Abstract
Aim
To document the long term outcome of congenital cataract surgery with primary posterior chamber (PC) lens implantation in the first year of life.
Method
A retrospective review of congenital cataract surgery in the first year of life with PC lens implantation in 18 infants, eight with unilateral and 10 with bilateral cataract. The average age at surgery was 15 weeks (range 3–44 weeks). The mean follow up was 95 months (range 60–139 months).
Results
The best outcomes were in the bilateral group where 50% of eyes achieved 6/18 or better, with a best acuity of 6/9. Acuities were poor in the unilateral group where only 38% achieved 6/60 or better, with a best acuity of 6/24. There was a mean refractive shift between first refraction after surgery and refraction at 36 months after surgery of −3.44 dioptres with a very wide range (+2.00 to −15.50). There was a significantly greater myopic shift in the unilateral cases. Many eyes in both groups continued to show an increasing myopic shift between 36 months after surgery and their final recorded refraction. The main complications were amblyopia, especially in unilateral cataracts, and posterior capsular opacification. Amblyopia was most probably related to a combination of early onset of dense cataract in this young age group, late presentation for initial surgery, delay in capsulotomies, and imperfect compliance with a rigorous occlusion regime.
Conclusion
Intraocular lens implantation in infants less than 1 year of age is generally a safe procedure. The spread of final refractive error was very wide. Final refraction in the unilateral group was significantly more myopic than the bilateral group. Final acuities were often disappointing especially in the unilateral group.
Keywords: cataract surgery, paediatrics, lens implant, congenital
The safety of intraocular lens (IOL) implantation in children is now well established1,2,3,4 although the long term effects of these implants remain undetermined. Posterior chamber (PC) lens implantation in children less than 1 year of age is a controversial issue but initial results are encouraging.5
Methods
The records of all children who had surgery for congenital cataract under the age of 12 months with a lens implant, at Bristol Eye Hospital between 1990 and 1998, were included. Eyes which had other structural abnormalities such as persistent hyperplastic primary vitreous or microphthalmos were excluded as lenses were not implanted in these situations. Eight children had unilateral and 10 had bilateral cataract surgery.
Biometry was performed at surgery using a hand held Nidek KM‐500 autokeratometer (Nidek Inc, Fremont, CA, USA) and axial length measurements were made using an Allergan Humphrey Ultrasonic Biometer 820 (Allergan Humphrey, San Leandro, CA, USA). Lens power calculations used the SRK II formula but as the indicated power was often considerably above +30 dioptres, an empirical reduction of approximately 20% was applied to the lens implanted. No lens above +30 dioptres was implanted and no power reduction was made if biometry indicated a lens of less than +26 dioptres. During the period studied, six types of lens implants were used (table 1).
Table 1 Lens implant characteristics.
| Lens type | “A” constant | Patient number |
|---|---|---|
| Alcon Acrysof MA30BA | 118.9 | 1, 1, 2, 9, 9, 14, 15, 16, 16, 18, 18 |
| Pharmacia 809C | 118.0 | 3, 5, 5, 13, 13 |
| Iolab SU124 | 118.0 | 4, 4, 11, 17 |
| Alcon Iogel | 118.5 | 7, 8, 12, 12 |
| Iolab L141U | 118.0 | 10, 10 |
| Surgidev 5BUV | 118.0 | 6 |
In bilateral cataracts, the same type of implant was used for each eye.
Cataracts were aspirated via two corneal incisions which were sutured at the end of surgery. The anterior capsulorrhexis was formed using a vitreous cutter or radio frequency diathermy (Oertli, Berneck, Switzerland).
Posterior capsulotomies were always carried out as a separate and subsequent procedure via the pars plana using a vitreous cutter.
Clinical characteristics of the infant groups are listed in tables 2–4. Where a reasonably reliable refraction could not be obtained at the specified interval after surgery, no refraction was recorded in the tables.
Table 2 Unilateral congenital cataracts.
