Abstract
A major challenge for the immune system is to recognize and eliminate cells undergoing carcinogenesis. Immune defense against tumors is complex. It can be mediated early by the innate immune system (i.e., phagocytes, NK cells, NKT cells, cytokines, and complement proteins) and later by the adaptive immune system (i.e., B cells and T cells). The eight articles in this Review series on tumor immunology discuss the mechanisms underlying immune surveillance of tumors, the regulation of carcinogenesis by immune inflammatory mediators, current approaches to controlling tumor growth through immunotherapy, and novel targets of immunotherapy.
Resurrection of the immune surveillance theory
The concept that the immune system protects the host against cancer was first posited by Ehrlich in 1909 (1) and modified in the 1950s by Burnet and Thomas (2, 3), who proposed that it was instrumental in eliminating precancerous or cancerous cells, through a “surveillance” function. However, the concept fell out of favor when studies in the 1980s indicated that tumors failed to develop more rapidly in nude mice (which lack T cells and B cells, but not NK cells) than in wild-type mice. It was resurrected in the 1990s, when a body of evidence emerged indicating that immunodeficient mice were at greater risk for spontaneous tumor development (4). These studies led to further refinement of the theory, now referred to as “cancer immunoediting,” encompassing three phases: elimination, equilibrium, and escape.
Elimination.
During the elimination phase, nascent tumor cells are destroyed by elements of the innate and adaptive immune systems (Figure 1). Evidence for the existence of this phase comes from animal experiments examining spontaneous or carcinogen-induced tumors in mice that lack specific immune effector cells, molecules, or pathways that are important for suppressing tumor growth. For example, RAG2-deficient mice, which lack T cells, B cells, and NK cells, spontaneously develop adenomas of the intestine and lung (5). Similarly, mice lacking key cytokines such as IFN-γ (6) have a higher incidence of tumor development with age than wild-type mice. Molecules involved in antigen processing and presentation and mediators of cytotoxic pathways are also critical for controlling tumor growth (7). Although these studies provide very strong support for immune surveillance, Jeremy Swann and Mark Smyth, in the first article of this Review series (8), point out that models in which tumors develop spontaneously and then undergo autochthonous regression, which would provide definitive evidence of immunoediting, have yet to be established.
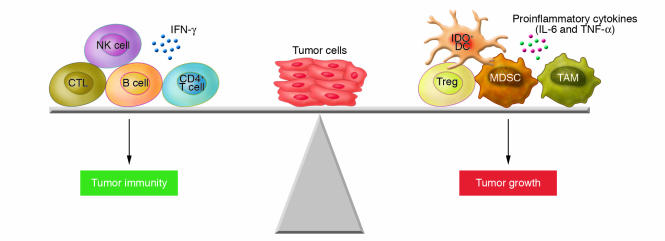
Figure 1. Some of the immunological factors discussed in this Review series that affect tumor development.
Cells of both the innate and adaptive arms of the immune system can mediate antitumor immunity, including CTLs, CD4+ T cells, B cells, and NK cells. However, as tumors progress, they often develop ways in which to escape immune recognition. For example, they can induce the production of proinflammatory cytokines, the expression of IDO by APCs, and the differentiation of Tregs and various suppressor cells of myeloid origin. TAM, tumor-associated macrophage.
In humans the evidence for immunoediting is less substantial but nevertheless suggestive. Immunosuppressed patients have a higher incidence of tumors, especially those of viral etiology (9). Individuals whose tumors are infiltrated with T cells have a more favorable prognosis (10). CTLs and/or antibodies that have antigen reactivity toward antigens expressed by both tumor and neuronal cells have been implicated in paraneoplastic disease. In some cases, patients present with paraneoplastic disease and no clear evidence of a tumor, suggesting that the neuronal outcome might be secondary to a strong antitumor response (11).
Equilibrium.
The second phase of immunoediting is the equilibrium phase, in which tumor cells persist but are “equilibrated” by the immune system. Indirect evidence of this phase comes from studies in which spontaneous or carcinogen-derived tumors have been transplanted into immunodeficient and wild-type mice. Although these tumors are eliminated in wild-type mice, they grow progressively in syngeneic immunodeficient animals (5, 12). These data suggest that tumors normally undergo sculpting by the immune system. More direct evidence of the equilibrium phase comes from experiments showing that if wild-type mice that are tumor free after low-dose methylcholanthrene administration are depleted of CD4+ and CD8+ T cells at day 200, they rapidly develop sarcomas that have unusual growth characteristics when transplanted into naive recipients (13).
Escape.
The final phase of immunoediting is termed escape, in which tumors actively disable immune recognition by co-opting immune cells for growth, angiogenesis, and invasion. Escape constitutes several complex events and processes, including loss of antigen-presenting machinery, tumor antigens, and sensitivity to immune effector molecules; expression of inhibitory molecules that induce T cell apoptosis or anergy; and induction of Tregs (4, 8, 14–17). Three mechanisms of escape are highlighted in this Review series (Figure 1).
First, David Munn and Andrew Mellor review the role of indoleamine 2,3-dioxygenase (IDO), an enzyme that catalyzes the rate-limiting step of tryptophan degradation along the kyneurenine pathway, in tumor-induced tolerance (18). IDO is produced by several cells, including tumor cells and APCs (both conventional and plasmacytoid DCs) (19–21), and its function is dependent on activation signals imparted to the APCs (22). IDO-mediated immune suppression is due to the production of tryptophan metabolites and local reduction of tryptophan levels, which cause T cell apoptosis and suppress T cell proliferation (23–26). The stress-responsive kinase general control nonderepressible 2 (GCN2), activated by amino acid deficiency, was recently shown to participate in IDO-mediated T cell anergy (27). In addition, IDO expression in APCs has been associated with the induction of immunosuppressive Tregs (28, 29). DC subsets expressing IDO have been described in tumor-draining lymph nodes, and IDO expression has been linked to poor clinical outcome (19, 30). As IDO expression can be induced by vaccine adjuvants and microbial infection, it might have a normal physiologic counterregulatory role in response to inflammation. Therefore, vaccines (including cancer vaccines) that induce its production might benefit from simultaneous addition of IDO inhibitors.
Second, tumors can also induce the differentiation of circulating myeloid cells into suppressor cells, termed collectively myeloid-derived suppressor cells (MDSCs) (31), which impact on immune surveillance mechanisms. MDSCs, discussed in this Review series by Antonio Sica and Vincenzo Bronte (32), are a complex mix of CD11b+ and Gr-1+ mononuclear cells that mediate the suppression of T cells in cancer and other pathological conditions. MDSCs apparently require activation by T cells, after which they inhibit CD4+ and CD8+ T cells in an MHC-independent manner (33). They express the inducible forms of NOS2 and arginase (ARG1), enzymes involved in the metabolism of arginine. Recently, Bronte’s group showed that both NOS2 and ARG1 are expressed by MDSCs in an IL-13– and IFN-γ–dependent manner and function synergistically to induce T cell dysfunction or apoptosis through the production of reactive nitrogen and oxygen species (33). MDSCs can also induce the development of Tregs (34). Tumor-associated macrophages (TAMs), another type of myeloid suppressor cell, are recruited to tumors and promote tumor growth by enhancing inflammation and angiogenesis (35, 36). Their role in promoting angiogenesis in tumors was recently confirmed with the identification of a new lineage of monocytes expressing the angiopoietin receptor TIE2 that are required for tumor vessel formation (37). Therapeutic approaches to reverse the effects of MDSCs and TAMs have focused on neutralizing their functional activity (38–41), vaccinating against expressed molecules (42), and inducing their differentiation into mature myeloid cells (43).
