Abstract
Aim
To compare paediatric axial length values estimated from the aphakic refraction alone with axial length values measured by ultrasound.
Methods
Retrospective institutional medical record review of paediatric aphakic patients 12 years of age and younger with documented ultrasonic axial length and objective refraction (retinoscopy) within 3 months of each other. An estimate of axial length was made from the aphakic refraction alone (with an assumed average keratometry value of 44 dioptres) for all patients.
Results
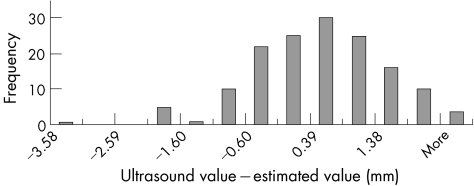
149 eyes of 102 paediatric aphakic patients were identified. The ultrasonic axial length values (mean 22.47 mm, SD 1.69, 95% confidence interval (CI) 0.27) and estimated axial length values (mean 22.41 mm, SD 1.53, 95% CI 0.25) had an average difference of 0.05 mm (SD 1.04, 95% CI 0.17) and were not significantly different (p = 0.56) by the two tailed paired t test. A histogram of the differences that did exist between the two values resembled a normal distribution. The nine eyes with the largest differences between the two values had either low hyperopic aphakic refractions or abnormal average keratometry values.
Conclusions
There was no significant difference between the two groups of axial length values, and the distribution of differences that did exist seemed random. The greatest differences between the two values occurred in longer (less hyperopic) eyes and in eyes with abnormally steep or flat keratometry. Estimation of axial length from the aphakic refraction alone seems to be a useful technique in the average paediatric eye, especially if biometry is unavailable.
Keywords: aphakic refraction, biometry, paediatric axial length
Axial length, the single most important factor in intraocular lens implant (IOL) power calculation, is more difficult to measure in children than in adults for many reasons.1,2 In paediatric phakic eyes IOL prediction error can be several dioptres; much of this error is probably the result of inaccurate axial length measurement by ultrasound biometry.1,2 In aphakic eyes, an alternative method for axial length determination is possible—calculation from the aphakic refraction.3,4,5,6,7,8 This refractive method has been shown to rival biometry in adults when actual keratometry is used.3,4,5 There is little information regarding this technique when an assumed keratometry is used rather than actual keratometry or in children.8 The purpose of this study was to compare paediatric axial length values estimated from the aphakic refraction alone (using a standard keratometry value) with those measured by ultrasonic biometry.
Methods
Institutional review board approval was obtained for the study. Charts of aphakic children 12 years of age and younger with recorded aphakic retinoscopy and aphakic ultrasonic axial length measurements within 3 months of each other were reviewed. Data collected for each eye included aphakic refraction, biometric axial length, and patient age at the time of refraction and biometry. Experienced ultrasound technicians performed contact (not immersion) axial length measurements using the machine's aphakic setting; these measurements were made under anaesthesia for young children and those with poor fixation. The Nidek ultrasound 3300 or Coopervision Ultrascan 404 was used for axial length measurement.
Retinoscopies were performed by experienced paediatric ophthalmologists; chloral hydrate sedation was used on young uncooperative children if necessary. For the study, each eye's axial length was estimated from its aphakic refraction (spherical equivalent) using the following sequence of previously described7 variables and formulas:
R (aphakic refraction) = spherical equivalent value from patient chart;
K (average keratometry) = 44 dioptres (arbitrarily assumed);
VTX (vertex distance) = 0.010 metres (arbitrarily assumed);
nc (corneal index of refraction) = 1.376;
na (aqueous index of refraction) = 1.336;
TC (thickness of the cornea in metres9) = 0.0006;
RcA (anterior corneal radius in metres) = 0.3375/K;
RcP (posterior corneal radius in metres) = RcA − 0.0009;
PFAC (dioptres in front of anterior cornea) = 1/((1/R) − VTX);
PBAC (dioptres behind anterior cornea) = PFAC + ((nc − 1)/RcA);
PFPC (dioptres in front of posterior cornea) = nc/((nc/PBAC)−TC);
PBPC (dioptres behind posterior cornea) = PFPC+((na − nc)/RcP);
AL (axial length in millimetres (mm)) = (na/PBPC) + TC.