| Patient no | Sex | R/L | Age at op (weeks) | IOL power (D) | Axial length (mm) | Refraction | Final visit (months postop) | Final postop acuity | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First refraction | At 1 year | At 2 years | At 3 years | Final refraction | ||||||||
| 2 | M | L | 3 | 26.0 | 19.00 | −5.00 | −7.50 | −7.25 | −7.50 | −3.75 | 82 | 6/60 |
| 3 | F | L | 4 | 26.0 | 17.00 | 6.00 | 3.50 | 1.00 | 1.00 | 0.75 | 112 | 6/24 |
| 6 | F | R | 12 | 27.0 | 17.64 | 2.50 | −0.50 | −0.25 | −8.00 | 132 | 1/60 | |
| 7 | M | L | 12 | 24.0 | 18.07 | 3.00 | 2.00 | −9.50 | −12.50 | −12.50 | 139 | 1/60 |
| 11 | F | L | 18 | 28.0 | 18.20 | 2.50 | 4.00 | 0.75 | −0.25 | −3.50 | 78 | 6/60 |
| 14 | F | L | 40 | 26.0 | 18.66 | 5.25 | 1.00 | 1.00 | 0.75 | 1.00 | 61 | 0.5/60 |
| 15 | F | R | 44 | 26.0 | 16.58 | 9.00 | 3.50 | 5.50 | 3.75 | 1.00 | 61 | 1/60 |
| 17 | F | R | 7 | 30.0 | 16.30 | 8.50 | 1.50 | 2.50 | 0.50 | 92 | 1/60 | |
Refractions are mean spherical equivalents. IOL power corrected for an “A” constant of 118.0.
Table 3 Clinical characteristics in bilateral congenital cataracts.
| Patient no | Sex | R/L | Age at op (weeks) | IOL power (D) | Axial length (mm) | Refraction | Final visit (months postop) | Final postop acuity | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First refraction | At 1 year | At 2 years | At 3 years | Final refraction | ||||||||
| 1 | M | R | 3 | 26.0 | 15.33 | 11.00 | 7.25 | 7.50 | 7.50 | 5.75 | 75 | 6/18 |
| 1 | M | L | 4 | 26.0 | 15.27 | 12.25 | 9.75 | 8.50 | 8.00 | 5.75 | 6/9 | |
| 4 | M | L | 8 | 28.0 | 17.50 | 5.75 | 6.00 | 4.50 | 3.50 | 0.75 | 75 | 6/18 |
| 4 | M | R | 10 | 28.0 | 18.00 | 4.50 | 5.50 | 4.25 | 1.75 | −2.50 | 2/60 | |
| 5 | M | L | 7 | 27.0 | 18.50 | 6.25 | 5.25 | 3.00 | 3.25 | 1.50 | 95 | 6/24 |
| 5 | M | R | 8 | 27.0 | 17.50 | 4.00 | 3.75 | 2.75 | 2.75 | 0.25 | 6/12 | |
| 9 | M | R | 9 | 27.0 | 15.84 | 10.50 | 10.00 | 8.75 | 7.75 | 6.00 | 82 | 6/36 |
| 9 | M | L | 23 | 26.0 | 15.97 | 12.00 | 11.50 | 10.25 | 10.50 | 9.25 | 6/24 | |
| 10 | M | L | 12 | 21.5 | 15.00 | 8.50 | 8.50 | 7.25 | 8.50 | 9.50 | 122 | 6/60 |
| 10 | M | R | 14 | 22.0 | 16.00 | 12.00 | 8.00 | 8.00 | 7.25 | 3.25 | 6/36 | |
| 12 | M | R | 27 | 23.0 | 21.02 | 7.00 | 8.00 | 6.75 | 4.75 | 2.00 | 125 | 6/18 |
| 12 | M | L | 28 | 23.0 | 20.90 | 7.00 | 8.50 | 4.25 | 3.00 | 2.50 | 6/36 | |
| 13 | M | R | 32 | 27.0 | 21.11 | −0.25 | −1.75 | −3.00 | −3.25 | −4.25 | 75 | 6/12 |
| 13 | M | L | 34 | 27.0 | 21.05 | 0.25 | −2.50 | −2.75 | −4.25 | −6.00 | 6/12 | |
| 18 | M | R | 3 | 26.0 | 17.00 | 5.50 | 2.75 | 2.50 | 2.50 | 2.75 | 60 | 6/12 |
| 18 | M | L | 4 | 26.0 | 17.00 | 7.00 | 5.00 | 4.50 | 5.50 | 4.50 | 6/60 | |
First operated eye listed first. Refractions are mean spherical equivalents. IOL power corrected for an “A” constant of 118.0.
Table 4 Bilateral congenital cataract, but IOL or vision in one eye only.
| Patient no | Sex | R/L | Age at op (weeks) | IOL power (D) | Axial length (mm) | Refraction | Final visit (months postop) | Final postop acuity | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First refraction | At 1 year | At 2 years | At 3 years | Final refraction | ||||||||
| 8 | F | L | 12 | 24.0 | 15.97 | 0.50 | −2.00 | −3.00 | −11.00 | 166 | 6/36 | |
| 8 | F | R | 13 | 16.47 | 13.00 | 13.50 | 8.75 | 6/60 | ||||
| 16 | M | R | 4 | 26.0 | 15.75 | 7.00 | 4.50 | 9.00 | 9.00 | 10.75 | 67 | 6/24 |
| 16 | M | L | 6 | 26.0 | 15.75 | PL | ||||||
Refractions are mean spherical equivalents. IOL power corrected for an “A” constant of 118.0.
