Abstract
Aim
To determine the complications associated with mitomycin C (MMC) in the treatment of ocular surface neoplasia.
Methods
A retrospective and consecutive study of 100 eyes in 91 patients with ocular surface neoplasia treated with MMC in a single centre between November 1998 and January 2005. Outcome measures included complications of MMC and the treatment required for these complications.
Results
One to three 7 day cycles of topical MMC 0.04% four times a day were given to 59 eyes with localised corneal‐conjunctival intraepithelial neoplasia (CIN), 19 eyes with diffuse CIN, six eyes with recurrent CIN, one eye with ocular surface squamous cell carcinoma, three eyes with primary acquired melanosis (PAM) with atypia, nine eyes with conjunctival malignant melanoma (MM), two eyes with sebaceous carcinoma with pagetoid spread, and one eye with recurrent atypical fibroxanthoma. Nine patients had bilateral CIN. 31 (34%) cases developed an allergic reaction to MMC and 14 (14%) eyes had epiphora secondary to punctal stenosis at a mean follow up period of 26.5 months.
Conclusion
In the largest study looking at complications of topical MMC in the treatment of ocular surface neoplasia, allergic reaction and punctal stenosis are relatively common. Serious complications were not observed suggesting the safe use of MMC in mid‐term follow up.
Keywords: mitomycin, eye neoplasms
Topical mitomycin C (MMC) has been well described for the treatment of corneal‐conjunctival intraepithelial neoplasia (CIN),1,2,3,4 primary acquired melanosis (PAM) with atypia,5,6,7 conjunctival malignant melanoma (MM),6,7 and pagetoid spread of sebaceous carcinoma.8
We present a large series of 100 eyes with ocular surface neoplasia treated with MMC either as primary or adjunctive therapy. The aim of this study was to determine the complications of MMC associated with the treatment of ocular surface neoplasia.
Methods
A retrospective and consecutive study was carried out of 100 eyes in 91 patients (67 males and 24 females) with ocular surface neoplasia receiving MMC therapy in a single centre between November 1998 and January 2005. Nine patients had bilateral CIN. There were 59 eyes with localised CIN, 19 eyes with diffuse CIN, six eyes with recurrent CIN, one eye with squamous cell carcinoma, three eyes with PAM with atypia, nine eyes with conjunctival melanoma, two eyes with sebaceous carcinoma, and one eye with recurrent atypical fibrous histiocytoma. All diagnoses were confirmed by histopathology. Cases were excluded if the follow up was less than 3 months.
Most patients were treated with MMC 0.04% four times a day using a week on and week off regimen. Treatment was only commenced after complete epithelial healing was achieved. Punctal plugs were not used during MMC treatment in any of our cases. The treatment in all cases was undertaken by a single ocular oncologist (JM). The treatment regimens for localised and diffuse CIN, diffuse PAM with atypia, and recurrent conjunctival MM are summarised in table 1. Patients from rural areas with difficult access to the treatment centre were treated with a continuous 2 week course of MMC. Two cases of sebaceous carcinoma had surgical excision and cryotherapy followed by three courses of adjunctive MMC. A single case of recurrent atypical fibrous histiocytoma was treated by three courses of MMC after primary surgical excision. MMC is not routinely used for the treatment of squamous cell carcinoma (SCC) in our centre, however a 1 week course of MMC was given in a patient following excision owing to a delay in the application of β radiotherapy.