Finally, in his Personal Perspective, Tyler Curiel discusses the role of Tregs in impeding tumor immune surveillance (44). CD4+ Tregs typically express CD25 (the α chain of the IL-2 receptor), cytotoxic T lymphocyte–associated antigen 4 (CTLA4), glucocorticoid-induced TNF receptor–related protein (GITR), and the transcription factor forkhead box P3 (FOXP3). They are generated in the thymus and the periphery (45–48) and exert their suppressive activity on multiple immune cells (T cells, NK cells, NKT cells, B cells, and APCs), through both contact-dependent and contact-independent mechanisms. Treg accumulation has been documented in various tumors, in tumor-draining lymph nodes, and in the peripheral circulation of individuals with cancer, and tumor antigen–specific Tregs have also been described (49). An inverse correlation between the number of Tregs in the tumor and clinical outcome has been noted (50), although the opposite observation has been made in hematologic malignancies (51, 52). Nevertheless, efforts to reduce Treg function in patients with cancer are being evaluated (53, 54), as their depletion can enhance the effects of immunotherapy in certain cases (54–56). This is especially important given that cancer vaccines might induce Tregs in addition to activating antitumor responses in vivo (57).
The link between inflammation and cancer
Malignant transformation can be closely associated with chronic infection and inflammation, as highlighted by cancers of the gastrointestinal tract. For example, liver cancer is associated with excessive alcohol consumption and infection with HBV and HCV, colon cancer is associated with inflammatory bowel disease, and gastric cancer can develop in individuals chronically infected with Helicobacter pylori (58). In their Review, Wan-Wan Lin and Michael Karin summarize the complex cytokine networks that seem to link inflammation, innate immunity, and cancer (59).
The inhibitor of NF-κB kinase/NF-κB (IKK/NF-κB) signaling pathway is an important molecular link between inflammation and tumor progression. Activation of the NF-κB family of transcription factors upregulates several genes whose products promote the phenotype and growth of malignant cells (60, 61). IKK/NF-κB signaling is one of many pathways activated following the recognition of pathogen-associated molecular patterns by pattern recognition receptors (PRRs). PRRs include TLRs and nucleotide-binding oligomerization domain–like (NOD-like) receptors. Recognition of pathogens by these receptors normally induces a host immune response that leads to their eradication. When this response fails, chronic inflammation ensues, and this can increase the risk of malignancy. For example, mutations in the NOD2 locus are associated with a higher risk for developing Crohn disease, possibly due to enhanced production of IL-1β (62, 63), and might be predisposing factors to colorectal cancer (64).
Lin and Karin summarize the role of several cytokines, produced by immune cells in response to inflammatory triggers, in tumor development and progression. The prolonged production of TNF-α for example, can induce NF-κB–dependent expression of antiapoptotic and proliferative genes, enhance angiogenesis, and adversely affect immune surveillance by conferring resistance to TNF-related apoptosis-inducing ligand (TRAIL) (65). Cytokines such as IL-6, induced through TLR activation or produced endogenously (e.g., by stromal cells), can promote cell cycle progression and exacerbate the effects of TNF-α. Indeed, IL-6 has been implicated in the development of multiple myeloma (66) and Kaposi sarcoma (67) and an elevated risk of Hodgkin lymphoma (68). Therefore, therapies that neutralize pathways that induce the chronic production of proinflammatory cytokines might limit tumor growth. Indeed, inhibition of NF-κB in cancer cells converts inflammation-induced TNF-α–mediated tumor growth to TRAIL-mediated tumor regression (65). Inhibitors of TNF-α are in wide use for the treatment of rheumatoid arthritis, but it remains to be seen whether they can be used to treat cancers associated with chronic inflammation (69).
Lin and Karin also discuss the role of immunosuppressive and antiinflammatory cytokines and factors in tumor development and growth. It seems that IL-10 and TGF-β can exhibit tumor-suppressing activity under certain circumstances; mice lacking either IL-10 or TGF-β1 are more susceptible to cancer in response to infection with enteric bacteria (70–72). By contrast, these factors can also promote tumor growth and development. Activation of STAT3 in tumor cells endows them with enhanced survival, metastatic, and angiogenic properties and confers suppressive effects on inflammatory and immune responses in the tumor microenvironment through the production of IL-10, IL-6, and VEGF (73). These factors inhibit DC activation, suppress T cell responses; block the proinflammatory effects of macrophages, NK cells, and neutrophils; and facilitate the induction of Tregs (41, 73–75). Moreover, STAT3 activation induces the downregulation of molecules necessary for functional antitumor immune responses (e.g., IL-12, IFN-γ, and IFN-β), which are also produced following NF-κB activation. Therefore, STAT3 can block the ability of NF-κB to stimulate antitumor immunity (76, 77) but cooperate with it to promote oncogenesis (73). Small-molecule inhibitors targeting STAT3 directly or indirectly can block the signaling effects of cytokines such as IL-6 and TGF-β and reverse the abnormal differentiation of DCs in cancer (41, 78).
Cancer vaccines and immunotherapy: a reality?
The most successful example of a vaccine that protects against developing cancer is the HBV vaccine, which protects individuals from hepatitis B and thereby reduces the likelihood of developing liver cancer (79). Likewise, the new vaccines used to prevent infection with HPV have been associated with reduced cervical dysplasia (80). Of course, these illustrate the relatively easy job of inducing protective antiviral immunity compared with inducing immunity to tumor antigens, many of which are self antigens. Can successful vaccines for cancers not associated with infectious agents be developed? Is it possible to develop immunotherapies to effectively eliminate existing tumors? The final three articles in this Review series highlight advances in immunological approaches to treat tumors.
Novel adjuvants.
