Summary
Screening for distress in cancer patients is recommended by the National Comprehensive Cancer Network, and a Distress Thermometer has previously been developed and empirically-validated for this purpose. The present study sought to determine the rates and predictors of distress in a sample of patients being seen in a multidisciplinary lung cancer clinic. Consecutive patients (N = 333) were recruited from an outpatient multidisciplinary lung cancer clinic to complete the Distress Thermometer, an associated Problem Symptom List, and two questions about interest in receiving help for symptoms. Over half (61.6%) of patients reported distress at a clinically significant level, and 22.5% of patients indicated interest in receiving help with their distress and/or symptoms. Problems in the areas of family relationships, emotional functioning, lack of information about diagnosis/treatment, physical functioning, and cognitive functioning were associated with higher reports of distress. Specific symptoms of depression, anxiety, pain and fatigue were most predictive of distress. Younger age was also associated with higher levels of distress. Distress was not associated with other clinical variables, including stage of illness or medical treatment approach. Similar results were obtained when individuals who had not yet received a definitive diagnosis of lung cancer (n = 134) were excluded from analyses; however, family problems and anxiety were no longer predictive of distress. Screening for distress in a multidisciplinary lung cancer clinic is feasible and a significant number of patients can be expected to meet clinical criteria for distress. Results also highlight younger age and specific physical and psychosocial symptoms as predictive of clinically-significant distress. Identification of the presence and predictors of distress are the first steps toward appropriate referral and treatment of symptoms and problems that contribute to cancer patients’ distress.
Keywords: psychological distress, screening, lung cancer, Distress Thermometer, predictors
1. Introduction
The consensus-based guidelines set forth by the Distress Management Panel of the National Comprehensive Cancer Network (NCCN) include a recommendation for comprehensive distress screening for all patients at their initial visit and across the disease continuum [1,2]. Distress has been defined as “a multifactorial, unpleasant experience of an emotional, psychological, social, or spiritual nature that interferes with the ability to cope with cancer, its physical symptoms, and its treatment” [1,2]. In the oncology context, distress is multifactorial, as numerous areas in a patient’s life contribute to his or her experience of distress, including physical symptoms, disease severity, treatment [3,4]; physical activity level / performance status [5–7]; social support (for a review see [8]); and psychological factors such as optimism [9,10], coping style [11,12], and pre-morbid or current depression [13].
In addition to the above factors, rates of distress often vary depending on age, sex, and site of cancer [11,14–16]. Younger patients and women report higher levels of distress [7,11,14,15], and individuals with lung cancer, compared to individuals with other cancer diagnoses, also report higher levels of distress [15,17]. Approximately 43% of patients with lung cancer report clinically-significant levels of distress [15,18], compared to about 33% of patients with breast cancer and 32% of patients with colon cancer [15].
Just as lung cancer patients are more likely to experience distress than other cancer patients, having a diagnosis of lung cancer was predictive of oncologists’ failure to correctly identify distress [19]. Categorizing distress as mild, moderate, or severe, oncologists inaccurately identified distress in 68% of patients with lung cancer (compared to 52% for other cancers with the exception of head and neck cancer, which was also high at 67%[19]). Distress and other psychosocial symptoms may not be accurately identified by oncology health care professionals for several reasons. Given the medical focus on physical symptoms and treatment, emotional and psychological symptoms may be overlooked or discounted. Physicians cite lack of time and lack of confidence as barriers to detecting certain physical and psychosocial symptoms [20]. Symptoms that practitioners may under- or misidentify include depression, pain, fatigue, and overall quality of life concerns [21–26]. Patients may be embarrassed or reluctant to report psychological problems, such as depressive symptoms [27]. Less than one in four patients with psychological problems spontaneously disclose those problems to their treatment team because of concerns about bothering the nurses or physicians or fear of being stigmatized for having an emotional problem [28]. As a result of both physician and patient barriers toward the reporting and identification of distress symptoms, such concerns may go untreated.
Left untreated, significant levels of distress may contribute not only to lower quality of life and lower satisfaction with care [29], but also to poorer adherence to treatment recommendations and possibly decreased survival [30–32]. In recognition of the potential impact of untreated distress, guidelines from the NCCN suggest:
Distress should be recognized, monitored, documented, and treated promptly at all stages of disease. All participants should be screened for distress at their initial visit, at appropriate intervals, and as clinically indicated, especially with changes in disease status (i.e., remission, recurrence, progression) [1].
1.1. Measuring Distress
The Distress Thermometer (DT) is a visual-analog tool developed to efficiently screen for distress in cancer patients [7,33–35]. The sensitivity, specificity, and appropriate cut-off score of the DT are established [16], with scores of 4 or above indicative of clinically-significant levels of distress. Through receiver operating characteristic (ROC) curve analyses, Jacobsen and colleagues compared scores on the DT to evidence-based cut-off scores on psychometrically valid measures of distress, the Brief Symptom Inventory and the Hospital Anxiety and Depression Scale [16]. Females and patients with lower self-reported performance status had higher levels of clinically-significant distress. No other demographic or clinical variables, including stage of disease or type of treatment, were associated with scoring 4 or higher on the DT. The DT thus represents a brief measure that is both sensitive and specific to detecting distress in individuals with cancer.
The DT has been used to evaluate distress in patients diagnosed with prostate cancer [33], patients undergoing bone marrow transplant [34], and ambulatory cancer patients with mixed cancer diagnoses [7,16,35]. Categories of symptoms consistently associated with clinically-significant levels of distress on the DT were emotional, family, and physical problems. Inconsistent results were found for the relationship between clinically-significant distress and spiritual problems [16,35]. In addition to clarifying the problem categories that contribute most to distress, researchers have called for future studies to focus on homogeneous diagnostic groups [35] and expansion of the symptom problem list frequently used with the DT to include a format for patients to identify other potential sources of distress and/or the issues for which they would most like help [16]. The present study addresses these issues through our focus on patients evaluated and treated in a lung cancer clinic and through the adaptation of the Symptom Problem List (see section 2.3.3 under Measures).
