Abstract
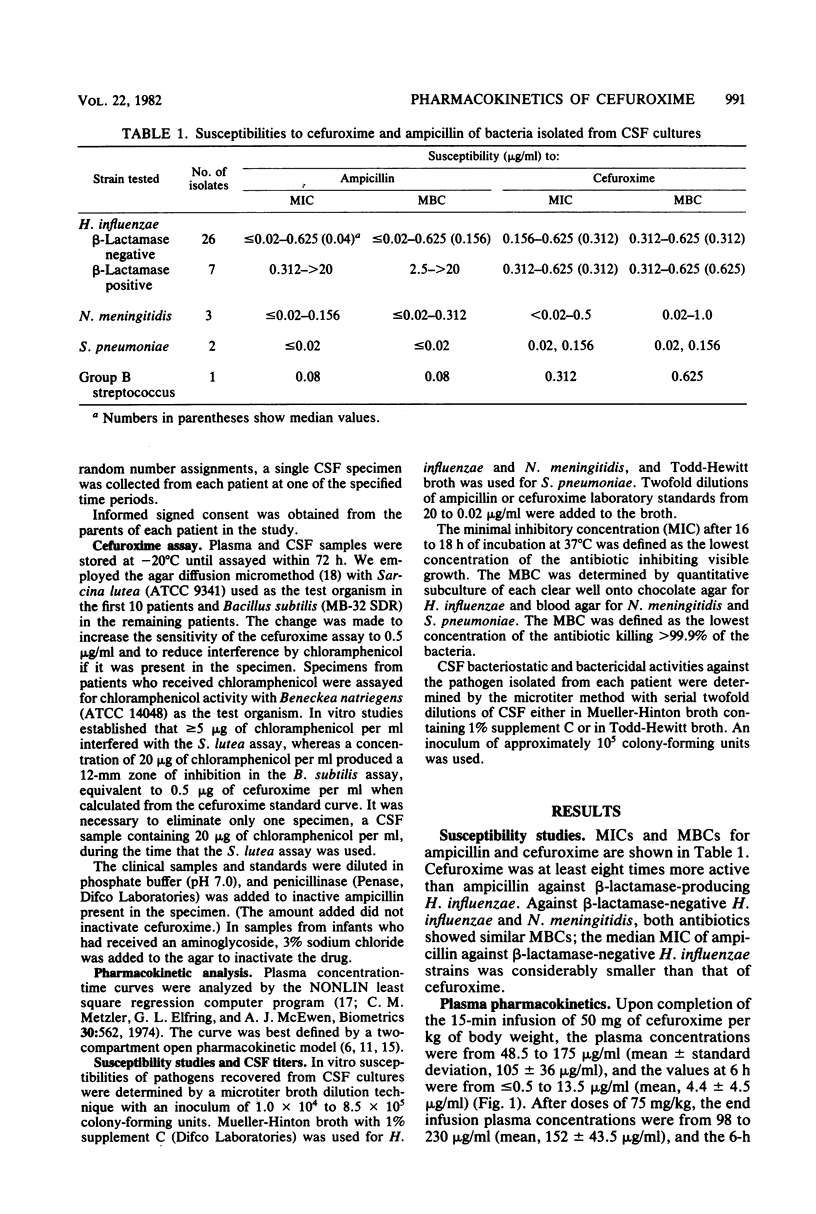
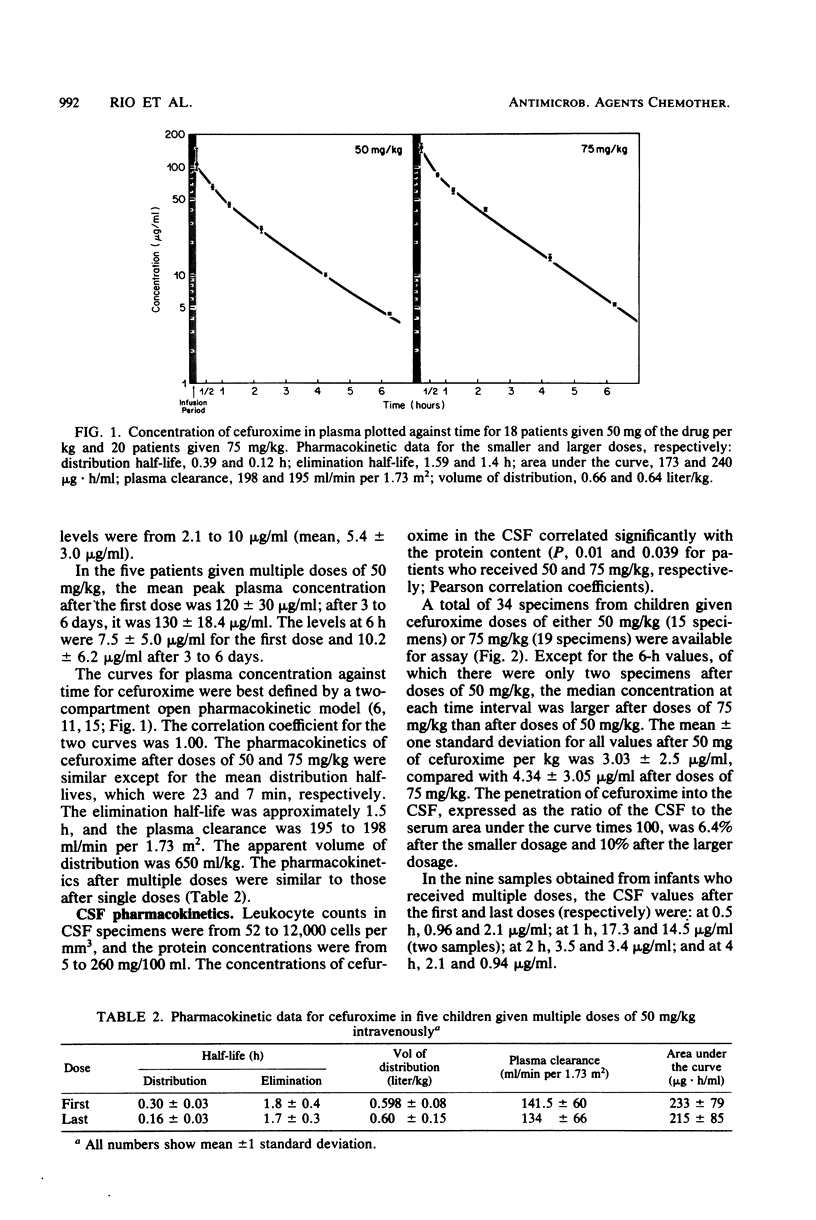
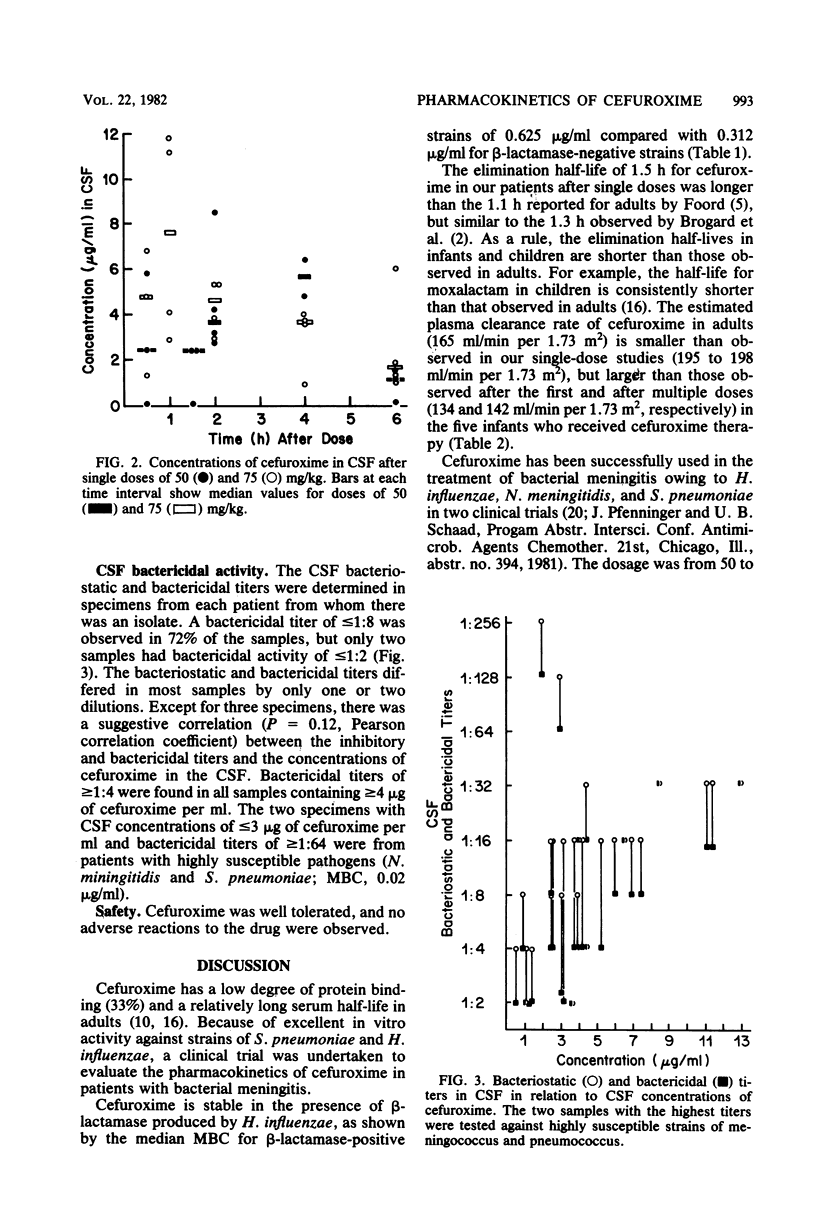
A total of 38 patients with bacterial meningitis received either 50 or 75 mg of cefuroxime per kg of body weight given as a 15-min intravenous infusion during the first to third days of therapy. The mean peak plasma concentrations of cefuroxime after doses of 50 and 75 mg/kg were 105 and 152 micrograms/ml, respectively. In five patients, pharmacokinetic values were determined after multiple doses of 50 mg of cefuroxime per kg every 6 h. The mean peak plasma concentrations were 120 micrograms/ml after the first dose and 130 micrograms/ml after the last dose. The concentrations at 6 h were 3.25 and 11.0 micrograms/ml after the first and last doses, respectively. The elimination half-life was approximately 1.5 h, and the apparent volume of distribution was 650 ml/kg. The plasma clearance rate was 195 to 198 ml/min per 1.73 m2. Penetration into the cerebrospinal fluid, expressed as the ratio of the cerebrospinal fluid to serum