TLR agonists are an exciting new class of vaccine adjuvants. Oligodeoxynucleotides containing one or more unmethylated CpG dinucleotides (CpG ODN), which target TLR9 and are the subject of the Review by Arthur Krieg (81), are probably the furthest along in clinical testing (82). Their adjuvant activity is based on their ability to activate human B cells and plasmacytoid DCs, the two main cell types that express TLR9 in humans. From several animal models, it is apparent that unmethylated CpG ODN can stimulate antitumor immunity, in some cases quite effectively. In humans, unmethylated CpG ODN enhance the immunogenicity of HBV and influenza vaccines (82) and can amplify the adjuvant effects of incomplete Freund’s adjuvant (IFA) in the tumor setting. Responses of CD8+ T cells from the blood to the HLA-A*0201–restricted melanoma-associated antigen recognized by T cells 1 (MART1) epitope were increased by more than 10-fold when CpG ODN were added to a mixture of the epitope and IFA, compared with the mixture alone (83), although they were qualitatively inferior within tumor sites (84). Incorporation of CpG ODN into vaccine mixtures will require optimization, however, as the responses obtained thus far in humans and nonhuman primates have not yet proven to be protective. Nevertheless, CpG ODN can synergize with other antitumor modalities by enhancing underlying antitumor immune responses after chemotherapy-mediated elimination of Tregs or other suppressive mechanisms. Furthermore, the addition of CpG ODN to chemotherapy (a combination of a taxane and a platinum-based drug) in untreated non–small cell lung cancer improved the response rate but not survival, compared with the chemotherapy alone (85), a result that is now being followed up in a phase III clinical trial. However, there are potential downsides to CpG ODN therapy, as under certain situations, CpG ODN contribute to the induction of Tregs (86), and this will require careful evaluation in humans. Although autoimmunity has not been described thus far, side effects such as thrombocytopenia will also need to be evaluated in larger human studies.
DC-based immunotherapy.
DCs have directly induced immunity in many clinical trials, but only limited success has been achieved in terms of inducing partial or complete remissions in cancer patients (87).
The most striking results were observed in HIV-infected individuals immunized with chemically inactivated, autologous virus–pulsed DCs who achieved viremic control (88). The Review by Eli Gilboa discusses why the promise of this approach has yet to be realized in the tumor setting (89). In many cases DCs used in the treatment of patients with cancer are differentiated in vitro from blood monocytes and activated in vitro by cytokines and PGE2, which render them resistant to in vivo licensing by costimulatory molecules such as CD40. These DCs fail to induce cytokines such as IL-12 that skew the immune response to a Th1 response, and they might even induce Tregs in vivo (90). Along these lines, Sporri and Reis e Sousa demonstrated that DCs activated indirectly by inflammatory mediators supported CD4+ T cell clonal expansion but failed to direct Th cell differentiation (91). By contrast, exposure to pathogen components (TLR agonists) resulted in fully activated DCs that promoted Th cell responses. Therefore, preferential activation of DCs with natural activators such as TLR agonists (particularly when physically linked with antigens to facilitate endosomal processing) might be a preferable way to generate therapeutically useful DCs. DC function might be further improved by inhibiting negative regulatory pathways in the cells or by inducing the cells to express costimulatory molecules and antiapoptotic proteins to enhance viability.
Improving the delivery of antigens to DCs is also required. Although several vehicles have been used for this purpose (viral vectors and apoptotic or necrotic tumor lysates), there is no consensus on the optimal approach, but transfection of human DCs with mRNA encoding tumor antigens is effective at inducing tumor-specific immunity in vitro and in vivo (92). At what stage of DC differentiation antigens should be loaded is also uncertain. Recent studies indicate that immature mouse DCs (unlike macrophages) express few proteases, with reduced capacity for lysosomal degradation (93). In vivo, mouse DCs degrade internalized antigens slowly and retain them for long periods. Evidently this translates into more favorable antigen presentation to both T cells and B cells. Therefore, modification of antigens to resist lysosomal proteolysis might render them more immunogenic when acquired by immature DCs (94). Other issues in the design of DC-based immunotherapies include the type(s) of antigen to be administered, the number of DCs to use per vaccination, the frequency of vaccinations, the mode and site of injection, and the utility of targeting DCs in situ with TLR agonists in place of the whole-cell approach. Finally, before venturing into making numerous improvements, it should be considered whether activated “mature” DCs are superior to other vaccine adjuvants, especially those in long-standing use.
Adoptive T cell immunotherapy.
The final article in this Review series, by Carl June, summarizes key advances in the adoptive transfer of T cells to humans, advances that have led to tumor regression in early-stage clinical trials (95). The challenges faced by immunologists using adoptive T cell therapy relate not only to generating large numbers of cells for transfusion, but also to developing cells that have specificity for tumor antigens; retain proliferative, homing, and effector function; and can engraft long-term. The ability to transfer central memory T cells with stem cell–like self-renewing qualities and that rapidly acquire effector function remains a challenge (96). Likewise, it is not apparent that immunotherapies will reach the level of potency required to eliminate the cancer stem cells that are responsible for initiating and sustaining tumor growth.
Nevertheless, the effectiveness of tumor-specific T cell adoptive transfer, which has shown promise in treating virus infections after transplantation (97, 98), has been enhanced by certain manipulations. For example, nonmyeloablative lymphodepletion prior to adoptive T cell transfer allows the transferred T cells to undergo homeostasis-driven proliferation in response to increased synthesis and accessibility to the endogenous growth factors (99). This is illustrated by the dramatic regression of some tumors that is seen following the adoptive transfer and clonal expansion of tumor-infiltrating lymphocytes recognizing melanoma-associated antigens and administration of IL-2 (100–102). Results from animal models have indicated that antitumor activity can be further enhanced by vaccination (e.g., with DCs) at the time of, or following, adoptive T cell transfer (103). In addition, vaccination might be useful in the pretransplantation setting in order to obtain and expand T cells ex vivo for adoptive T cell therapy after HSC transplantation. As demonstrated by June, adoptive transfer of pathogen-specific T cells that had been expanded ex vivo after in vivo vaccination resulted in the rapid enhancement of immunity specifically for a central memory compartment in humans (104). Booster immunization with these T cells also reduced the transplantation-associated immunodeficiency associated with myelodepletion. Moreover, the combination of myeloablative treatment and HSC transplantation was shown to be superior to nonmyeloablative treatment prior to adoptive T cell therapy in inducing antitumor responses, by driving T cell expansion and function (105). This was the case even if stem cells were administered in the latter situation, where the antitumor T cell/host cell ratios were ultimately less favorable than in myeloablated animals.
The next decade is likely to see the implementation of several strategies to propel adoptive T cell therapy into the mainstream, including the use of tumor antigen–specific TCR gene transduction of T cells, which may enhance immunity (106).
Synergizing immunotherapy with novel interventions.
It is unlikely that vaccines alone will successfully induce the regression of bulky tumors. As alluded to in several articles in this Review series, consideration is being given to combining vaccines (DC or otherwise) and immunotherapies with other approaches. Some of the more promising strategies involve the coadministration of agonistic antibodies specific for the costimulatory molecules that are expressed on activated T cells (107). Antagonistic antibodies specific for the coinhibitory receptors CTLA4 and programmed death 1 (PD1) (108) are also being evaluated. In mouse models, CTLA4-specific antibody, in combination with cancer vaccines (e.g., a GM-CSF–transduced tumor cell vaccine), functions in a cell-intrinsic manner on both effector T cells and Tregs to increase the rejection of poorly immunogenic tumors. The net effect is greater infiltration of tumor-reactive T cells in the tumor and a change in the balance of effector T cells and Tregs (in favor of the effector T cells) at this site (109). CTLA4 blockade might also release DCs from B7-mediated engagement, with either effector T cells or Tregs, which causes the induction of IDO and immune suppression due to tryptophan depletion and the production of proapoptotic factors (110). In humans, CTLA4 blockade increased tumor immunity in a number of previously vaccinated cancer patients (111) and was associated with objective tumor regression in some melanoma patients who received peptide/adjuvant vaccines (112), although it was accompanied by serious side effects in some cases (hypophysitis and enterocolitis). An ongoing phase III clinical trial will resolve whether CTLA4-specific antibodies as a single agent or administered in combination with peptide vaccine are efficacious in treating metastatic melanoma.
