.4%), used appropriate spectacles for their need (met need), while 230 others, accounting for 4.8% (95% CI, 4.1% to 5.4%) had an unmet need because they either used no spectacles or did not wear appropriate ones. Therefore, the spectacle coverage rate in the total studied population was 66.0%, leaving 34.0% with an unmet need. Table 1 presents the rates of spectacle coverage, met need, and unmet need categorised in groups of age, sex, education, ethnicity, and type of refractive error. Univariate analyses showed that all investigated variables, except sex, were significantly associated with the participants' unmet need (table 1). The adjusted effect of these variables on the unmet need was assessed in a multivariate logistic regression analysis, results of which are summarised in table 2. In the final model, sex and ethnicity showed no significant association with unmet need, while age, education, and type of refractive error did; an unmet need was more likely with an increase in age, decrease in education, and myopia (table 2). Among different types of refractive error, the greatest likelihood for an unmet need was found with myopia followed by hyperopia, while the association with astigmatism, although significant, was the weakest.
Table 1 Spectacle coverage rate and the prevalence (95% CI) of met and unmet need for spectacles according to sex, age, education, ethnicity, and type of refractive error*.
| Number | Met need | Unmet need | Spectacle coverage (%) | p Value | |
|---|---|---|---|---|---|
| Age groups (years) | <0.001 | ||||
| 5–15 | 1021 | 3.6 (2.5 to 4.8) | 2.1 (1.3 to 2.9) | 63.2 | |
| 16–25 | 982 | 12.7 (10.3 to 15.1) | 3.6 (2.5 to 4.7) | 77.9 | |
| 26–35 | 642 | 8.1 (5.3 to 10.9) | 3.3 (2.0 to 4.6) | 77.1 | |
| 36–45 | 644 | 9.5 (7.2 to 11.8) | 3.4 (1.9 to 4.8) | 73.6 | |
| 46–55 | 536 | 12.4 (9.5 to 15.3) | 8.4 (6.0 to 10.8) | 59.6 | |
| 56 and over | 492 | 15.5 (11.9 to 19.1) | 16.2 (12.6 to 19.8) | 48.9 | |
| Sex | 0.254 | ||||
| Male | 1796 | 8.8 (7.4 to 10.3) | 4.1 (3.2 to 4.9) | 68.2 | |
| Female | 2521 | 9.9 (8.5 to 11.2) | 5.5 (4.6 to 6.5) | 64.3 | |
| Education | <0.001 | ||||
| None | 265 | 4.4 (2.1 to 6.7) | 19.3 (14.0 to 24.6) | 18.6 | |
| Up to 5 years | 781 | 5.3 (3.6 to 7.0) | 3.8 (2.4 to 5.1) | 58.2 | |
| 6–12 years | 2435 | 9.1 (7.8 to 10.3) | 4.4 (3.6 to 5.2) | 67.4 | |
| Over 12 years | 684 | 17.6 (14.2 to 21.0) | 3.5 (2.2 to 4.9) | 83.4 | |
| Ethnicity | <0.001 | ||||
| Persian | 3466 | 9.6 (8.4 to 10.8) | 4.4 (3.7 to 5.1) | 68.6 | |
| Turk | 697 | 7.7 (5.4 to 10.1) | 6.4 (4.3 to 8.4) | 54.6 | |
| Armenian | 57 | 13.6 (2.7 to 24.5) | 3.8 (0.3 to 9.4) | 78.2 | |
| Other | 82 | 8.0 (3.9 to 12.0) | 8.7 (2.6 to 14.8) | 47.9 | |
| Refractive error | <0.001 | ||||
| Myopia | 931 | 33.6 (30.2 to 37.1) | 12.7 (11.4 to 14.9) | 72.6 | |
| Hyperopia | 1133 | 7.2 (5.6 to 8.8) | 6.5 (5.1 to 7.9) | 52.6 | |
| Astigmatism | 1293 | 18.2 (16.0 to 20.4) | 9.9 (8.2 to 11.5) | 64.8 | |
| Total | 4317 | 9.3 (8.2 to 10.4) | 4.8 (4.1 to 5.4) | 66.0 |
*Standardised for age and sex based on the 1996 national census.