Microsoft Excel 2003 was used for the above calculations as well for statistical analysis of the data (the two tailed paired t test at an α of 0.05, the Pearson correlation coefficient, averages, differences, 95% confidence intervals (CIs), data plotting, and histogram generation).
Results
In all, 149 eyes of 102 patients were identified. The mean patient age was 6.99 years (range 6 months to 12 years, SD 3.02). The mean aphakic refraction was 14.06 dioptres (D) (range 8–25D, SD 3.06).
The data for the two axial length values are summarised in table 1 and figure 1. The Pearson correlation coefficient for the two axial length values was 0.80. The two tailed paired t test showed no significant difference between the two axial length values at a 0.05 significance level (t = −0.59 while the critical two tailed value for an α of 0.05 was 1.98). A histogram of the differences that did exist between the two values for each eye resembled a normal distribution (fig 2). The average difference was 0.05 mm with a 95% CI of 0.17. The maximum difference was 3.6 mm, the minimum difference was 0 mm, and the standard deviation of the differences was 1.04.
Table 1 Data for the two axial length values are summarised.
| Ultrasonic value | Estimated value | |
|---|---|---|
| Mean value | 22.47 mm | 22.41 mm |
| 95% CI | 0.27 | 0.25 |
| Maximum value | 26.08 mm | 25.67 mm |
| Minimum value | 17.80 mm | 17.40 mm |
| SD | 1.69 | 1.53 |
Figure 1 A plot of refractive axial length versus ultrasonic axial length shows positive correlation (Pearson coefficient = 0.80).
Figure 2 A histogram of differences between the two values resembles a normal distribution. “More” represents the value +2.38, the maximum positive difference in the study.
A difference between the estimated and measured axial length values of 2 mm or more was found in nine eyes. The aphakic refractions for these nine eyes were: 8.5D, 11.5D, 11.5D, 9.75D, 10.25D, 12.5D, 18D, 18D, 18.75D. For each of these eyes the actual average keratometry ranged from 42–44D except for the final three eyes (the highest aphakic refractions of the group); for these three eyes average keratometry readings were 48.25D, 49D, and 37.5D, respectively.
Discussion
As a group, there was no significant difference between biometric axial length measurements and axial length values estimated from the aphakic refraction in this series of 149 paediatric aphakic eyes. A histogram of the differences that did exist between the two values resembles a normal distribution (fig 2). This finding suggests random rather than regular variation between the two values; previous studies in adults (that used actual rather than assumed keratometry) indicated the same finding.4,6 Six of the nine eyes with the largest differences between the two values were among the least hyperopic (longest) eyes in the study. It is beyond the scope of this study to assess whether refractive estimation or ultrasound measurement was more accurate for these eyes. The other three of these nine eyes were the three eyes with the most extreme actual keratometry values in the study. Although for most patients axial length values estimated from the aphakic refraction were not greatly influenced by the assumption of a standard 44 dioptre average keratometry, this assumption did introduce error when actual keratometry was very flat or very steep.7,8 Use of actual keratometry values would have been expected to increase accuracy; however, the goal of this study was to evaluate axial length estimation from the aphakic refraction alone (and thus with a standard keratometry value).