1.2. Studying Distress Screening in a Multidisciplinary Lung Cancer Program
In prior research on the DT with ambulatory cancer patients, less than 100 lung cancer patients participated across three studies [7,16,35]. Given that lung cancer is the leading cause of cancer-related death for women and men [36], additional information on rates and predictors of distress in this population is needed. Recent worldwide estimates indicate that lung cancer remains the most frequently diagnosed cancer (1.35 million in 2002) and the leading cause of cancer deaths worldwide (1.18 million in 2002; [37]). One year relative survival rates for lung cancer patients have increased from 37% in 1975 to 42% in 2000; however, the 5-year relative survival rate for all stages of lung cancer is only 15.2%, compared to 5-year relative survival rates of 87.7% for breast cancer and 63.4% for colorectal cancer [36].
Even with a conservative estimate of the percentage of patients experiencing distress (e.g., 20% compared with the documented rate of 43% in lung cancer patients [15]), hundreds of thousands of patients with lung cancer likely experience clinically-significant distress. Despite the large numbers of lung cancer patients and high rates of distress in this population, specific predictors of distress and its overall prevalence remain understudied in lung cancer patients [13]. In the largest study to date documenting rates of distress across different cancer sites, Zabora and colleagues highlighted patients with lung cancer as a group at high risk for experiencing distress and emphasized that “special attention in terms of early detection and intervention [of distress in lung cancer patients] is warranted” [15, p. 26].
Thus, in the present study, we sought to establish the rates and predictors of distress in a sample of patients seeking care in an outpatient multidisciplinary lung cancer clinic. The primary objectives were to 1) document rates of overall and clinically-significant distress in an outpatient lung cancer clinic sample and 2) evaluate the demographic, clinical, and symptomatic predictors of overall distress and clinically-significant distress. A secondary aim was to evaluate the clinical, demographic, and symptomatic predictors of the desire for clinical services to help with distress.
2. Method
2.1. Participants
Participants were consecutive patients who were seen in the Multidisciplinary Lung Cancer Program (MLCP) at Markey Cancer Center, Lexington, Kentucky. Eligibility criteria were ≥ 18 years of age, appointment with a MLCP physician (cardiothoracic surgeon, pulmonologist, medical oncologist, or medical radiologist), ability to speak English, and willingness to complete the DT. Patients were seen in the MLCP for evaluation of symptoms, consultation by a MLCP team member, or routine post-operative or treatment follow-up. Approximately 60% of all clinic visits to the MLCP consist of new patients or individuals presenting for the first time to this clinic.
2.2. Procedure
Patients were approached by either a clinical psychology postdoctoral fellow or another trained member of the Symptom Management and Palliative Care team to complete a DT. The DTs were completed by the patient or through a face-to-face brief interview while the patient waited to be seen by a physician, either in the outpatient waiting room or in an examination room. Patients completed the DTs as part of routine clinical care to detect those in need of referral to the Symptom Management and Palliative Care Program. Patients who attended the clinic more than once were screened only one time.
Clinical data was extracted from medical records and only those patients for whom associated medical records could be reviewed were included in the present sample. Medical record data in this study was collected and analyzed after approval from the University of Kentucky's Institutional Review Board for use of existing medical records. All data was de-identified and analyzed in aggregate form.
2.3. Measures
2.3.1. Demographic and Clinical Characteristics
Information on participants’ age and sex was collected at the time the DT was completed in clinic. Additional demographic and clinical data was extracted from medical charts: race, zip code (to determine rurality of residence based on the 2003 Rural-Urban Coding System, [38]), diagnosis/stage at time of distress screening, and treatment at time of distress screening.
2.3.2. Distress Thermometer
The DT is a single-item self-report measure of distress [7,16,33–35]. Patients mark their level of distress on a picture of a thermometer, with endpoints of no distress (0) and extreme distress (10; See Figure 1). The DT has good reliability and is significantly correlated with the Hospital Anxiety and Depression Scale [7] and the Brief-Symptom Inventory [33]. ROC analyses demonstrated that with a cut-off score of 4, the DT had a sensitivity of α = 0.70 and specificity of α = 0.70 for detecting clinical levels of distress [16].
FIGURE 1.