T cells become functionally impaired in chronic viral infections and in the tumor setting and express high levels of PD1, an inhibitory molecule induced after T cell activation (113). PD1 interacts with B7-H1 (also known as PDL1) and B7-DC (also known as PDL2) (16, 114). It has been appointed a marker of disease progression in HIV infection, as it correlates positively with plasma viral load and inversely with CD4+ T cell numbers (115). Blockade with antibodies specific for B7-H1 augmented HIV-specific CD4+ and CD8+ T cell function in vitro (115–117). Similar analyses of T cells in the tumor setting are being undertaken. B7-H1 has been shown to be expressed by mouse melanoma cells, and their in vivo growth was inhibited by administering B7-H1–specific antibody (114). PD1 blockade is currently being evaluated in humans, and it remains to be seen whether blockade of other functionally related coinhibitory molecules, such as B7-H3, B7-H4 (also known as B7x), B and T lymphocyte attenuator (BTLA), and the recently described V-set and Ig domain–containing 4 (VSIG4) (118) will achieve antitumor effects in humans.
Although not addressed in this Review series, the success of monoclonal antibodies as immune therapies for treating cancers should be acknowledged. Rituximab (Rituxan), which is specific for CD20, was the first monoclonal antibody approved to treat malignancy (non-Hodgkin lymphoma), and has been followed by several others. These include the HER2-specific antibody trastuzumab (Herceptin), which is used to treat individuals with HER2/neu-expressing metastatic breast cancer, as well as the EGF-specific antibody cetuximab (Erbitux) and the VEGF-specific antibody bevacizumab (Avastin), both of which are used to treat individuals with colon cancer (119). The mechanisms by which these antibodies work include antibody-dependent cellular cytotoxicity, direct cytotoxic activity, and inhibition of receptor signaling. In some cases the antibodies have been rendered more effective through linking to toxins or radionuclides or by combination with chemotherapy.
Finally, one should point out the immune consequences of chemotherapy and radiation, which can render tumors immunogenic through cross-presentation; enhance MHC class I expression (120); increase the expression of ligands for NK cells (121); and enhance NK cell activity (122). Along these lines, sensitizing tumor stromal cells by radiation or chemotherapy can lead to eradication of established cancer by adoptively transferred T cells (123). Certain chemotherapeutics (e.g., anthracyclins) can render tumor cells immunogenic through preapoptotic translocation of calreticulin to the cell surface, which facilitates their uptake by DCs and activation of T cells by cross-presentation (124). Developing approaches to manipulate these conventional cancer therapies to prime immunity, especially in combination with other interventions, is an exciting endeavor for the future.
Footnotes
Nonstandard abbreviations used: CpG ODN, oligodeoxynucleotide(s) containing one or more unmethylated CpG dinucleotides; CTLA4, cytotoxic T lymphocyte–associated antigen 4; IDO, indoleamine 2,3-dioxygenase; MDSC, myeloid-derived suppressor cell; PD1, programmed death 1.
Conflict of interest: N. Bhardwaj has served as a member of the Scientific Advisory Boards of CERUS and Pfizer and is a coinventor on patents relating to the use of DCs as immune adjuvants.
Citation for this article: J. Clin. Invest. 117:1130–1136 (2007). doi:10.1172/JCI32136.
References
- 1.Ehrlich P. Über den jetzigen Stand der Karzinomforschung [In German]. Ned. Tijdschr. Geneeskd. 1909;5:273–290. [Google Scholar]
- 2.Burnet M. Immunological factors in the process of carcinogenesis. Br. Med. Bull. 1964;20:154–158. doi: 10.1093/oxfordjournals.bmb.a070310. [DOI] [PubMed] [Google Scholar]
- 3. Thomas, L. 1959. Reactions to homologous tissue antigens in relation to hypersensitivity [discussion]. InCellular and humoral aspects of the hypersensitive states. H.S. Lawrence, editor. Hoeber-Harper. New York, New York, USA. 529–532. [Google Scholar]
- 4.Dunn G.P., Bruce A.T., Ikeda H., Old L.J., Schreiber R.D. Cancer immunoediting: from immunosurveillance to tumor escape. Nat. Immunol. 2002;3:991–998. doi: 10.1038/ni1102-991. [DOI] [PubMed] [Google Scholar]
- 5.Shankaran V., et al. IFNγ and lymphocytes prevent primary tumour development and shape tumour immunogenicity. Nature. 2001;410:1107–1111. doi: 10.1038/35074122. [DOI] [PubMed] [Google Scholar]
- 6.Street S.E., et al. Innate immune surveillance of spontaneous B cell lymphomas by natural killer cells and gammadelta T cells. J. Exp. Med. 2004;199:879–884. doi: 10.1084/jem.20031981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunn G.P., Old L.J., Schreiber R.D. The three Es of cancer immunoediting. Annu. Rev. Immunol. 2004;22:329–360. doi: 10.1146/annurev.immunol.22.012703.104803. [DOI] [PubMed] [Google Scholar]
- 8.Swann J.B., Smyth M.J. Immune surveillance of tumors. J. Clin. Invest. 2007;117:1137–1146. doi: 10.1172/JCI31405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Penn I. Tumors of the immunocompromised patient. Annu. Rev. Med. 1988;39:63–73. doi: 10.1146/annurev.me.39.020188.000431. [DOI] [PubMed] [Google Scholar]
- 10.Galon J., et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science. 2006;313:1960–1964. doi: 10.1126/science.1129139. [DOI] [PubMed] [Google Scholar]
- 11.Darnell R.B., Posner J.B. Paraneoplastic syndromes affecting the nervous system. Semin. Oncol. 2006;33:270–298. doi: 10.1053/j.seminoncol.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Crowe N.Y., Smyth M.J., Godfrey D.I. A critical role for natural killer T cells in immunosurveillance of methylcholanthrene-induced sarcomas. J. Exp. Med. 2002;196:119–127. doi: 10.1084/jem.20020092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Schreiber, R., Koebel, C., Vermi, W., Smyth, M., and Old, L.J. 2006. Cancer immunoediting: deciphering the complex interaction of the immune system with developing tumors. Presented at the Cancer Research Institute Annual Meeting on October 4–6, 2006, in New York, New York, USA. S–02. [Google Scholar]
- 14.Blank C., et al. PD-L1/B7H-1 inhibits the effector phase of tumor rejection by T cell receptor (TCR) transgenic CD8+ T cells. Cancer Res. 2004;64:1140–1145. doi: 10.1158/0008-5472.can-03-3259. [DOI] [PubMed] [Google Scholar]