Both axial length techniques are prone to error in paediatric aphakic eyes. Outpatient ultrasonic axial length measurements in children are limited by inconsistent cooperation and fixation. Under anaesthesia such measurements are prone to error because they are made without having the guidance of a fixating patient. This problem is especially difficult in paediatric aphakic patients, as the lack of a lens spike makes verification of the visual axis even more difficult. (The use of immersion ultrasound techniques would have increased the accuracy of ultrasound measurements, but this was not the standard of care at the hospital during the time of the study.) Further complicating ultrasonic axial length measurement in paediatric eyes are biomechanics that differ from adults—for example, increased corneal elasticity (and thus increased potential for corneal compression), potentially thicker central corneas9 (and thus longer intracorneal ultrasound transit time that what is assumed by the ultrasound unit), and differing ocular tissue viscosity (potentially resulting in an actual speed of sound different than what is assumed by the ultrasound unit).1,2 The aphakic refraction technique for axial length estimation used in this study also had several potential sources of error. Younger children with more rapidly growing eyes may have had a difference in axial length from the time the retinoscopy was done to the time the ultrasound was done. The refractions obtained were the best objective estimate of the examiner, who was using the retinoscope on the child for an approximate refraction (not for precise axial length determination) that would then typically be overplussed a few dioptres for the actual worn refractive correction (and therefore the examiner did not need to be extremely accurate). For younger uncooperative children retinoscopy was performed under sedation; without patient fixation there is a question as to whether or not the objective refraction is along the visual axis. Vertex distances were not recorded; therefore, a standard vertex distance of 10 mm was assumed. Use of this arbitrary vertex distance may be the reason we found ultrasonic values to be larger on average than values estimated from the aphakic refraction (the opposite would have been expected because ultrasound measures axial length to the vitreoretinal interface rather than to retinal/choroidal pigment).3,4,5,6,7 This difference, however, was not statistically significant and both means have overlapping 95% confidence intervals. In addition, as discussed above, the assumption of a standard keratometry value when estimating axial length from the aphakic refraction as was done in this study introduces significant error when actual keratometry is very flat or very steep.7,8
In summary, paediatric axial lengths can be estimated from aphakic refractions alone, and these estimates are not significantly different from axial length values as measured by ultrasound. The largest observed differences between the estimated and measured values were in longer (less hyperopic) eyes and eyes with very steep or flat corneas. One would expect improved results for the latter eyes if actual keratometry were used. For the average paediatric aphakic eye, the refractive method can be a useful technique for axial length estimation, especially if biometry is unavailable. This study does not address which value is more suitable for intraocular lens implant power prediction, a topic that deserves further study.
Footnotes
This study was approved by the Human Ethics Committee and Institutional Review Board of the King Khaled Eye Specialist Hospital in Riyadh, Saudi Arabia.
References
- 1.Mezer E, Rootman D S, Abdolell M.et al Early postoperative refractive outcomes of pediatric intraocular lens implantation. J Cataract Refract Surg 200430603–610. [DOI] [PubMed] [Google Scholar]
- 2.Andreo L K, Wilson M E, Sauders R A. Predictive value of regression and theoretical IOL formulas in pediatric intraocular lens implantation. J Pediatr Ophthalmol Strabismus 199734240–243. [DOI] [PubMed] [Google Scholar]
- 3.Weinstein G W, Baum G, Binkhorst R D.et al A comparison of ultrasonographic and optical methods for determining the axial length of the aphakic eye. Am J Ophthalmol 1966621194–1201. [DOI] [PubMed] [Google Scholar]
- 4.Binkhorst R D. The accuracy of ultrasonic measurement of the axial length of the eye. Ophthalmic Surg 198112363–365. [PubMed] [Google Scholar]
- 5.Olsen T. Calculating axial length in the aphakic and the pseudophakic eye. J Cataract Refract Surg 198814413–416. [DOI] [PubMed] [Google Scholar]
- 6.Krag S, Olsen T. Secondary IOL power calculation: a comparison of an optical and a biometric method. Acta Ophthalmol 199169625–629. [PubMed] [Google Scholar]
- 7.McClatchey S K, Parks M M. Theoretic refractive changes after lens implantation in childhood. Ophthalmology 19971041744–1751. [DOI] [PubMed] [Google Scholar]
- 8.Hug T. Use of the aphakic refraction in intraocular lens (IOL) power calculations for secondary IOLs in pediatric patients. J Pediatr Ophthalmol Strabismus 200441209–211. [DOI] [PubMed] [Google Scholar]
- 9.Simon J W, O'Malley M R, Gandham S B.et al Central corneal thickness and glaucoma in aphakic and pseudophakic children. J AAPOS 20059326–329. [DOI] [PubMed] [Google Scholar]