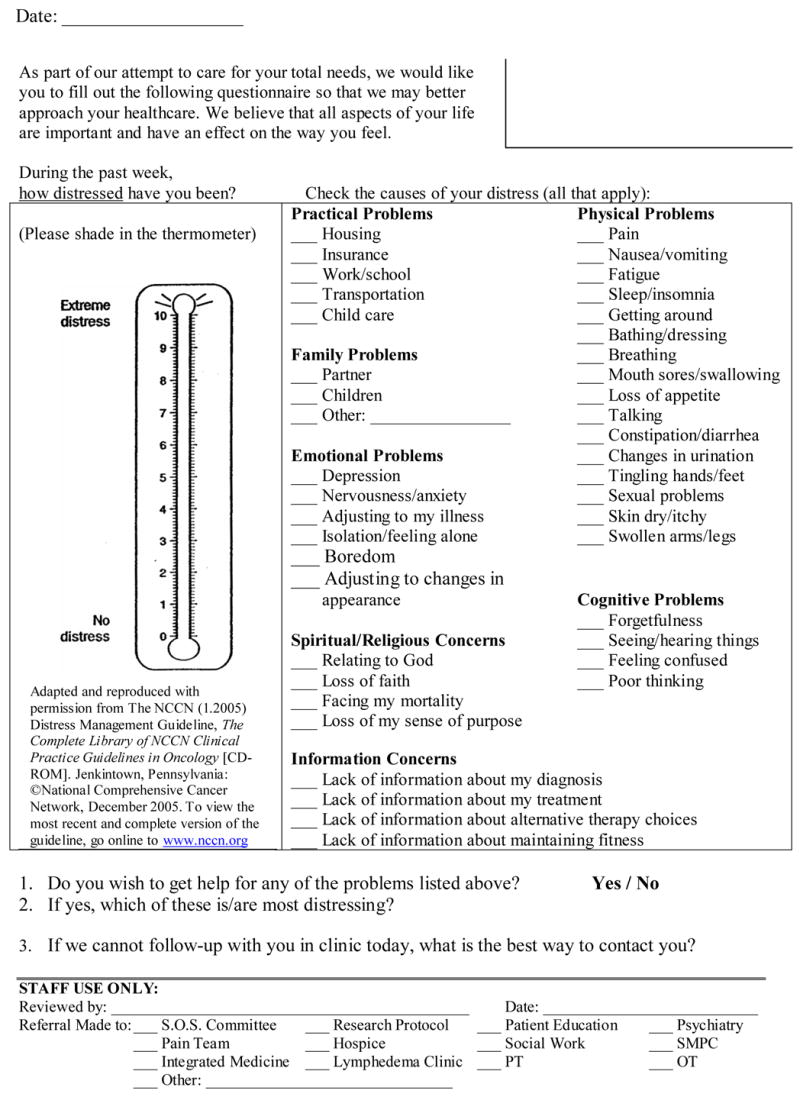
Distress Thermometer and Symptom Problem List. These guidelines are a work in progress that will be refined as often as new significant data becomes available. The NCCN Guidelines are a statement of consensus of its authors regarding their views of currently accepted approaches to treatment. Any clinician seeking to apply or consult any NCCN guideline is expected to use independent medical judgment in the context of individual clinical circumstances to determine any patient’s care or treatment. The National Comprehensive Cancer Network makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. These Guidelines are copyrighted by the National Comprehensive Cancer Network. All rights reserved. These Guidelines and illustrations herein may not be reproduced in any form for any purpose without the express written permission of the NCCN.
2.3.3. Problem Symptom List
The Problem List developed by the Distress Management Guidelines Panel of the NCCN [39] was adapted for the present study. Specifically, the Problem Symptom List used in the current study contained 42 problems frequently experienced by individuals with cancer, retaining 27 of the 34 items on the original Problem List and adding 17 additional problems1. The 42 problems are classified into seven categories: Practical Problems, Family Problems, Emotional Problems, Spiritual/ Religious Concerns, Information Concerns, Physical Problems, and Cognitive Problems (see Figure 1).
2.3.4. Interest in Help
Two items were used to determine the patient’s interest in obtaining services for distress: “Do you wish to get help for any of the problems listed above?” answered with a Yes/No response, and “If yes, which of these is/are the most distressing?” allowing the patient to write in the most distressing problem(s).
2.3.5. Predictors of Distress
The variables evaluated as predictors of distress consisted of demographic variables (age, sex, race, rurality of residence), clinical variables (diagnosis and treatment at time of distress screening), and number and type of problems checked. For new patients or individuals being evaluated for a lung cancer diagnosis, treatment type was defined as surgical consult (see Table 1). Problems from the Symptom Problem List were evaluated as both individual problem items (e.g., insurance, partner, nervousness, loss of faith, lack of information about my diagnosis, insomnia, forgetfulness) and categories of problems (Practical Problems, Family Problems, Emotional Problems, Spiritual/Religious Concerns, Information Concerns, Physical Problems, and Cognitive Problems).
Table 1.
Sample Clinical Characteristics (N = 333)
| Variable | Number of Patients (%) |
|---|---|
| Lung Cancer Diagnosis / Stage Information at time of Screening | |
| Stage I | 1 (0.3) |
| Stage II | 10 (3.0) |
| Stage III | 7 (2.1) |
| Stage IV | 72 (21.6) |
| Lung Diagnosis, diagnostic information unknown | 39 (11.7) |
| Lung Diagnosis, Small Cell Lung Cancer, stage unknown | 13 (3.9) |
| Lung Diagnosis, Non-Small Cell Lung Cancer, stage unknown | 57 (17.1) |
| Evaluation of Lung Mass or Symptoms; Dx, stage unknown | 134 (40.2) |
| Treatment type categorization at time of Screening | |
| Routine follow-up, stable condition | 32 (9.6) |
| Surgery / Surgery follow-up | 71 (21.3) |
| Surgery Consult | 134 (40.2) |
| Chemotherapy | 12 (3.6) |
| Radiation | 1 (0.3) |
| Surgery and Radiation | 10 (3.0) |
| Surgery and Chemotherapy | 33 (9.9) |
| Radiation and Chemotherapy | 12 (3.6) |
| Surgery, Chemotherapy and Radiation | 28 (8.4) |
Dx = Diagnosis
2.4. Data Analysis
Problem totals were calculated by creating sum scores for the number of items checked in each problem category. Standard descriptive statistics were generated to characterize the sociodemographic, clinical, distress, and problem variables in the sample. To evaluate bivariate relationships, we used Pearson’s χ2 tests (for relationships between two dichotomous variables and between dichotomous and nominal variables), t tests (for relationships between dichotomous and continuous variables), and Pearson’s correlation coefficients (for relationships between two continuous variables). We used linear regression to evaluate predictors of overall distress, controlling for variables with significant bivariate associations with distress. We used logistic regression to separately evaluate predictors of clinically significant distress (distress level ≥ 4 or distress level < 4), extreme distress (distress level = 10 or distress level < 10), and interest in help (yes versus no), again controlling for variables with bivariate associations with these outcomes.
3. Results
3.1. Demographic and Clinical Characteristics
DTs were collected from 415 patients in the MLCP as part of routine clinical care. Less than 3% of approached patients declined to complete a DT. These patients did not differ from completers on age or sex. Medical data was not collected on decliners and thus we were unable to compare decliners to completers on any medical data. Of the 415 patients completing DTs, 25 (6% of sample) were excluded from analyses due to missing or unavailable medical record data. These participants did not differ from those included in the analyses on age, sex, date of screening, or overall distress level. Another 57 (13.7%) patients were excluded from analyses because they were being evaluated in the MLCP for metastases to the lung from a primary cancer diagnosis other than lung cancer.