- 15.Brown J.A., et al. Blockade of programmed death-1 ligands on dendritic cells enhances T cell activation and cytokine production. J. Immunol. 2003;170:1257–1266. doi: 10.4049/jimmunol.170.3.1257. [DOI] [PubMed] [Google Scholar]
- 16.Dong H., et al. Tumor-associated B7-H1 promotes T-cell apoptosis: a potential mechanism of immune evasion. Nat. Med. 2002;8:793–800. doi: 10.1038/nm730. [DOI] [PubMed] [Google Scholar]
- 17.Thompson R.H., et al. Costimulatory B7-H1 in renal cell carcinoma patients: indicator of tumor aggressiveness and potential therapeutic target. Proc. Natl. Acad. Sci. U. S. A. 2004;101:17174–17179. doi: 10.1073/pnas.0406351101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Munn D.H., Mellor A.L. Indoleamine 2,3-dioxygenase and tumor-induced tolerance. . J. Clin. Invest. 2007;117:1147–1154. doi: 10.1172/JCI31178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Munn D., et al. Expression of indoleamine 2,3-dioxygenase by plasmacytoid dendritic cells in tumor-draining lymph nodes. J. Clin. Invest. 2004;114:280–290. doi: 10.1172/JCI200421583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grohmann U., et al. IL-6 inhibits the tolerogenic function of CD8α+ dendritic cells expressing indoleamine 2,3-dioxygenase. . J. Immunol. 2001;167:708–714. doi: 10.4049/jimmunol.167.2.708. [DOI] [PubMed] [Google Scholar]
- 21.Orabona C., et al. Toward the identification of a tolerogenic signature in IDO-competent dendritic cells. Blood. 2006;107:2846–2854. doi: 10.1182/blood-2005-10-4077. [DOI] [PubMed] [Google Scholar]
- 22.Munn D.H., Sharma M.D., Mellor A.L. Ligation of B7-1/B7-2 by human CD4(+) T cells triggers indoleamine 2,3-dioxygenase activity in dendritic cells. J. Immunol. 2004;172:4100–4110. doi: 10.4049/jimmunol.172.7.4100. [DOI] [PubMed] [Google Scholar]
- 23.Fallarino F., et al. T cell apoptosis by tryptophan catabolism. Cell Death Differ. 2002;9:1069–1077. doi: 10.1038/sj.cdd.4401073. [DOI] [PubMed] [Google Scholar]
- 24.Frumento G., et al. Tryptophan-derived catabolites are responsible for inhibition of T and natural killer cell proliferation induced by indoleamine 2,3-dioxygenase. J. Exp. Med. 2002;196:459–468. doi: 10.1084/jem.20020121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weber W.P., et al. Differential effects of the tryptophan metabolite 3-hydroxyanthranilic acid on the proliferation of human CD8+ T cells induced by TCR triggering or homeostatic cytokines. Eur J. Immunol. 2006;36:296–304. doi: 10.1002/eji.200535616. [DOI] [PubMed] [Google Scholar]
- 26.Terness P., et al. Inhibition of allogeneic T cell proliferation by indoleamine 2,3-dioxygenase-expressing dendritic cells: mediation of suppression by tryptophan metabolites. J. Exp. Med. 2002;196:447–457. doi: 10.1084/jem.20020052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Munn D.H., et al. GCN2 kinase in T cells mediates proliferative arrest and anergy induction in response to indoleamine 2,3-dioxygenase. Immunity. 2005;22:633–642. doi: 10.1016/j.immuni.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 28.Mellor A.L., et al. Cutting edge: CpG oligonucleotides induce splenic CD19+ dendritic cells to acquire potent indoleamine 2,3-dioxygenase-dependent T cell regulatory functions via IFN type 1 signaling. J. Immunol. 2005;175:5601–5605. doi: 10.4049/jimmunol.175.9.5601. [DOI] [PubMed] [Google Scholar]
- 29.Wingender G., et al. Systemic application of CpG-rich DNA suppresses adaptive T cell immunity via induction of IDO. Eur. J. Immunol. 2006;36:12–20. doi: 10.1002/eji.200535602. [DOI] [PubMed] [Google Scholar]
- 30.Lee J.H., et al. Quantitative analysis of melanoma-induced cytokine-mediated immunosuppression in melanoma sentinel nodes. Clin. Cancer Res. 2005;11:107–112. [PubMed] [Google Scholar]
- 31.Gabrilovich D.I., et al. The terminology issue for myeloid-derived suppressor cells. Cancer Res. 2007;67:425; author reply 426. doi: 10.1158/0008-5472.CAN-06-3037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sica A., Bronte V. Altered macrophage differentiation and immune dysfunction in tumor development. J. Clin. Invest. 2007;117:1155–1166. doi: 10.1172/JCI31422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gallina G., et al. Tumors induce a subset of inflammatory monocytes with immunosuppressive activity on CD8+ T cells. J. Clin. Invest. 2006;116:2777–2790. doi: 10.1172/JCI28828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huang B., et al. Gr-1+CD115+ immature myeloid suppressor cells mediate the development of tumor-induced T regulatory cells and T-cell anergy in tumor-bearing host. Cancer Res. 2006;66:1123–1131. doi: 10.1158/0008-5472.CAN-05-1299. [DOI] [PubMed] [Google Scholar]
- 35.Serafini P., Borrello I., Bronte V. Myeloid suppressor cells in cancer: recruitment, phenotype, properties, and mechanisms of immune suppression. Semin. Cancer Biol. 2006;16:53–65. doi: 10.1016/j.semcancer.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 36.Colombo M.P., Mantovani A. Targeting myelomonocytic cells to revert inflammation-dependent cancer promotion. Cancer Res. 2005;65:9113–9116. doi: 10.1158/0008-5472.CAN-05-2714. [DOI] [PubMed] [Google Scholar]
- 37.De Palma M., et al. Tie2 identifies a hematopoietic lineage of proangiogenic monocytes required for tumor vessel formation and a mesenchymal population of pericyte progenitors. Cancer Cell. 2005;8:211–226. doi: 10.1016/j.ccr.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 38.Muller A.J., Scherle P.A. Targeting the mechanisms of tumoral immune tolerance with small-molecule inhibitors. Nat. Rev. Cancer. 2006;6:613–625. doi: 10.1038/nrc1929. [DOI] [PubMed] [Google Scholar]
- 39.Saccani A., et al. p50 nuclear factor-kappaB overexpression in tumor-associated macrophages inhibits M1 inflammatory responses and antitumor resistance. Cancer Res. 2006;66:11432–11440. doi: 10.1158/0008-5472.CAN-06-1867. [DOI] [PubMed] [Google Scholar]
- 40.O’Shea J.J., Pesu M., Borie D.C., Changelian P.S. A new modality for immunosuppression: targeting the JAK/STAT pathway. Nat. Rev. Drug Discov. 2004;3:555–564. doi: 10.1038/nrd1441. [DOI] [PubMed] [Google Scholar]
- 41.Kortylewski M., et al. Inhibiting Stat3 signaling in the hematopoietic system elicits multicomponent antitumor immunity. Nat. Med. 2005;11:1314–1321. doi: 10.1038/nm1325. [DOI] [PubMed] [Google Scholar]