Table 1 Summary of treatment regimen of ocular surface neoplasia.
| Treatment group | Treatment regimen | |
|---|---|---|
| Localised CIN | Excision and 0.04% MMC four times daily 2–3 weeks, 1 week on/1 week off | |
| Diffuse CIN | 0.04% MMC four times daily 3 weeks, 1 week on/1 week off | |
| Diffuse PAM with atypia | 0.04% MMC four times daily 3 weeks, 1 week on/1 week off | |
| Recurrent conjunctival MM | Excision and 0.04% MMC four times daily 3 weeks, 1 week on/1 week off |
Patients were examined in most cases 1 month and 3 months following completion of MMC treatment, then at 6 monthly intervals. Outcome measures included complications of MMC and the treatment required for these complications. Allergic reaction was defined clinically as marked pruritus in association with conjunctival and periocular erythema and oedema. Punctal stenosis was detected clinically with inspection of the punctum using slit lamp biomicroscopy. Probing and syringing of the nasolacrimal system was undertaken in all eyes with epiphora. Transient tearing, irritation, and conjunctival erythema were regarded as self limiting reactions and not complications of MMC.
Data were entered into an Excel database and analysed with SAS (SAS institute Inc, Cary, NC, USA) version 9.1. Binary outcomes were analysed using log binomial generalised estimating equation (GEE) allowing clustering of patients. A p value of <0.05 was considered significant.
Results
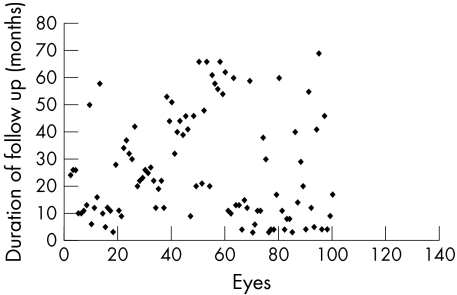
The mean duration of follow up was 26.5 months (range 3–69, median 20.5) (fig 1); 31 (34%) cases developed an allergic reaction towards MMC. Allergy occurred during the second (10) or third course (21) of MMC (table 2). In 19 of these cases, the particular week's course of MMC was completed. In the other 12 cases, MMC was immediately held because of poor tolerance towards the allergic symptoms. In all patients, the allergic symptoms and signs settled within a week with cold compresses and topical lubricants.
Figure 1 Distribution of duration of follow up of the 100 eyes with ocular surface neoplasia treated with MMC.
Table 2 Onset of allergic reaction by courses of MMC treatment.
| Allergy reaction | No of courses | Total (patients) | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| No | 1 | 31 | 28 | 60 |
| 100% | 77% | 57% | ||
| Yes | 0 | 10 | 21 | 31 |
| 0% | 24% | 43% | ||
| Total | 1 | 41 | 49 | 91 |
Fourteen eyes (14%) in 14 patients developed epiphora as a result of punctal stenosis after application of MMC. The mean duration from the first day of MMC treatment to the onset of epiphora was 1.9 months (range 0.75–4, median 1.75). Epiphora were reported by all patients at their first follow up review following completion of MMC. The appointment date rather than the exact date of onset of epiphora was used to calculate our results. The frequency of epiphora by the number of completed courses of MMC is presented in table 3. Twelve of the 14 patients did not have a previous history of epiphora. Two patients with pre‐existing epiphora due to ectropion and punctal stenosis noted worsening of their symptom following MMC treatment.
Table 3 Punctal stenosis by number of completed courses of MMC.
| Punctal stenosis | No of courses | Total (eyes) | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| No | 3 | 43 | 40 | 86 |
| 75% | 81% | 93% | ||
| Yes | 1 | 10 | 3 | 14 |
| 25% | 19% | 7% | ||
| Total | 4 | 53 | 43 | 100 |
Seven patients underwent dilatation and syringing of the punctum and five patients required a punctal one snip procedure to achieve resolution of the epiphora. One patient had persistent minor tearing despite syringing but was not troubled by the symptom, and one patient had persistent tearing after punctal snip that subsequently required dacro‐cystorhinostomy. The punctum in each patient remained patent throughout the follow up period. Using type 3 GEE analysis, an allergic reaction did not predict the occurrence of punctal stenosis (p>0.05).
One patient developed ptosis as a result of levator disinsertion attributed to allergy related lid oedema. At no stage was limbal stem cell deficiency, corneoscleral ulceration, iridocyclitis, cataract, or glaucoma observed in any of the patients.