areas under the curve times 100, was 6.4% in patients given 50 mg of cefuroxime per kg and 10% in those who received 75 mg/kg. The cerebrospinal bactericidal activity in 27 patients was less than or equal to 1:8; only 2 patients had bactericidal activity of less than or equal to 1:2.
Full text
PDF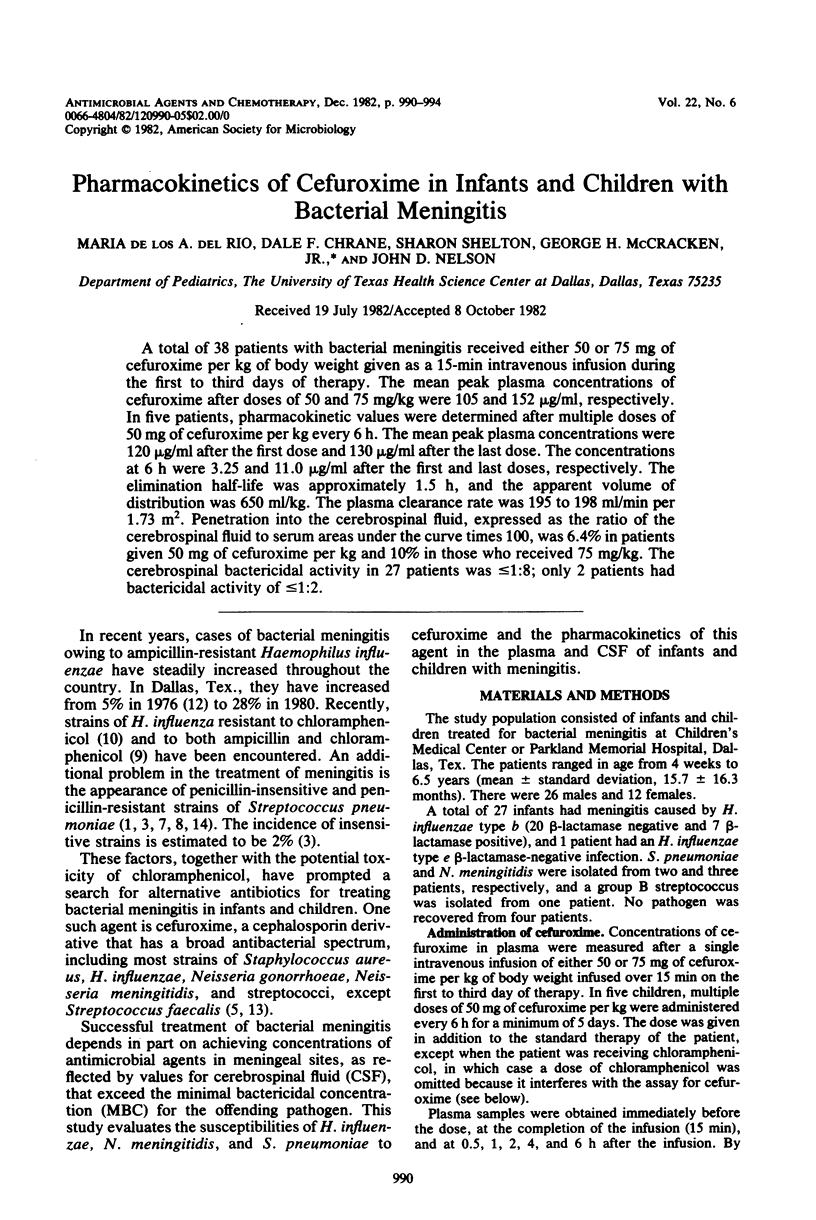
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahronheim G. A., Reich B., Marks M. I. Penicillin-insensitive pneumococci. Case report and review. Am J Dis Child. 1979 Feb;133(2):187–191. doi: 10.1001/archpedi.1979.02130020079017. [DOI] [PubMed] [Google Scholar]
- Fisher L. S., Chow A. W., Yoshikawa T. T., Guze L. B. Cephalothin and cephaloridine therapy for bacterial meningitis. Ann Intern Med. 1975 May;82(5):689–693. doi: 10.7326/0003-4819-82-5-689. [DOI] [PubMed] [Google Scholar]
- Foord R. D. Cefuroxime: human pharmacokinetics.. Antimicrob Agents Chemother. 1976 May;9(5):741–747. doi: 10.1128/aac.9.5.