- 42.Luo Y., et al. Targeting tumor-associated macrophages as a novel strategy against breast cancer. J. Clin. Invest. 2006;116:2132–2141. doi: 10.1172/JCI27648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mirza N., et al. All-trans-retinoic acid improves differentiation of myeloid cells and immune response in cancer patients. . Cancer Res. 2006;66:9299–9307. doi: 10.1158/0008-5472.CAN-06-1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Curiel T.J. Tregs and rethinking cancer immunotherapy. J. Clin. Invest. 2007;117:1167–1174. doi: 10.1172/JCI31202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liston A., Rudensky A.Y. Thymic development and peripheral homeostasis of regulatory T cells. Curr. Opin. Immunol. 2007;19:176–185. doi: 10.1016/j.coi.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 46.Chen W., et al. Conversion of peripheral CD4+CD25- naive T cells to CD4+CD25+ regulatory T cells by TGF-beta induction of transcription factor Foxp3. J. Exp. Med. 2003;198:1875–1886. doi: 10.1084/jem.20030152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fu S., et al. TGF-beta induces Foxp3+ T-regulatory cells from CD4+ CD25- precursors. Am. J. Transplant. 2004;4:1614–1627. doi: 10.1111/j.1600-6143.2004.00566.x. [DOI] [PubMed] [Google Scholar]
- 48.Fantini M.C., et al. Cutting edge: TGF-beta induces a regulatory phenotype in CD4+CD25- T cells through Foxp3 induction and down-regulation of Smad7. J. Immunol. 2004;172:5149–5153. doi: 10.4049/jimmunol.172.9.5149. [DOI] [PubMed] [Google Scholar]
- 49.Wang H., et al. Tumor-specific human CD4+ regulatory T cells and their ligands: implications for immunotherapy. Immunity. 2004;20:107–118. doi: 10.1016/s1074-7613(03)00359-5. [DOI] [PubMed] [Google Scholar]
- 50.Curiel T., et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat. Med. 2004;10:942–949. doi: 10.1038/nm1093. [DOI] [PubMed] [Google Scholar]
- 51.Carreras J., et al. High numbers of tumor-infiltrating FOXP3-positive regulatory T cells are associated with improved overall survival in follicular lymphoma. Blood. 2006;108:2957–2964. doi: 10.1182/blood-2006-04-018218. [DOI] [PubMed] [Google Scholar]
- 52.Alvaro T., et al. Outcome in Hodgkin’s lymphoma can be predicted from the presence of accompanying cytotoxic and regulatory T cells. Clin. Cancer Res. 2005;11:1467–1473. doi: 10.1158/1078-0432.CCR-04-1869. [DOI] [PubMed] [Google Scholar]
- 53.Yurchenko E., et al. CCR5-dependent homing of naturally occurring CD4+ regulatory T cells to sites of Leishmania major infection favors pathogen persistence. J. Exp. Med. 2006;203:2451–2460. doi: 10.1084/jem.20060956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dannull J., et al. Enhancement of vaccine-mediated antitumor immunity in cancer patients after depletion of regulatory T cells. J. Clin. Invest. 2005;115:3623–3633. doi: 10.1172/JCI25947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Steitz J., Bruck J., Lenz J., Knop J., Tuting T. Depletion of CD25(+) CD4(+) T cells and treatment with tyrosinase-related protein 2-transduced dendritic cells enhance the interferon alpha-induced, CD8(+) T-cell-dependent immune defense of B16 melanoma. Cancer Res. 2001;61:8643–8646. [PubMed] [Google Scholar]
- 56.Sutmuller R.P., et al. Synergism of cytotoxic T lymphocyte-associated antigen 4 blockade and depletion of CD25(+) regulatory T cells in antitumor therapy reveals alternative pathways for suppression of autoreactive cytotoxic T lymphocyte responses. J. Exp. Med. 2001;194:823–832. doi: 10.1084/jem.194.6.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Banerjee D.K., Dhodapkar M.V., Matayeva E., Steinman R.M., Dhodapkar K.M. Expansion of FOXP3high regulatory T cells by human dendritic cells (DCs) in vitro and after injection of cytokine-matured DCs in myeloma patients. Blood. 2006;108:2655–2661. doi: 10.1182/blood-2006-03-011353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hussain S.P., Hofseth L.J., Harris C.C. Radical causes of cancer. Nat. Rev. Cancer. 2003;3:276–285. doi: 10.1038/nrc1046. [DOI] [PubMed] [Google Scholar]
- 59.Lin W.-W., Karin M. A cytokine-mediated link between innate immunity, inflammation, and cancer. J. Clin. Invest. 2007;117:1175–1183. doi: 10.1172/JCI31537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Karin M. Nuclear factor-kappaB in cancer development and progression. Nature. 2006;441:431–436. doi: 10.1038/nature04870. [DOI] [PubMed] [Google Scholar]
- 61.Luo J.L., Kamata H., Karin M. IKK/NF-κB signaling: balancing life and death — a new approach to cancer therapy. J. Clin. Invest. 2005;115:2625–2632. doi: 10.1172/JCI26322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hugot J.P., et al. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn’s disease. Nature. 2001;411:599–603. doi: 10.1038/35079107. [DOI] [PubMed] [Google Scholar]
- 63.Eckmann L., Karin M. NOD2 and Crohn’s disease: loss or gain of function? Immunity. 2005;22:661–667. doi: 10.1016/j.immuni.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 64.Kurzawski G., et al. The NOD2 3020insC mutation and the risk of colorectal cancer. Cancer Res. 2004;64:1604–1606. doi: 10.1158/0008-5472.can-03-3791. [DOI] [PubMed] [Google Scholar]
- 65.Luo J.L., Maeda S., Hsu L.C., Yagita H., Karin M. Inhibition of NF-kappaB in cancer cells converts inflammation-induced tumor growth mediated by TNFalpha to TRAIL-mediated tumor regression. Cancer Cell. 2004;6:297–305. doi: 10.1016/j.ccr.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 66.Bommert K., Bargou R.C., Stuhmer T. Signalling and survival pathways in multiple myeloma. Eur. J. Cancer. 2006;42:1574–1580. doi: 10.1016/j.ejca.2005.12.026. [DOI] [PubMed] [Google Scholar]
- 67.Osborne J., Moore P.S., Chang Y. KSHV-encoded viral IL-6 activates multiple human IL-6 signaling pathways. Hum. Immunol. 1999;60:921–927. doi: 10.1016/s0198-8859(99)00083-x. [DOI] [PubMed] [Google Scholar]
- 68.Cozen W., et al. IL-6 levels and genotype are associated with risk of young adult Hodgkin lymphoma. Blood. 2004;103:3216–3221. doi: 10.1182/blood-2003-08-2860. [DOI] [PubMed] [Google Scholar]
- 69.Bongartz T., et al. Anti-TNF antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies: systematic review and meta-analysis of rare harmful effects in randomized controlled trials. JAMA. 2006;295:2275–2285. doi: 10.1001/jama.295.19.2275. [DOI] [PubMed] [Google Scholar]