Of the 333 participants in the present sample, 50.8% were female, 94% were Caucasian (6% African American), and 56.5% lived in an area defined as rural by the 2003 Rural-Urban Coding System. Participants had a mean age of 60.6 years (SD = 11.1 years, range 22 to 89 years). Clinical characteristics (treatment type, stage information) are presented in Table 1. Over half of the participants screened for distress (60%) were presenting for the first time to the MLCP. Of participants being seen in the clinic for the first time, a proportion were being evaluated for lung cancer due to the presence of a lung mass or other suggestive lung symptoms and had not yet received a definitive diagnosis of lung cancer (n = 134, 40.2%).
3.2. Rates of Distress in the Multidisciplinary Lung Cancer Program
3.2.1. Rates of Overall Distress
The mean level of distress on the 0 to 10 DT scale was 4.56 (SD = 2.99) and the mean number of symptoms checked (out of 42 total) was 7.77 (SD = 5.56; see Table 2 for percentage of patients reporting distress in each problem category). The most frequently reported symptoms were fatigue (55.6%), pain (51.4%), nervousness/anxiety (48.6%), problems with breathing (43.2%), sleep/insomnia (39.9%), and depression/sadness (35.4%). Statistically significant correlations emerged between distress level and number of problems (r = .51, p < .001), distress level and wanting help (t (331) = − 5.98, p < .001), and number of problems and wanting help (t (331) = −6.8, p < .001), with more problems and greater distress related to wanting help.
Table 2.
Percentage of Participants Indicating Distress in Problem Categories
| Category | Overall Sample (N = 333) | Clinically-Significant Distress Group (Scoring 4 or Above on DT, n = 205) |
|---|---|---|
| Any Practical Problems | 26.7 | 30.2 |
| Any Family Problems | 14.6 | 18.5 |
| Any Emotional Problems | 68.8 | 80.0 |
| Any Spiritual / Religious Concerns | 13.3 | 16.1 |
| Any Information Concerns | 24.6 | 30.7 |
| Any Physical Problems (4 or more) | 90.7 (39.3) | 96.1 (50.7) |
| Any Cognitive Problems | 40.8 | 50.7 |
| Wants Help with Problems | 22.5 | 29.3 |
DT = Distress Thermometer
3.2.2 Rates of Clinically-Significant Distress
Using the cut-off score of 4, more than half (61.6%; n = 205) of the patients screened reported experiencing distress at or above this clinically significant level. Of the patients reporting distress at a level of 4 or more, the most common symptoms reported were fatigue (65.4%), pain (64.9%), nervousness/anxiety (62.4%), problems with breathing (52.7%), depression/sadness (49.3%), and sleep/insomnia (48.3%). Less than one-third (29.3%) wanted help with their distress and reported that they experienced, on average, 9.6 symptoms (SD = 5.6, see Table 2 for percentage of patients reporting distress in each problem category).
A small percentage (9.8%; n = 20) of the patients reported distress at a level of 10, indicating extreme distress. Compared to patients who reported distress at levels below 10 (0 to 9), individuals reporting this level of extreme distress were statistically more likely to indicate interest in services (55% vs. 20%), report a larger number of total problems (15 vs. 7 problems), and endorse more problems in the areas of cognitive, physical, psychosocial, and information concerns (all ps < .05).
3.4. Predictors of Distress
3.4.1. Demographic and Clinical Correlates of Distress
Age was related to overall distress (r = −.14, p = .01), with younger age related to higher levels of distress. No other demographic (sex, race, rurality of residence) or clinical (stage of disease, treatment type) variables were related to overall distress. Age was also statistically related to clinically-significant levels of distress, with younger patients more likely to report clinically-significant levels of distress (t (331) = 2.48, p = .014). Similar to associations with overall distress, no other demographic or clinical variables were related to clinically-significant levels of distress. Likewise, only age was significantly related to wanting help (t (331) = 2.72, p = .007), with younger age being more indicative of wanting help with symptoms.
3.4.2. Predictors of Overall Distress
We first used categories of problems to predict distress, with the final regression model (age, total number of problems with practical concerns, family relationships, emotional functioning, religious/spiritual concerns, lack of information, physical functioning, and cognitive functioning) accounting for 31.1% of the variance in reported distress level (see Table 3). After eliminating non-significant predictors, the final model included family relationship problems, emotionalproblems, problems related to lack of information, physical problems, and cognitive problems and accounted for 31.0% of the variance in reported distress level.
Table 3.
Hierarchal Regression Analyses of Problem Categories and Specific Symptoms as Predictors of Overall Distress (N = 333)
| Problem Category Variables | ΔR2 | βa | p | Specific Symptom Variables | ΔR2 | βa | p |
|---|---|---|---|---|---|---|---|
| Block 1 | 0.020 | Block 1 | 0.020 | ||||
| Age | −.142 | .010 | Age | −.142 | .010 | ||
| Block 2 | 0.291 | Block 2 | 0.278 | ||||
| Age | −.114 | .021 | Age | −.100 | .036 | ||
| Total Practical Problems | −.028 | .583 | Depression/sadness | .232 | .000 | ||
| Total Relationship Problems | .102 | .030 | Nervousness/anxiety | .171 | .002 | ||
| Total Emotional Problems | .280 | .000 | Pain | .189 | .000 | ||
| Total Religious/Spiritual Problems | −.010 | .837 | Fatigue | .141 | .007 | ||
| Total Lack of Information Problems | .098 | .043 | Sleep or insomnia | .057 | .256 | ||
| Total Physical Problems | .162 | .005 | Breathing | −.008 | .886 | ||
| Total Cognitive Problems | .163 | .004 | |||||
| Full model statistics | Full model statistics | ||||||
| Multiple R | 0.557 | Multiple R | 0.546 | ||||
| Multiple R2 | 0.311 | Multiple R2 | 0.298 | ||||
| F | 18.263b | .000 | F | 19.691c | .000 |
Standardized regression coefficients in full model.
df = 8, 324.
df = 7, 325.