Discussion
Before its use in ocular surface neoplasia, MMC had been widely used in glaucoma and pterygium surgery for its anti‐proliferative effect on subconjunctival fibroblasts. In 1994, Frucht‐Pery et al were credited for first using MMC in the treatment of corneal intraepithelial neoplasia.9 MMC has a few advantages in the treatment of ocular surface neoplasia. Unlike cryotherapy, it is a “whole eye” treatment, spreading to cover the entire ocular surface and reaching well into the fornices, thereby potentially eradicating subclinical new tumours on the ocular surface. MMC is considered a safe chemotherapeutic agent in treating ocular surface neoplasia. Transient side effects including tearing, ocular pain, blepharospasm, keratoconjunctivitis, conjunctival hyperaemia, and punctate epithelial keratopathy are common.1,4,6,8,9,10 Uncommon but significant complications such as limbal stem cell deficiency, focal corneal haze, cataract, excoriating dermatitis, and disciform keratitis have also been reported (table 4).2,6,7,11,12
Table 4 Summary of complications of MMC in studies utilising MMC for treating ocular surface malignancy.
| Study | Ocular surface malignancy | No of patients in study | Regimens of MMC | Complications of MMC | No of patients affected | |
|---|---|---|---|---|---|---|
| Frucht‐Pery et al9 | Corneal intraepithelial neoplasia | 3 | 0.02% MMC four times daily for 10–22 days | Conjuntival hyperaemiaOcular pain | 32 | |
| Blepharospasm | 1 | |||||
| Frucht‐Pery et al1 | Conjunctival‐corneal intraepithelial neoplasia | 17 | 0.02–0.04% MMC four times daily for 7–28 days | Ocular painConjunctival hyperaemia | 28 | |
| blepharospasm | 1 | |||||
| Allergy (probable) | 2 | |||||
| Heigle et al3 | Recurrent conjunctival epithelial neoplasia | 3 | 0.04% three times daily for 3 weeks, 1 week on/1 week off | Corneal oedema and epithelial toxicity | 1 | |
| Wilson et al4 | Conjunctival and corneal epithelial dysplasia and neoplasia | 7 | 0.04% MMC four times daily for 4–21 days, in alternate weeks | Conjunctival inflammationOcular painPunctate epithelial keratopathy | 572 | |
| Finger et al6 | Conjunctival melanoma and PAM with atypia | 10 | 0.04% MMC qid for 28 days (4) and 7 days (6) | KeratoconjunctivitisCorneal haze | 101 | |
| Demirci et al7 | Conjunctival malignant melanoma and PAM with atypia | 12 | 0.04% four times daily for 28 days (7) | Keratoconjunctivitis | 12 | |
| 0.04% four times daily for 7 days (5) | Focal corneal haze | 1 | ||||
| Daniell et al2 | Corneal conjunctival intraepithelial neoplasia | 20 | 0.02–0.04% MMC four times daily for 1–5 weeks, 1 week on/1 week off | Epithelial toxicityContact dermatitisDisciform keratitis | 1021 | |
| Membranous conjunctivitis | 1 | |||||
| Shields et al10 | Diffuse conjunctival corneal squamous cell carcinoma | 10 | 0.04% MMC four times daily for 1–4 weeks, 1 week on/1 week off | Conjunctival erythemaConjunctival irritationConjunctival chemosis | 632 | |
| Punctate keratopathy | 1 | |||||
| Shields et al8 | Sebaceous gland carcinoma with conjunctival pagetoid spread | 4 | 0.04% MMC four times daily for 1–4 weeks, 1 week on/1 week off | Ocular painConjunctival irritationConjunctival injection | 134 | |
| Recurrent corneal abrasion | 1 | |||||
| Peripheral corneal pannus | 1 | |||||
| Sacu et al12 | Conjunctival malignant melanoma | 1 | 0.04% MMC four times daily for 8 weeks, two 28 days courses, separated by 1 month | Intumescent cataract | 1 | |
| Billing et al13 | Corneal epithelial dysplasia | 1 | 0.04% MMC four times daily for 2 weeks, 1 week on/1 week off | Punctal canalicular stenosis | 1 | |
| Dudney et al11 | Conjunctival corneal intraepithelial neoplasia | 1 | 0.04% MMC four times daily for 5 weeks, five 1 week courses | Recurrent non‐healing corneal epithelial defects/limbal stem cell deficiency | 1 | |