- 70.Berg D.J., et al. Enterocolitis and colon cancer in interleukin-10-deficient mice are associated with aberrant cytokine production and CD4(+) TH1-like responses. J. Clin. Invest. 1996;98:1010–1020. doi: 10.1172/JCI118861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sellon R.K., et al. Resident enteric bacteria are necessary for development of spontaneous colitis and immune system activation in interleukin-10-deficient mice. Infect. Immun. 1998;66:5224–5231. doi: 10.1128/iai.66.11.5224-5231.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Engle S.J., et al. Elimination of colon cancer in germ-free transforming growth factor beta 1-deficient mice. Cancer Res. 2002;62:6362–6366. [PubMed] [Google Scholar]
- 73.Yu H., Kortylewski M., Pardoll D. Crosstalk between cancer and immune cells: role of STAT3 in the tumour microenvironment. Nat. Rev. Immunol. 2007;7:41–51. doi: 10.1038/nri1995. [DOI] [PubMed] [Google Scholar]
- 74.Doganci A., et al. The IL-6R α chain controls lung CD4+CD25+ Treg development and function during allergic airway inflammation in vivo. . J. Clin. Invest. 2005;115:313–325. doi: 10.1172/JCI200522433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zorn E., et al. IL-2 regulates FOXP3 expression in human CD4+CD25+ regulatory T cells through a STAT-dependent mechanism and induces the expansion of these cells in vivo. Blood. 2006;108:1571–1579. doi: 10.1182/blood-2006-02-004747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hoentjen F., Sartor R.B., Ozaki M., Jobin C. STAT3 regulates NF-kappaB recruitment to the IL-12p40 promoter in dendritic cells. Blood. 2005;105:689–696. doi: 10.1182/blood-2004-04-1309. [DOI] [PubMed] [Google Scholar]
- 77.Schottelius A.J., Mayo M.W., Sartor R.B., Baldwin A.S., Jr. Interleukin-10 signaling blocks inhibitor of kappaB kinase activity and nuclear factor kappaB DNA binding. J. Biol. Chem. 1999;274:31868–31874. doi: 10.1074/jbc.274.45.31868. [DOI] [PubMed] [Google Scholar]
- 78.Nefedova Y., et al. Hyperactivation of STAT3 is involved in abnormal differentiation of dendritic cells in cancer. J. Immunol. 2004;172:464–474. doi: 10.4049/jimmunol.172.1.464. [DOI] [PubMed] [Google Scholar]
- 79.Kao J.H., Chen D.S. Global control of hepatitis B virus infection. Lancet Infect. Dis. 2002;2:395–403. doi: 10.1016/s1473-3099(02)00315-8. [DOI] [PubMed] [Google Scholar]
- 80.Mao C., et al. Efficacy of human papillomavirus-16 vaccine to prevent cervical intraepithelial neoplasia: a randomized controlled trial. Obstet. Gynecol. 2006;107:18–27. doi: 10.1097/01.AOG.0000192397.41191.fb. [DOI] [PubMed] [Google Scholar]
- 81.Krieg A.M. Development of TLR9 agonists for cancer therapy. J. Clin. Invest. 2007;117:1184–1194. doi: 10.1172/JCI31414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Krieg A.M. Therapeutic potential of Toll-like receptor 9 activation. Nat. Rev. Drug Discov. 2006;5:471–484. doi: 10.1038/nrd2059. [DOI] [PubMed] [Google Scholar]
- 83.Speiser D.E., et al. Rapid and strong human CD8+ T cell responses to vaccination with peptide, IFA, and CpG oligodeoxynucleotide 7909. . J. Clin. Invest. 2005;115:739–746. doi: 10.1172/JCI200523373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Appay V., et al. New generation vaccine induces effective melanoma-specific CD8+ T cells in the circulation but not in the tumor site. . J. Immunol. 2006;177:1670–1678. doi: 10.4049/jimmunol.177.3.1670. [DOI] [PubMed] [Google Scholar]
- 85.Manegold C. Addition of PF-3512676 (CpG 7909) to a taxane/platinum regimen for first-line treatment of unresectable non small cell lung cancer (NSCLC) improves objective response — phase II clinical trial. Eur. J. Cancer. 2005;3(Suppl.):326. [Google Scholar]
- 86.Moseman E.A., et al. Human plasmacytoid dendritic cells activated by CpG oligodeoxynucleotides induce the generation of CD4+CD25+ regulatory T cells. J. Immunol. 2004;173:4433–4442. doi: 10.4049/jimmunol.173.7.4433. [DOI] [PubMed] [Google Scholar]
- 87.O’Neill D., Adams S., Bhardwaj N. Manipulating dendritic cell biology for the active immunotherapy of cancer. Blood. 2004;104:2235–2246. doi: 10.1182/blood-2003-12-4392. [DOI] [PubMed] [Google Scholar]
- 88.Lu W., Arraes L., Ferreira W., Andrieu J. Therapeutic dendritic-cell vaccine for chronic HIV-1 infection. Nat. Med. 2004;10:1359–1365. doi: 10.1038/nm1147. [DOI] [PubMed] [Google Scholar]
- 89.Gilboa E. DC-based cancer vaccines. J. Clin. Invest. 2007;117:1195–1203. doi: 10.1172/JCI31205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Morelli A.E., Thomson A.W. Dendritic cells under the spell of prostaglandins. Trends Immunol. 2003;24:108–111. doi: 10.1016/s1471-4906(03)00023-1. [DOI] [PubMed] [Google Scholar]
- 91.Sporri R., Reis e Sousa C. Inflammatory mediators are insufficient for full dendritic cell activation and promote expansion of CD4+ T cell populations lacking helper function. Nat. Immunol. 2005;6:163–170. doi: 10.1038/ni1162. [DOI] [PubMed] [Google Scholar]
- 92.Gilboa E., Vieweg J. Cancer immunotherapy with mRNA-transfected dendritic cells. Immunol. Rev. 2004;199:251–263. doi: 10.1111/j.0105-2896.2004.00139.x. [DOI] [PubMed] [Google Scholar]
- 93.Delamarre L., Pack M., Chang H., Mellman I., Trombetta E.S. Differential lysosomal proteolysis in antigen-presenting cells determines antigen fate. Science. 2005;307:1630–1634. doi: 10.1126/science.1108003. [DOI] [PubMed] [Google Scholar]
- 94.Delamarre L., Couture R., Mellman I., Trombetta E.S. Enhancing immunogenicity by limiting susceptibility to lysosomal proteolysis. . J. Exp. Med. 2006;203:2049–2055. doi: 10.1084/jem.20052442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.June C.H. Principles of adoptive T cell cancer therapy. J. Clin. Invest. 2007;117:1204–1212. doi: 10.1172/JCI31446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sallusto F., Geginat J., Lanzavecchia A. Central memory and effector memory T cell subsets: function, generation, and maintenance. Annu. Rev. Immunol. 2004;22:745–763. doi: 10.1146/annurev.immunol.22.012703.104702. [DOI] [PubMed] [Google Scholar]
- 97.Bollard C.M., et al. In vivo expansion of LMP 1- and 2-specific T-cells in a patient who received donor-derived EBV-specific T-cells after allogeneic stem cell transplantation. Leuk. Lymphoma. 2006;47:837–842. doi: 10.1080/10428190600604724. [DOI] [PubMed] [Google Scholar]