We then used specific symptoms rather than total categories of problems to predict distress (see Table 3). This regression model accounted for 29.8% of the variance of distress level. After eliminating non-significant predictors, the final model included depression/sadness, nervousness/anxiety, pain, and fatigue, and accounted for 29.5% of the variance in reported distress level. Sleep/insomnia (β = .06, p = .26) and breathing problems (β = −.01, p = .88) were not significant predictors of distress in the final model.
As a proportion of our participants had not yet received a definitive diagnosis of lung cancer (n = 134, 40.2%), we re-analyzed our data without these participants. Results were the same in the final model with the exception that problems related to lack of information about diagnosis or treatment were non-significant (β = .04, p = .52), and cognitive problems were only marginally related to overall distress (β = .12, p = .07).
3.4.3. Predictors of Clinically-Significant Distress
To evaluate predictors of clinical distress (i.e., distress at or above the cutoff score of 4), we used logistic regression with hierarchical variable entry. Two logistic regression analyses were conducted, as identification of both the problem categories and the specific symptoms predictive of distress is conceptually and clinically meaningful, respectively. Results are presented in Table 4. Younger age was predictive of clinical distress in both the category- and specific-symptom logistic regression models. Predictors of clinical distress at the category-level included problems in the areas of family relationships (OR = 2.14, 95% CI = 1.06 to 4.32), and emotional (OR = 1.53, 95% CI = 1.20 to 1.95), physical (OR = 1.12, 95% CI = 1.05 to 1.32), and cognitive symptoms (OR = 1.56, 95% CI = 1.10 to 2.22). Significant symptom predictors of whether an individual reported distress at or above the cut-off of 4 on the DT were depression (OR = 3.14, 95% CI = 1.62 to 6.09), anxiety (OR = 1.99, 95% CI = 1.12 to 3.53), and pain (OR = 2.60, 95% CI = 1.53 to 4.42). We again repeated the analyses removing those participants (n = 134) without a definitive diagnosis of lung cancer. Results were very similar, although for categories of problems, family relationship problems were no longer a significant predictor of clinical distress. For specific symptoms, anxiety was no longer predictive of clinical distress after excluding participants without a definitive lung cancer diagnosis.
Table 4.
Logistic Regression Analyses of Problem Categories and Specific Symptoms as Predictors of Clinically-Significant Distress
| Characteristic/Problem Categorya | OR | 95% CI | Characteristic/Specific Symptomb | OR | 95% CI |
|---|---|---|---|---|---|
| Age | 0.97 | 0.94 to 0.99 | Age | 0.98 | 0.95 to 0.99 |
| Total Practical Problems | 1.02 | 0.66 to 1.58 | Depression/sadness | 3.14 | 1.62 to 6.09 |
| Total Relationship Problems | 2.14 | 1.06 to 4.32 | Nervousness/anxiety | 1.99 | 1.12 to 3.53 |
| Total Emotional Problems | 1.53 | 1.20 to 1.95 | Pain | 2.60 | 1.53 to 4.42 |
| Total Religious/Spiritual Problems | 0.87 | 0.47 to 1.68 | Fatigue | 1.61 | 0.93 to 2.80 |
| Total Lack of Information Problems | 1.23 | 0.89 to 1.69 | Sleep or insomnia | 1.30 | 0.74 to 2.28 |
| Total Physical Problems | 1.18 | 1.05 to 1.32 | Breathing | 1.37 | 0.77 to 2.43 |
| Total Cognitive Problems | 1.56 | 1.10 to 2.22 |
Final Model χ28 = 92.16, p < .001.
Final Model χ27 = 91.93, p < .001
3.4.4. Predictors of Wanting Help
A total of 75 patients (22.5%) indicated they wanted help with their symptoms. Only the category of emotional problems (OR = 1.36, 95% CI = 1.09 to 1.69) was a significant predictor of wanting help; specific symptoms predictive of wanting help included pain, fatigue, and depression. No other categories of problems or specific symptoms were related to interest in services to help with distress. For patients who did indicate wanting help with their distress, the problems listed most frequently as causing them the most distress were pain, emotional problems, and fatigue.
4. Discussion
More than half of the patients seen in a multidisciplinary outpatient lung cancer clinic reported clinically significant levels of distress. Distress was predicted by problems in the areas of family relationships, emotionalconcerns, information concerns, physical symptoms, and cognitive functioning. Specific symptoms predictive of distress included depression, anxiety, pain, and fatigue. Consistent with previous research, younger patients were more likely to report higher levels of distress along with an interest in obtaining help for distress [14]. Distress levels were not associated with any other clinical variables, including stage of illness or treatment type. The lack of relationship between distress and stage and treatment variables is similar to previous reports [15,16]. Specifically, illness prognosis and illness burden were unrelated to rates of distress in a sample of over 9000 cancer patients [15]. These findings are also consistent with results from a recent study in which clinical variables were unrelated to depression in women treated for early-stage breast cancer [40].