Table 2 Multivariate logistic model for “unmet need”.
| Independent variables | Odds ratio (95% CI) |
|---|---|
| Age (years) | |
| 5–15 | 1 |
| 16–25 | 1.09 (0.64 to 1.85) |
| 26–35 | 0.99 (0.53 to 1.88) |
| 36–45 | 1.04 (0.54 to 1.95) |
| 46–55 | 2.05 (1.17 to 3.60) |
| 56 and over | 3.17 (1.78–5.64) |
| Education | |
| None | 1 |
| Up to 5 years | 0.37 (0.20 to 0.71) |
| 6–12 years | 0.44 (0.26 to 0.75) |
| Over 12 years | 0.27 (0.15 to 0.51) |
| Type of refractive error | |
| None | 1 |
| Myopia | 18.67 (9.09 to 38.37) |
| Hyperopia | 7.94 (4.20 to 15.01) |
| Astigmatism | 1.61 (1.17 to 2.22) |
Table 3 shows the improvement in the participants' vision achievable by correcting their uncorrected or miscorrected refractive errors. Using appropriate spectacles improved the visual acuity by at least one line in 26.7% of the studied population and as much as four lines or more in 5.9% (95% CI, 5.2% to 6.7%). These figures were more pronounced among participants with visual impairment. According to definition, 349 participants (7.1%) were visually impaired with a visual acuity worse than 20/40 in the better eye, 62.0% of which (95% CI, 57.1% to 66.8%) could experience a four line improvement in vision by wearing proper spectacles. Among these people, 230 (56.9%) visually recovered by wearing proper spectacles and could improve their visual acuity to better than 20/40. The presenting visual acuity was worse than 20/20 in the better eye of 1163 participants (24.4%), among which 23.7% could gain four lines of visual acuity with accurately prescribed spectacles.
Table 3 Visual improvement after correcting refractive errors*.
| Gained lines | % (95% CI) | ||
|---|---|---|---|
| Presenting vision worse than 20/40 in the better eye (n = 349) | ⩾1 line | 81.9 (77.7 to 86.1) | |
| ⩾2 lines | 76.1 (71.6 to 80.1) | ||
| ⩾3 lines | 71.1 (66.4 to 75.7) | ||
| ⩾4 lines | 62.0 (57.1 to 66.8) | ||
| Presenting vision worse than 20/20 in the better eye (n = 1163) | ⩾1 line | 85.8 (83.7 to 87.9) | |
| ⩾2 lines | 58.9 (55.8 to 61.9) | ||
| ⩾3 lines | 38.4 (35.2 to 41.7) | ||
| ⩾4 lines | 23.7 (21.0 to 26.3) | ||
| Total (n = 4317) | ⩾1 line | 26.7 (25.1 to 28.3) | |
| ⩾2 lines | 16.5 (15.1 to 17.8) | ||
| ⩾3 lines | 10.1 (9.1 to 11.2) | ||
| ⩾4 lines | 5.9 (5.2 to 6.7) |
*Standardised for age and sex based on the 1996 national census.
Discussion
Refractive errors and low vision are one of the five priorities of the global initiative for elimination of avoidable blindness, Vision 2020.2 Today they are gaining more attention, and many studies have shown that a considerable percentage of cases with low vision are the result of miscorrected refractive errors.1 The importance of this issue was further revealed when the effect of visual impairment and low vision on morbidity and mortality was identified in certain studies.8,9,10,11,12 Studies concerning spectacle utilisation rates and correct prescriptions among different communities are based on these grounds.3,4,5,6,7,17,19,20,21
Results of the present study show that over one third of those who need spectacles did not have appropriate ones, and over one fourth of them could experience visual improvement with proper correction of their refractive errors. This was a substantial issue among the visually impaired; vision could be improved in over four fifths of these people, and two thirds could gain four or more lines of visual acuity. In addition, this study determined the roles of age, education, and type of refractive error, revealed the significant prevalence of uncorrected refractive errors, and also showed that eye care services were underutilised.