Patient 8 had bilateral cataract but an implant in the left eye only. Patient 16 developed an early left endophthalmitis and no subsequent vision recordable from this eye.
Visual acuity was measured by a variety of methods appropriate for age—Teller Acuity Cards (Vistech Consultants Inc, Dayton, OH, USA), Cardiff Cards (Keeler, Windsor, UK), Kay pictures (Clement Clarke International Ltd, Harlow, UK), Sheridan Gardner single letters and, finally, linear Snellen letters.
Results
The mean age at surgery was 17.5 weeks (range 3–44 weeks) in the unilateral group, and 13.0 weeks (range 3–34 weeks) in the bilateral group. The mean follow up of 95 months (range 60–139 months) was similar in both groups (tables 2–4).
Acuities
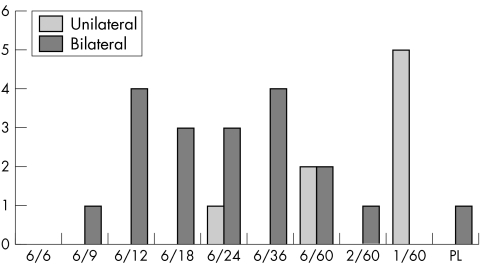
In the bilateral group, 50% achieved 6/18 or better; the best was 6/9. In the unilateral group, only 38% achieved 6/60 or better; the best was 6/24 (fig 1).
Figure 1 Final visual outcome (number of cases achieving each acuity level).
Refraction
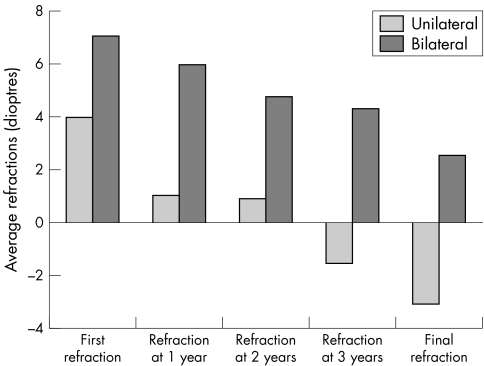
There was a mean refractive shift between first refraction after surgery and refraction at 36 months after surgery of −5.53 dioptres (range −2.50 to −15.50) for unilateral cases, and −2.77 dioptres (range 0.0 to −4.75) for bilateral cases. This difference was significant (p<0.023, independent samples t test). Many eyes continued a significant myopic shift between 36 months and the date of their final recorded refraction (fig 2).
Figure 2 Change in averaged refraction over time in unilateral and bilateral cases.
Spherical equivalent refraction at 36 months averaged −1.56 dioptres for unilateral cases (range +3.75 to −12.50), and +4.31 dioptres for bilateral cases (range +10.50 to −4.25). The difference was highly significant (p<0.007, independent samples t test).
Complications
Apart from amblyopia, posterior capsule opacification (table 5) was the most common complication in our series. Other complications are listed in table 6.
Table 5 Posterior capsulotomy.
| Number and type of capsulotomy | Patient number |
|---|---|
| No capsulotomy required | 16R |
| Laser | 6, 13R, 13L |
| Surgical | All other eyes |
| Second capsulotomy | 1R, 6, 8L, 12L, 13L |
| Third capsulotomy | 1R, 8L |
Second and third capsulotomies were always surgical.
R or L after a patient number indicates the eye affected in bilateral cases.
Table 6 Complications.
| Type of complication | Patient number |
|---|---|
| Endophthalmitis | 16L |
| Iris prolapse | 11, 16L |
| Iris to wound | 6, 8L, 18R, 18L |
| Fibrocellular membrane over anterior IOL surface | 1R, 1L, 2, 3 |
| Iris capture by IOL | 4R |
| Raised IOP/glaucoma | 4R, 4L |
Patient number repeated where both eyes affected.
R or L after a patient number indicates the eye affected in bilateral cases.
Discussion
Clearly a study such as this has limitations because of possible bias in selection, and because accurate refraction in infants after lens aspiration and lens implantation is often very challenging even for experienced optometrists, probably explaining the irregular changes in refraction sometimes recorded in our subjects (tables 2–4).
Complications
Capsulotomy was carried out as a secondary procedure, as it was thought that not all capsules would thicken or opacify and that we would be able to detect and treat posterior capsular opacification at a stage before it had much effect on vision. In practice, we found that only one eye did not require a capsulotomy. When we did perform capsulotomies, we were often surprised at the denseness of opacification despite being able to view the fundus and perform refraction. Failure to detect opacification at an early stage probably contributed to the denseness of amblyopia. In general we found that laser capsulotomy was not very effective at this age (and even up to the age of 5 years) requiring surgical revision in almost all cases.