The high rates of distress reported by patients in this sample, many of whom were being seen for the first time or very early in their illness experience, are noteworthy for several reasons. First, patients may experience symptoms of distress beginning with the initial presentation to a lung cancer clinic, results consistent with findings reported by Cooley, Short and Moriarty [41]. Second, in addition to physical symptoms, several other categories of problems (family relationship problems, emotional concerns, information concerns, and cognitive functioning) predict distress. The predictive power of these problem areas highlights the need to assess patients’ functioning beyond the usual practice of monitoring physical symptoms and performance status. The psychosocial nature of these problem categories also signal the importance of including symptom management and palliative care services in early symptom assessment. Third, the distress screening procedures followed in this study were easily implemented. Although not formally documented as a part of the present study, important information about symptoms experienced by patients seen in MLCP was conveyed quickly and efficiently to patients’ physicians and nurses. Clinic staff (CL, PM) and medical oncologists (SA) agreed that the screening improved delivery of patient care by facilitating referrals and calling attention to patient symptoms that may have otherwise gone unaddressed. Thus, although referral procedures and follow-up require further empirical evaluation, inclusion of routine distress screening, involvement of palliative care professionals or other staff dedicated to implementing the brief distress screening form, and treatment of distress symptoms based on a multidisciplinary approach are steps that will likely significantly impact lung patients’ symptom burden. Appropriate identification and treatment of distress and the symptoms contributing to that distress are likely to result in higher quality of life, satisfaction with care, smoking cessation efforts, and better adherence to treatment [29–32,42]. Thus, documenting rates of referral based on distress screening, specific treatment interventions, and quality of life and clinical outcomes following distress screening are important next steps to improve clinical care and evaluate patient outcomes following utilization of distress screening.
In the present study, we responded to calls in the literature to expand the Symptom Problem list that accompanies the DT and to utilize a homogeneous sample of patients rather than a sample of patients with mixed cancer diagnoses [16,35]. Two problem categories predictive of distress, information concerns and cognitive problems, were novel to the problem list used in this study. Because of the predictive utility of information concerns and cognitive problems for level of distress, future distress screening instruments should include assessment of these two areas in addition to the current categories of problems on the NCCN distress thermometer [39].
Compared to other studies using the DT to screen for distress, our sample consisted of large numbers of patients residing in rural areas (56%) and had a sizable number of patients older than age 65 (35%). Our use of an expanded Symptom Problem List and assessment of the desire to help were also novel aspects to the study. Despite these strengths, several limitations should be noted. Although representative of the local geographic area in terms of patient ethnicity, our sample was limited in terms of ethnic diversity. In addition, our sample consisted of consecutive patients and distress screening was conducted as part of routine clinical service, and, as such, we did not collect clinical data on study decliners. Thus, we could not compare decliners to participants in terms of treatment type or stage of disease. Treatment type and stage of disease data for study participants consisted of broad rather than specific categories, and the number of individuals in certain categories (e.g., early stage disease) was small; thus future research should obtained detailed medical records to replicate the lack of relationship between clinical variables and distress found in the present study. Importantly, previous research has not found associations between clinical factors and distress ratings [15,16,40], and thus our results are consistent with these prior reports. Finally, we did not systematically document and follow referral patterns and treatment outcomes for patients referred to the clinical services for treatment of distress. This information would be useful to draw more accurate conclusions about the clinical utility of distress screening. Keller and colleagues recently conducted a study investigating both identification of distressed patients and rates of referral to support services in a sample of patients with mixed cancer diagnoses. Their results suggest that even if distress is recognized by the medical staff, only a small percentage of patients with distress (31%) were actually referred for services [43].
Similar to the rates of referral to services in the study by Keller and colleagues [43], less than one-third of patients (29.3%) with clinically-significant levels of distress in the present sample reported an interest in receiving help for their symptoms. Our results indicate a relationship between distress level and interest in support services; however, previous research did not find such a relationship between distress level and interest in services [44]. Support services may not be palatable for a number of reasons, including stigmatization of needing psychological support [19], lack of knowledge of available support for distress symptoms, or lack of interest in what is perceived as traditional “talk therapy” [17]. Certain characteristics of our sample may have further contributed to the relatively low percentage of individuals who desired help for their symptoms, including significant percentages of older individuals and individuals from rural areas. While age was the only significant factor related to wanting help (with younger patients reporting more interest in wanting help), other factors associated with rurality may be related to not wanting help for distress, including transportation concerns or misunderstanding of what support services may entail [45–46]. Future efforts should be targeted toward clarifying additional barriers to seeking support as well as making services for treating distress as palatable as possible.
Routine screening for distress using brief self-report instruments has been criticized as resulting in elevated rates of distress and potentially inappropriate use of clinical resources [47]. Importantly, however, using empirically established cut-off scores on the DT and following treatment recommendations established by NCCN guidelines for distress management will likely result in appropriate use of clinical resources. Specific areas of concern to the patient, such as uncontrolled pain or nausea, can be assessed, identified, documented, and then addressed through referrals and treatment according to clinical practice guidelines. Although certain symptoms that drive up a patient’s level of distress may remit on their own over time (e.g., state anxiety and/or uncertainty over medical treatment options), documentation of these symptoms is a first step toward encouraging members of the medical team to inquire about these symptoms at future appointments. Physician recommendation of and referral to support services is paramount to patient initiation and uptake of such services, as patients value oncologists’ opinions of these services [48]. In the past, the majority of oncologists did not discuss support or symptom management services with their patients [48], or, if these services were mentioned, many patients did not recall hearing about these services [49]. Oncology professionals may not have received training in communication skills and likely have limited resources and time available [50]. More recently, evidence points to patients taking a more active role in inquiring about support services [51], and thus awareness of the specific symptoms that contribute to levels of distress would allow for more accurate and appropriate referral in response to patient inquiries for services.
The present study highlights the prevalence of clinically-significant distress in patients being seen in a multi-disciplinary lung cancer clinic and suggests that screening for distress should occur at initial patient visits to appropriately identify and refer patients experiencing significant levels of distress. Clinical implications from the present results are clear—1) screening for distress of consecutive patients in a multidisciplinary lung cancer clinic is feasible, 2) distress screening in this setting will identify distressed patients, and 3) a significant number of patients in an outpatient clinic can be expected to meet clinical criteria for distress. Future investigations can investigate the effectiveness of appropriate identification of distress by prospectively assessing patients’ distress and measuring rate of referral, intervention, and psychological and physical outcomes. Moreover, specific strategies can be elucidated for making distress management services palatable to patients, busy oncology health professionals, and cancer clinic administrators.