| Kopp et al14 | MM, PAM, SCC | 14 | 0.04% MMC four times daily for 2–18 weeks, one to six 2 week courses | Punctal canalicular stenosis | 6 |
Our study is the largest cohort to date looking at complications of topical MMC. We found that allergic reaction is the most common complication (34%). This has not been previously reported as a common complication. One study suggested possible allergy due to MMC in two of 17 patients (12%) with CIN.1 Three patients from two separate studies were reported as having toxoallergic reactions following MMC treatment.13,14 Interestingly, we found that the incidence of allergic reaction was greatest among patients with conjunctival melanoma (eight of nine cases).
A delayed hypersensitivity reaction could be a possible mechanism for the allergic reaction of the ocular surface to MMC. Firstly, the allergic reaction was always observed after the second or third courses of MMC in our study and never during the first course. Patients who developed an allergy were likely to be sensitised during the first course of treatment. Secondly, the process of sensitisation requires cells to present antigen to T lymphocytes and this role could be fulfilled by Langerhan cells found in the conjunctiva.
Contact allergy to MMC, presenting as exfoliative dermatitis of the palms and soles or generalised itch, has occurred with intravesical instillation or topical application.15,16,17 Patch tests with MMC concentrations as low as 0.01% in these patients was positive, suggesting a type IV hypersensitivity reaction which is cell mediated.15,16,17 Type III hypersensitivity reactions have also been reported with MMC.15 Further studies are needed to evaluate the mechanisms of allergic reaction to MMC on the ocular surface.
Epiphora secondary to punctal stenosis was the next most commonly encountered complication (14%) in our study. Two cases (12.5%) had persistent epiphora, possibly due to more distal obstruction of the nasolacrimal apparatus. The incidence may have been lower if we had used punctal occlusion routinely, but then we would have been unnecessarily inserting punctal plugs into over 80% of our patients. Punctal‐canalicular obstruction was first reported with MMC in a patient with corneal epithelial dysplasia 1 month after treatment.13 In another study, punctal‐canalicular obstruction was noted in 43% of patients treated for PAM, MM, and recurrent SCC 1 month after completion of MMC.14 Punctal stenosis was an unexpected complication of MMC given its effectiveness as an adjunct to punctectomy in preventing punctal restenosis.18 However, obstruction of the punctum and canaliculus has been well reported with other chemotherapeutic agents such as systemic fluorouracil, S‐1, and docetaxel, which are secreted into the tears thereby inducing chronic inflammation and subsequent fibrosis.19,20,21 Inflammation from toxallergic reaction was thought to be a possible mechanism underlying MMC related punctual‐canalicular stenosis in one study13; however, our study showed that there was no significant correlation between allergic reaction and punctal stenosis complications to support this hypothesis. Further studies are necessary to evaluate the mechanism underlying punctal stenosis.
Patients with underlying mild punctal stenosis should be warned of the potential onset or exacerbation of epiphora if MMC treatment is planned. Fortunately, the management of punctal stenosis was mostly straightforward and uncomplicated. In 44% of cases epiphora resolved following simple dilatation of the punctum with syringing of the nasolacrimal system; 33% required a punctal snip to the posterior lip of the lower lid punctum. Long term follow up is necessary to determine if punctal stenosis or restenosis may occur later.