Although our impression was that the incidence of glaucoma was less than in non‐implanted eyes, possible selection bias prevents us drawing safe conclusions about this, and even longer follow up may be required to detect late development of glaucoma.
Amblyopia
Our visual outcomes, although disappointing, compare reasonably well to outcomes in aphakic correction in this very young age group.6,7 Poor visual results may have related to delays in presentation for surgery, insufficiently early clearance of posterior capsule opacification, and imperfect adherence to the necessary rigorous occlusion regimes.8
Refraction
Implanting an IOL of fixed power in a growing eye is acknowledged as a problem.9,10,11,12 Employing the algorithm for lens power stated in the Methods section still resulted in a wide range of residual refractive error.
Whereas there was no significant difference in either initial axial length or first refraction after surgery between the unilateral and bilateral groups, at 36 months postoperatively and at final refraction, spherical equivalent refractive error was significantly more myopic or less hypermetropic in the unilateral group than the bilateral group. We expected to be able to show that this was related to denser amblyopia in the unilateral group but were unable to show, in individual cases, a link between final refractive error and final acuity. As a group, however, the unilateral cataract cases showed a link between poor acuity and more myopic refraction. We could show no significant relations between initial axial length, age at surgery, implanted IOL power, and visual and refractive outcome in this study with its modest number of cases.
The lessons learnt from this early series were the importance of no delay in surgery, simultaneous posterior capsulotomy with anterior vitrectomy, the fashioning of a strong capsulorrhexis using an adaptive viscoelastic such as Healon5 (Advanced Medical Optics, Santa Ana, CA, USA) so that the implant is securely in the bag, accurate suturing of all corneal entry sites using 10/0 Vicryl (Ethicon Ltd, Edinburgh, UK), and a rigorous postoperative occlusion regime.
Abbreviations
IOL - intraocular lens
PC - posterior chamber
Footnotes
Competing interests: none.
Approval for this study was obtained from the Central and South Bristol Research Ethics Committee, UBHT Headquarters, Marlborough Street, Bristol BS1 3NU, UK.
References
- 1.Markham R H C, Bloom P A, Chandna A.et al Results of intraocular lens implantation in paediatric aphakia. Eye 19926493–498. [DOI] [PubMed] [Google Scholar]
- 2.O'Keefe M, Mulvill A, Yeoh P L. Visual outcome and complications of bilateral intraocular lens implantation in children. J Cataract Refract Surg 2000261758–1764. [DOI] [PubMed] [Google Scholar]
- 3.Cassidy L, Rahi J, Nischal K.et al Outcome of lens aspiration and intraocular lens implantation in children aged 5 years and under. Br J Ophthalmol 200185540–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zwaan J, Mullaney P B, Awad A.et al Pediatric intraocular lens implantation; surgical results and complications in more than 300 patients. Ophthalmology 1998105112–119. [DOI] [PubMed] [Google Scholar]
- 5.O'Keefe M, Fenton S, Lanigan B. Visual outcomes and complications of posterior chamber intraocular lens implantation in the first year of life. J Cataract Refract Surg 2001272006–2011. [DOI] [PubMed] [Google Scholar]
- 6.Lundvall A, Kugelberg U. Outcome after treatment of congenital bilateral cataract. Acta Ophthalmol Scand 200280593–597. [DOI] [PubMed] [Google Scholar]
- 7.Lundvall A, Kugelberg U. Outcome after treatment of congenital unilateral cataract. Acta Ophthalmol Scand 200280588–592. [DOI] [PubMed] [Google Scholar]
- 8.Wilson M E, Jr, Trivedi R H, Hoxie J P.et al Treatment outcomes of congenital monocular cataracts: the effects of surgical timing and patching compliance. J Pediatr Ophthalmol Strabismus 200340323–329. [DOI] [PubMed] [Google Scholar]
- 9.Wilson M E, Jr, Trivedi R H. Eye growth after pediatric cataract surgery. Am J Ophthalmol 20041381039–1040. [DOI] [PubMed] [Google Scholar]
- 10.Vasavada A R, Raj S M, Nihalani B. Rate of axial growth after congenital cataract surgery. Am J Ophthalmol 2004138915–924. [DOI] [PubMed] [Google Scholar]
- 11.Plager D A, Kipfer H, Sprunger D T.et al Refractive change in pediatric pseudophakia: 6‐year follow‐up. J Cataract Refract Surg 200228810–815. [DOI] [PubMed] [Google Scholar]
- 12.McClatchey S K, Dahan E, Maselli E.et al A comparison of the rate of refractive growth in pediatric aphakic and pseudophakic eyes. Ophthalmology 2000107118–122. [DOI] [PubMed] [Google Scholar]