Acknowledgments
Supported by a Ruth L. Kirschstein National Research Service Award F32CA97760 from the National Cancer Institute (K.D. Graves). We thank Timothy Mullett, MD and Eric Bensadoun, MD, for support of the distress screening process and access to patients. We also thank Susan Revo and Stephen Erena, MS, for assistance with distress screening, and Mike Poynter for assistance with data extraction from the MLCP database.
Footnotes
Conflict of Interest Statement
None declared.
The Problem Symptom List used in the present study was adapted from the Problem List developed by the Distress Management Guidelines Panel of the NCCN [39]. Adaptations included removal of 7 items from the original Problem List and adding 17 items. The seven removed items included: fears, worry, sadness, indigestion, fevers, nose dry/congested, and eating. The 17 additional items included: other family problems, adjusting to my illness, isolation/feeling alone, boredom, facing my mortality, loss of my sense of purpose, lack of information about my diagnosis, lack of information about my treatment, lack of information about alternative therapy choices, lack of information about maintaining fitness, insomnia, swallowing, talking, forgetfulness, seeing/hearing things, feeling confused, and poor thinking.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.National Comprehensive Cancer Network. Distress management clinical practice guidelines. J Natl Comp Cancer Network. 2003;1:344–374. doi: 10.6004/jnccn.2003.0031. [DOI] [PubMed] [Google Scholar]
- 2.Holland J. Psychological care of patients: Psycho-oncology’s contributions. J Clin Oncol. 2003;21:253s–265s. doi: 10.1200/JCO.2003.09.133. [DOI] [PubMed] [Google Scholar]
- 3.Kurtz ME, Kurtz JC, Stommel M, Given CW, Given B. Predictors of depressive symptomatology of geriatric patients with lung cancer-a longitudinal analysis. Psychooncology. 2002;11:12–22. doi: 10.1002/pon.545. [DOI] [PubMed] [Google Scholar]
- 4.McDaniel JS, Musselman DL, Porter MR, Reed DA, Nemeroff CB. Depression in patients with cancer. Diagnosis, biology, and treatment. Arch Gen Psychiatry. 1995;52:89–99. doi: 10.1001/archpsyc.1995.03950140007002. [DOI] [PubMed] [Google Scholar]
- 5.Cella DF, Orofiamma B, Holland JC, Silberfarb PM, Tross S, Feldstein M, Perry M, Maurer LH, Comis R, Oray EJ. The relationship of psychological distress, extent of disease, and performance status in patients with lung cancer. Cancer. 1987;60:1661–1667. doi: 10.1002/1097-0142(19871001)60:7<1661::aid-cncr2820600740>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 6.Cella D. Quality of life considerations in patients with advanced lung cancer. Semin Oncol. 2004;31:16–20. doi: 10.1053/j.seminoncol.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Akizuki N, Akechi T, Nakanishi T, Yoshikawa E, Okamura M, Nakano T, Murakami Y, Uchitomi Y. Development of a brief screening interview for adjustment disorders and major depression in patients with cancer. Cancer. 2003;97:2605–2613. doi: 10.1002/cncr.11358. [DOI] [PubMed] [Google Scholar]
- 8.Helgeson VS, Cohen S. Social support and adjustment to cancer: reconciling descriptive, correlational, and intervention research. Health Psychology. 1996;15:135–148. doi: 10.1037//0278-6133.15.2.135. [DOI] [PubMed] [Google Scholar]
- 9.Carver CS, Pozo-Kaderman C, Harris SD, Noriega V, Scheier MF, Robinson DS, Ketcham AS, Moffat FL, Clark KC. Optimism versus pessimism predicts the quality of women's adjustment to early stage breast cancer. Cancer. 1994;73:1213–1220. doi: 10.1002/1097-0142(19940215)73:4<1213::aid-cncr2820730415>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 10.Boehmke MM, Brown K. Predictors of symptom distress in women with breast cancer during the first chemotherapy cycle. Can Oncol Nurs J. 2005;15:215–227. doi: 10.5737/1181912x154215220. [DOI] [PubMed] [Google Scholar]
- 11.Akechi T, Kugaya A, Okamura H, Nishiwaki Y, Yamawaki S, Uchitomi Y. Predictive factors for psychological distress in ambulatory lung cancer patients. Support Care Cancer. 1998;6:281–286. doi: 10.1007/s005200050167. [DOI] [PubMed] [Google Scholar]
- 12.Stanton AL, Danoff-Burg S, Huggins ME. The first year after breast cancer diagnosis: Hope and coping strategies as predictors of adjustment. Psychooncology. 2002;11:93–102. doi: 10.1002/pon.574. [DOI] [PubMed] [Google Scholar]
- 13.Uchitomi Y, Mikami I, Nagai K, Nishiwake Y, Akechi T, Okamura H. Depression and psychological distress in patients during the year after curative resection of non-small-cell lung cancer. J Clin Oncol. 2003;21:69–77. doi: 10.1200/JCO.2003.12.139. [DOI] [PubMed] [Google Scholar]
- 14.Wenzel LB, Fairclough DL, Brady MJ, Cella D, Garrett KM, Kluhsman BC, Crane LA, Marcus AC. Age-related differences in the quality of life of breast carcinoma patients after treatment. Cancer. 1999;86:1768–1774. [PubMed] [Google Scholar]
- 15.Zabora J, Brintzenhofeszoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 16.Jacobsen PB, Donovan KA, Trask PC, Fleishman SB, Zabora J, Baker F, Holland JC. Screening for psychologic distress in ambulatory cancer patients: A multicenter evaluation of the Distress Thermometer. Cancer. 2005;103:1494–1502. doi: 10.1002/cncr.20940. [DOI] [PubMed] [Google Scholar]