The definition used for calculating the spectacle coverage rate in this study has been suggested by Bourne and colleagues.17 This definition focuses on those who need visual correction and have proper spectacles. It also determines what proportion of all those who need correction to achieve acceptable visual improvement (better than 20/40) have received prescription glasses. This is not a comprehensive definition, because there are people with correct spectacles who cannot achieve such corrections because of other eye problems, and so do not fit in the “met need” category. The number of such cases is of course too limited to alter results. On the other hand, the definition overlooks the role of spectacles in improving visions better than 20/40; this shortcoming has somewhat been addressed in a different analysis (table 3). According to the report by Bourne et al,17 the spectacle coverage rate in a Bangladesh rural and urban population ⩾30 years of age was 25.2%. This rate is much smaller than our finding, although comparing results would be difficult because our sample population was an urban one with a wider age range. Still the problem is also considerable in our studied population.
The rate of uncorrected refractive errors in this study was 7.1%. Other studies on different populations have reported various rates. In a review, Dandona et al1 stated that, according to different reports, the rate of blindness caused by uncorrected refractive errors was 0.2% up to 1.06% in a population of over 40 year olds in India.
Uncorrected refractive errors are also considered a serious issue in developed countries. In one study on Australian adults, uncorrected refractive errors were accountable for, respectively, 25% and 56% of cases of visual loss and visual impairment.22 The rate of uncorrected refractive errors in the over 40 year old Australian population has been reported to be 10.2% and 10.0% in two separate studies.3,5 The Baltimore Eye Study showed that correcting refractive errors increases the visual acuity by at least one line in 54% of people, among whom 7.5% could experience a gain of three lines or more.7 In another study in Australia, at least one line of visual improvement with correct prescriptions was seen in 45% of people who had a presenting vision worse than 20/20, and 13% gained three lines or more.6 A study in Chile found that proper spectacles could improve vision in 7% of children, and in 56% of these cases, poor vision was the result of refractive errors.23 All these reports stress the importance and role of uncorrected refractive errors in societies and the necessity to observe them. In Australia, “off the shelf” spectacles have been proposed for dealing with this issue, and they found that 20% of the 40–60 year age range make use of them.19
The present study had certain limitations, which must be mentioned. Firstly, despite an acceptable participation rate (70.3%), it is likely that the computed rate of spectacle coverage and unmet need differs from that in the total Tehran population. Secondly, the reasons for an unmet need were not determined. It was not clear if lack of correct prescriptions was because of lack of accessibility, knowledge, need, or other reasons. Regarding the extent of the issue, further studies can be enlightening. Thirdly, the sample population of the study does not represent the nation in terms of socioeconomic characteristics, therefore, although unique and providing valuable information, results of this study cannot be generalised to the whole country. It is advisable to carry out similar studies in other areas of the country. Fourthly, need for spectacles to correct presbyopia was not assessed; studies addressing this issue are also necessary.
Conclusion
The present study revealed that a substantial proportion of the population lack proper spectacles for correcting their refractive error, while a considerable percentage would greatly benefit from them. In addition, it showed that an unmet need was more likely among the elderly, less educated, and myopes, although reasons behind its high rate were not identified. In short, the importance of spectacles, as a simple and inexpensive solution, should not be overlooked in correcting poor vision in Tehran.
Acknowledgements
This project was funded in part by the Noor Vision Correction Centre and a grant from the Iranian National Research Centre for Medical Sciences. The random selection of clusters was performed by the Iranian Statistics Centre based on the 1996 national census.
Footnotes
Competing interests: none of the authors has a proprietary interest in any products mentioned in this study.