In one of our cases of diffuse CIN involving 360° of limbus and near total corneal involvement, the whole corneal epithelium sloughed off after first course of MMC as a result of complete destruction and shedding of the lesion. A second course of MMC was subsequently given following epithelial healing without development of an epithelial defect. Peripheral pannus and recurrent corneal epithelial abrasion have been reported following MMC treatment for sebaceous carcinoma and diffuse CIN.8,11 It is possible that the limbal stem cell damage in these cases was related to the diffuse neoplastic disease process or its previous surgical treatment rather than to the MMC itself.
Serious complications of MMC have been reported but were seen in the context of pterygium surgery where MMC was applied to the bare sclera for 3–5 minutes via a soaked sponge. Complications have included scleromalacia and perforation, corneal melt, cataract, intractable glaucoma, anterior uveitis, pyogenic granulomas, calcific scleral plaques, and corneal ulcers.22,23 None of these serious complications were observed in our study or in the series that have employed one to five cycles of the four times a day for 7 day regimen of topical MMC for ocular surface neoplasia.1,2,4,8,10 In two exenteration specimens of conjunctival melanoma previously treated with MMC 0.04% four times a day for 7 days and 28 days respectively, no toxic effect was noted on histology of the episclera, cornea, iris, ciliary body, lens, sclera, or retina.7 This finding suggested that the usual regimen of MMC for ocular surface neoplasia does not penetrate deeper than the corneal or conjunctival subepithelium. We therefore believe that allowing time for the corneal epithelium to heal before commencing topical MMC would be important although this was not evaluated in our study.
In the largest study looking at complications of MMC in the treatment of ocular surface neoplasia, allergic reaction and puntal stenosis were the main complications noted. Serious complications were not observed, suggesting the safe use of MMC in mid‐term evaluation. Long term study is needed to determine if limbal stem cell failure will prove to be a complication.
Acknowledgements
We would like to acknowledge the assistance of Ms Emmaé Ramsay, Department of Public Health, University of Adelaide in statistical analysis of the results.
Abbreviations
CIN - corneal‐conjunctival intraepithelial neoplasia
MM - malignant melanoma
MMC - mitomycin C
PAM - primary acquired melanosis
SCC - squamous cell carcinoma
Footnotes
Sponsors: none.
Competing interests: none.
Ethical approval: not required
References
- 1.Frucht‐Pery J, Sugar J, Baum J.et al Mitomycin C treatment for conjunctival‐corneal intraepithelial neoplasia. A multicenter experience. Ophthalmology 19971042085–2093. [DOI] [PubMed] [Google Scholar]
- 2.Daniell M, Maini R, Tole D. Use of mitomycin C in the treatment of corneal conjunctival intraepithelial neoplaisa. Clin Experiment Ophthalmol 20023094–98. [DOI] [PubMed] [Google Scholar]
- 3.Heigle T J, Stulting R D, Palay D A. Treatment of recurrent conjunctival epithelial neoplasia with topical mitomycin C. Am J Ophthalmol 1997124397–399. [DOI] [PubMed] [Google Scholar]
- 4.Wilson M W, Hungerford J L, George S M.et al Topical mitomycin C for the treatment of conjunctival and corneal epithelial dysplasia and neoplasia. Am J Ophthalmol 1997124303–311. [DOI] [PubMed] [Google Scholar]
- 5.Frucht‐Pery J, Pe'er J. Use of mitomycin C in the treatment of conjunctival primary acquired melanosis with atypia. Arch Ophthalmol 19961131261–1264. [DOI] [PubMed] [Google Scholar]