- 98.Leen A.M., et al. Monoculture-derived T lymphocytes specific for multiple viruses expand and produce clinically relevant effects in immunocompromised individuals. Nat. Med. 2006;12:1160–1166. doi: 10.1038/nm1475. [DOI] [PubMed] [Google Scholar]
- 99.Gattinoni L., Powell D.J., Jr., Rosenberg S.A., Restifo N.P. Adoptive immunotherapy for cancer: building on success. Nat. Rev. Immunol. 2006;6:383–393. doi: 10.1038/nri1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dudley M.E., et al. A phase I study of nonmyeloablative chemotherapy and adoptive transfer of autologous tumor antigen-specific T lymphocytes in patients with metastatic melanoma. J. Immunother. 2002;25:243–251. doi: 10.1097/01.CJI.0000016820.36510.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dudley M.E., et al. Cancer regression and autoimmunity in patients after clonal repopulation with antitumor lymphocytes. Science. 2002;298:850–854. doi: 10.1126/science.1076514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dudley M.E., Rosenberg S.A. Adoptive-cell-transfer therapy for the treatment of patients with cancer. Nat. Rev. Cancer. 2003;3:666–675. doi: 10.1038/nrc1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lou Y., et al. Dendritic cells strongly boost the antitumor activity of adoptively transferred T cells in vivo. Cancer Res. 2004;64:6783–6790. doi: 10.1158/0008-5472.CAN-04-1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rapoport A.P., et al. Restoration of immunity in lymphopenic individuals with cancer by vaccination and adoptive T-cell transfer. Nat. Med. 2005;11:1230–1237. doi: 10.1038/nm1310. [DOI] [PubMed] [Google Scholar]
- 105.Wrzesinski C., et al. Hematopoietic stem cells promote the expansion and function of adoptively transferred antitumor CD8+ T cells. . J. Clin. Invest. 2007;117:492–501. doi: 10.1172/JCI30414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Morgan R.A., et al. Cancer regression in patients after transfer of genetically engineered lymphocytes. Science. 2006;314:126–129. doi: 10.1126/science.1129003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Melero I., et al. Monoclonal antibodies against the 4-1 BB T-cell activation molecule eradicate established tumors. Nat. Med. 1997;3:682–685. doi: 10.1038/nm0697-682. [DOI] [PubMed] [Google Scholar]
- 108.Korman A.J., Peggs K.S., Allison J.P. Checkpoint blockade in cancer immunotherapy. Adv. Immunol. 2006;90:297–339. doi: 10.1016/S0065-2776(06)90008-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Quezada S.A., Peggs K.S., Curran M.A., Allison J.P. CTLA4 blockade and GM-CSF combination immunotherapy alters the intratumor balance of effector and regulatory T cells. J. Clin. Invest. 2006;116:1935–1945. doi: 10.1172/JCI27745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Fallarino F., et al. Modulation of tryptophan catabolism by regulatory T cells. Nat. Immunol. 2003;4:1206–1212. doi: 10.1038/ni1003. [DOI] [PubMed] [Google Scholar]
- 111.Hodi F.S., et al. Biologic activity of cytotoxic T lymphocyte-associated antigen 4 antibody blockade in previously vaccinated metastatic melanoma and ovarian carcinoma patients. Proc. Natl. Acad. Sci. U. S. A. 2003;100:4712–4717. doi: 10.1073/pnas.0830997100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Phan G.Q., et al. Cancer regression and autoimmunity induced by cytotoxic T lymphocyte-associated antigen 4 blockade in patients with metastatic melanoma. Proc. Natl. Acad. Sci. U. S. A. 2003;100:8372–8377. doi: 10.1073/pnas.1533209100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Freeman G.J., et al. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J. Exp. Med. 2000;192:1027–1034. doi: 10.1084/jem.192.7.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Iwai Y., et al. Involvement of PD-L1 on tumor cells in the escape from host immune system and tumor immunotherapy by PD-L1 blockade. Proc. Natl. Acad. Sci. U. S. A. 2002;99:12293–12297. doi: 10.1073/pnas.192461099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Day C.L., et al. PD-1 expression on HIV-specific T cells is associated with T-cell exhaustion and disease progression. Nature. 2006;443:350–354. doi: 10.1038/nature05115. [DOI] [PubMed] [Google Scholar]
- 116.Petrovas C., et al. PD-1 is a regulator of virus-specific CD8+ T cell survival in HIV infection. . J. Exp. Med. 2006;203:2281–2292. doi: 10.1084/jem.20061496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Trautmann L., et al. Upregulation of PD-1 expression on HIV-specific CD8+ T cells leads to reversible immune dysfunction. Nat. Med. 2006;12:1198–1202. doi: 10.1038/nm1482. [DOI] [PubMed] [Google Scholar]
- 118.Vogt L., et al. VSIG4, a B7 family–related protein, is a negative regulator of T cell activation. J. Clin. Invest. 2006;116:2817–2826. doi: 10.1172/JCI25673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Waldmann T.A., Morris J.C. Development of antibodies and chimeric molecules for cancer immunotherapy. Adv. Immunol. 2006;90:83–131. doi: 10.1016/S0065-2776(06)90003-0. [DOI] [PubMed] [Google Scholar]
- 120.Reits E.A., et al. Radiation modulates the peptide repertoire, enhances MHC class I expression, and induces successful antitumor immunotherapy. J. Exp. Med. 2006;203:1259–1271. doi: 10.1084/jem.20052494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Armeanu S., et al. Natural killer cell-mediated lysis of hepatoma cells via specific induction of NKG2D ligands by the histone deacetylase inhibitor sodium valproate. Cancer Res. 2005;65:6321–6329. doi: 10.1158/0008-5472.CAN-04-4252. [DOI] [PubMed] [Google Scholar]
- 122.Borg C., et al. Novel mode of action of c-kit tyrosine kinase inhibitors leading to NK cell–dependent antitumor effects. J. Clin. Invest. 2004;114:379–388. doi: 10.1172/JCI200421102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhang B., et al. Induced sensitization of tumor stroma leads to eradication of established cancer by T cells. J. Exp. Med. 2007;204:49–55. doi: 10.1084/jem.20062056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Obeid M., et al. Calreticulin exposure dictates the immunogenicity of cancer cell death. Nat. Med. 2007;13:54–61.. doi: 10.1038/nm1523. [DOI] [PubMed] [Google Scholar]