References
- 1.Dandona R, Dandona L. Refractive error blindness. Bull World Health Organ 200179237–243. [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Vision 2020. Global initiative for the elimination of avoidable blindness. Fact Sheet No 1213. Geneva: WHO, 2000
- 3.Thiagalingam S, Cumming R G, Mitchell P. Factors associated with undercorrected refractive errors in an older population: the Blue Mountains Eye Study. Br J Ophthalmol 2002861041–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Munoz B, West S K, Rodriguez J.et al Blindness, visual impairment and the problem of uncorrected refractive error in a Mexican American population: Proyecto VER. Invest Ophthalmol Vis Sci 200243608–614. [PubMed] [Google Scholar]
- 5.Liou H, Mccarty C A, Jin C L.et al Prevalence and predictors of undercorrected refractive errors in the Victorian population. Am J Ophthalmol 1999127590–596. [DOI] [PubMed] [Google Scholar]
- 6.Attebo K, Mitchell P, Smith W. Visual acuity and the causes of visual loss in Australia. Ophthalmology 1996103357–364. [DOI] [PubMed] [Google Scholar]
- 7.Tielsch J, Sommer A, Witt K.et al Blindness and visual impairment in an American urban population. Arch Ophthalmol 1990108286–290. [DOI] [PubMed] [Google Scholar]
- 8.Klein B E, Klein R, Lee K E.et al Performance‐based and self‐assessed measures of visual function as related to history of falls, hip fractures, and measured gait time. The Beaver Dam Eye Study. Ophthalmology 1998105160–164. [DOI] [PubMed] [Google Scholar]
- 9.Ivers R Q, Norton R, Cumming R G.et al Visual impairment and risk of hip fracture. Am J Epidemiol 2000152633–639. [DOI] [PubMed] [Google Scholar]
- 10.Wang J J, Mitchell P, Simpson J.et al Visual impairment, age‐related cataract, and mortality. Arch Ophthalmol 20011191186–1190. [DOI] [PubMed] [Google Scholar]
- 11.McCarty C A, Nanjan M B, Taylor H R. Vision impairment predicts 5 year mortality. Br J Ophthalmol 200185322–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klein R, Klein B E K, Moss S E. Age related eye disease and survival. The Beaver Dam Eye Study. Arch Ophthalmol 1995113333–339. [DOI] [PubMed] [Google Scholar]
- 13.Holden B A, Resnikoff S. The role of optometry in Vision 2020. Community Eye Health 20021533–36. [PMC free article] [PubMed] [Google Scholar]
- 14.Hashemi H, Fotouhi A, Mohammad K. The age and gender specific prevalences of refractive errors in Tehran: the Tehran Eye Study. Ophthalmic Epidemiol 200411213–225. [DOI] [PubMed] [Google Scholar]
- 15.Fotouhi A, Hashemi H, Mohammad K.et al The prevalence and causes of visual impairment in Tehran: the Tehran Eye Study. Br J Ophthalmol 200488740–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hashemi H, Fotouhi A, Mohammad K. Tehran Eye Study: research design and eye examination protocol. BMC Ophthalmol 200383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bourne R R A, Dineen B P, Noorul Huq D M.et al Correction of refractive error in the adult population of Bangladesh: meeting the unmet need. Invest Ophthalmol Vis Sci 200445410–417. [DOI] [PubMed] [Google Scholar]
- 18.Iranian Statistics Center The report of the 1996 population census. http://amar.sci.or.ir (10 March 2003)
- 19.Maini R, Keeffe J, Weih L A.et al Correction of refractive error in the Victorian population: the feasibility of “off the shelf” spectacles. Br J Ophthalmol 2001851283–1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dandona R, Dandona L, Naduvilath T J.et al Refractive errors in an urban population in Southern India: the Andhra Pradesh Eye Disease Study. Invest Ophthalmol Vis Sci 1999402810–2818. [PubMed] [Google Scholar]
- 21.Dandona R, Dandona L, Kovai V.et al Population‐based study of spectacles use in southern India. Indian J Ophthalmol 200351107–108. [PubMed] [Google Scholar]
- 22.Taylor H R, Livingston P M, Stanislavsky Y L.et al Visual impairment in Australia: distance visual acuity, near vision and visual field findings of the Melbourne Vision Impairment Unit. Am J Ophthalmol 1997123328–337. [DOI] [PubMed] [Google Scholar]
- 23.Maul E, Barroso S, Munoz S R.et al Refractive error study in children: results from La Florida, Chile. Am J Ophthalmol 200029445–454. [DOI] [PubMed] [Google Scholar]