- 6.Finger P T, Grazyna C, Liarikos S. Topical mitomycin C chemotherapy for conjunctival melanoma and PAM with atypia. Br J Ophthalmol 199882476–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Demirci H, McCormick S, Finger P. Topical mitomycin chemotherapy for conjunctival malignant melanoma and primary acquired melanosis with atypia: clinical experience with histopathologic observations. Arch Ophthalmol 2000118885–891. [PubMed] [Google Scholar]
- 8.Shields C L, Naseripour M, Shields J A. Topical mitomycin‐C for pagetoid invasion of the conjunctiva by eyelid sebaceous gland carcinoma. Ophthalmology 20021092129–2133. [DOI] [PubMed] [Google Scholar]
- 9.Frucht‐Pery J, Rozenman Y. Mitomycin C therapy for corneal intraepithelial neoplasia. Am J Ophthalmol 1994117164–168. [DOI] [PubMed] [Google Scholar]
- 10.Shields C L, Naseripour M, Shields J A. Topical mitomycin C for extensive, recurrent conjunctival‐corneal squamous cell carcinoma. Am J Ophthalmol 2002133601–606. [DOI] [PubMed] [Google Scholar]
- 11.Dudney B W, Malecha M A. Limbal stem cell deficiency following topical mitomycin C treatment of conjunctival‐corneal intraepithelial neoplasia. Am J Ophthalmol 2004137950–951. [DOI] [PubMed] [Google Scholar]
- 12.Sacu S, Ségur‐Eltz N, Horvat R.et al Intumescent cataract after topical mitomycin C for conjunctival malignant melanoma. Am J Ophthalmol 2003136375–377. [DOI] [PubMed] [Google Scholar]
- 13.Billing K, Karagiannis A, Selva D. Punctal‐canalicular stenosis associated with mitomycin‐C for corneal epithelial dysplasia. Am J Ophthalmol 2003136746–747. [DOI] [PubMed] [Google Scholar]
- 14.Kopp E D, Seregard S. Epiphora as a side effect of topical mitomycin C. Br J Ophthalmol 2004881422–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kunkeler L, Nieboer C, Bruynzeel D P. Type III and type IV hypersensitivity reactions due to mitomycin C. Contact Dermatitis 20004274–76. [DOI] [PubMed] [Google Scholar]
- 16.Colver G B, Inglis J A, McVittie E.et al Dermatitis due to intravesical mitomycin C: a delayed‐type hypersensitivity reaction? Br J Dermatol 1990122217–224. [DOI] [PubMed] [Google Scholar]
- 17.Torrijos E G, Borja J, Galindo P A.et al Allergic contact dermatitis from mitomycin C. Allergy 199752687. [DOI] [PubMed] [Google Scholar]
- 18.Ma'luf R N, Hamush N G, Awwad S T.et al Mitomycin C as adjunct therapy in correcting punctal stenosis. Ophthal Plast Reconstr Surg 200218285–288. [DOI] [PubMed] [Google Scholar]
- 19.Esmaeli B, Valero V, Ahmadi M A.et al Canalicular stenosis secondary to docetaxel (taxotere): a newly recognized side effect. Ophthalmology 2001108994–995. [DOI] [PubMed] [Google Scholar]
- 20.Eiseman A S, Flanagan J C, Brooks A B.et al Ocular surface, ocular adnexal, and lacrimal complications associated with the use of systemic 5‐fluorouracil. Ophthal Plast Reconstr Surg 200319216–224. [DOI] [PubMed] [Google Scholar]
- 21.Esmaeli B, Golio D, Lubecki L.et al Canalicular and nasolacrimal duct blockage: an ocular side effect associated with the antineoplastic drug S‐1. Am J Ophthalmol 2005140325–327. [DOI] [PubMed] [Google Scholar]
- 22.Dougherty P J, Hardten D R, Lindstrom R L. Corneoscleral melt after pterygium surgery using a single intraoperative application of mitomycin‐C. Cornea 199615537–540. [PubMed] [Google Scholar]
- 23.Rubinfeld R S, Pfister R R, Stein R M.et al Serious complications of topical mitomycin‐C after pterygium surgery. Ophthalmology 1992991647–1654. [DOI] [PubMed] [Google Scholar]