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansman D., Glasgow H., Sturt J., Devitt L., Douglas R. Increased resistance to penicillin of pneumococci isolated from man. N Engl J Med. 1971 Jan 28;284(4):175–177. doi: 10.1056/NEJM197101282840403. [DOI] [PubMed] [Google Scholar]
- Kenny J. F., Isburg C. D., Michaels R. H. Meningitis due to Haemophilus influenzae type b resistant to both ampicillin and chloramphenicol. Pediatrics. 1980 Jul;66(1):14–16. [PubMed] [Google Scholar]
- Kinmonth A. L., Storrs C. N., Mitchell R. G. Meningitis due to chloramphenicol-resistant Haemophilus influenzae type b. Br Med J. 1978 Mar 18;1(6114):694–694. doi: 10.1136/bmj.1.6114.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naraqi S., Kirkpatrick G. P., Kabins S. Relapsing pneumococcal meningitis: isolation of an organism with decreased susceptibility to penicillin G. J Pediatr. 1974 Nov;85(5):671–673. doi: 10.1016/s0022-3476(74)80513-5. [DOI] [PubMed] [Google Scholar]
- doi: 10.1177/00359157770700S901. [DOI] [PMC free article] [Google Scholar]
- Schaad U. B., McCracken G. H., Jr, Threlkeld N., Thomas M. L. Clinical evaluation of a new broad-spectrum oxa-beta-lactam antibiotic, moxalactam, in neonates and infants. J Pediatr. 1981 Jan;98(1):129–136. doi: 10.1016/s0022-3476(81)80559-8. [DOI] [PubMed] [Google Scholar]
- Sedman A. J., Wagner J. G. CSTRIP, a fortran IV computer program for obtaining initial polyexponential parameter estimates. J Pharm Sci. 1976 Jul;65(7):1006–1010. doi: 10.1002/jps.2600650713. [DOI] [PubMed] [Google Scholar]
- Simon H. J., Yin E. J. Microbioassay of antimicrobial agents. Appl Microbiol. 1970 Apr;19(4):573–579. doi: 10.1128/am.19.4.573-579.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strausbaugh L. J., Mandaleris C. D., Sande M. A. Cefamandole and ampicillin therapy in experimental Haemophilus influenzae meningitis. J Infect Dis. 1977 Feb;135(2):210–216. doi: 10.1093/infdis/135.2.210. [DOI] [PubMed] [Google Scholar]
- Wilson H. D., Haltalin K. C. Ampicillin in Haemophilus influenzae meningitis. Clinicopharmacologic evaluation of intramuscular vs intravenous administration. Am J Dis Child. 1975 Feb;129(2):208–215. doi: 10.1001/archpedi.1975.02120390042009. [DOI] [PubMed] [Google Scholar]