- 17.Carlson LE, Angen M, Cullum J, Goodey E, Koopmans J, Lamont L, MacRae JH, Martin M, Pelletier G, Robinson J, Simpson JS, Speca M, Tillotson L, Bultz BD. High levels of untreated distress and fatigue in cancer patients. Br J Cancer. 2004;90:2297–2304. doi: 10.1038/sj.bjc.6601887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weisman AD, Worden JW. The existential plight in cancer: significance of the first 100 days. Int J Psychiatry Med. 1976;7:1–15. doi: 10.2190/uq2g-ugv1-3ppc-6387. [DOI] [PubMed] [Google Scholar]
- 19.Söllner W, DeVries A, Steixner E, Lukas P, Sprinzl G, Rumpold G, Maislinger S. How successful are oncologists in identifying patient distress, perceived social support, and need for psychosocial counseling? Br J Cancer. 2001;84:179–185. doi: 10.1054/bjoc.2000.1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maguire P. Improving communication with cancer patients. Eur J Cancer. 1999;35:1415–1422. doi: 10.1016/s0959-8049(99)00178-1. [DOI] [PubMed] [Google Scholar]
- 21.Passik SD, Dugan W, McDonald MV, Rosenfeld B, Theobald DE, Edgerton S. Oncologists’ recognition of depression in their patients with cancer. J Clin Oncol. 1998;16:1594–1600. doi: 10.1200/JCO.1998.16.4.1594. [DOI] [PubMed] [Google Scholar]
- 22.McDonald M, Passik SD, Dugan W, Rosenfeld B, Theobald D, Edgerton S. Nurses' recognition of depression in their patients with cancer. Oncol Nurs Forum. 1999;26:593–599. [PubMed] [Google Scholar]
- 23.Grossman SA, Sheidler VR, Swedeen K. Correlation of patient and caregiver ratings of cancer pain. J Pain Symptom Manage. 1991;6:53–57. doi: 10.1016/0885-3924(91)90518-9. [DOI] [PubMed] [Google Scholar]
- 24.Di Maio M, Gridelli C, Gallo C, Manzione L, Brancaccio L, Barbera S, Robbiati SF, Ianniello GP, Ferrau F, Piazza E, Frontini L, Rosetti F, Carrozza F, Bearz A, Spatafora M, Adamo V, Isa L, Iaffaioli RV, Di Salvo E, Perrone F. Prevalence and management of pain in Italian patients with advanced non-small-cell lung cancer. Br J Cancer. 2004;90:2288–2296. doi: 10.1038/sj.bjc.6601810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oi-Ling K, Man-Wah DT, Kam-Hung DN. Symptom distress as rated by advanced cancer patients, caregivers and physicians in the last week of life. Palliat Med. 2005;19:228–233. doi: 10.1191/0269216305pm1001oa. [DOI] [PubMed] [Google Scholar]
- 26.Fisch MJ, Titzer ML, Kristeller JL, Shen J, Loehrer PJ, Jung SH, Passik SD, Einhorn LH. Assessment of quality of life in outpatients with advanced cancer: the accuracy of clinician estimations and the relevance of spiritual well-being—a Hoosier Oncology Group Study. J Clin Oncol. 2003;21:2754–2759. doi: 10.1200/JCO.2003.06.093. [DOI] [PubMed] [Google Scholar]
- 27.Valente SM, Saunders JM, Cohen MZ. Evaluating depression among patients with cancer. Cancer Pract. 1994;2:65–71. [PubMed] [Google Scholar]
- 28.Maguire P. Improving the detection of psychiatric problems in cancer patients. Soc Sci Med. 1985;20:819–823. doi: 10.1016/0277-9536(85)90336-3. [DOI] [PubMed] [Google Scholar]
- 29.Von Essen L, Larsson G, Oberg K, Sjoden PO. ‘Satisfaction with care’: Associations with health-related quality of life and psychosocial function among Swedish patients with endocrine gastrointestinal tumors. Eur J Cancer Care. 2002;11:91–99. doi: 10.1046/j.1365-2354.2002.00293.x. [DOI] [PubMed] [Google Scholar]
- 30.Kennard BD, Stewart SM, Olvera R, Bawdon RE, Hailin AO, Lewis CP, Winick NJ. Nonadherence in adolescent oncology patients: preliminary data on psychological risk factors and relationships to outcome. J Clin Psych Medical Settings. 2004;11:31–39. [Google Scholar]
- 31.Kukull WA, McCorkle R, Driever M. Symptom distress, psychosocial variables and lung cancer survival. J Psychosoc Oncol. 1986;4:91–104. [Google Scholar]
- 32.Kaasa S, Mastekaasa A, Lund E. Prognostic factors for patients with inoperable non-small cell lung cancer, limited disease. The importance of patients’ subjective experience of disease and psychosocial well being. Radiother Oncol. 1989;15:235–242. doi: 10.1016/0167-8140(89)90091-1. [DOI] [PubMed] [Google Scholar]
- 33.Roth AJ, Kornblith AB, Batel-Copel L, Peabody E, Scher HI, Holland JC. Rapid screening for psychologic distress in men with prostate carcinoma: A pilot study. Cancer. 1998;82:1904–1908. doi: 10.1002/(sici)1097-0142(19980515)82:10<1904::aid-cncr13>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 34.Trask PC, Paterson A, Riba M, Brines B, Griffith K, Parker P, Weick J, Steele P, Kyro K, Ferrara J. Assessment of psychological distress in prospective bone marrow transplant patients. Bone Marrow Transplant. 2002;29:917–925. doi: 10.1038/sj.bmt.1703557. [DOI] [PubMed] [Google Scholar]
- 35.Hoffman BM, Zevon MA, D’Arrigo MC, Cecchini TB. Screening for distress in cancer patients: The NCCN rapid-screening measure. Psychooncology. 2004;13:792–799. doi: 10.1002/pon.796. [DOI] [PubMed] [Google Scholar]
- 36.American Cancer Society. [accessed June 21, 2005];Cancer Facts and Figures. 2005 Available from URL: http://www.cancer.org.
- 37.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 38.Economic Research Service US Department of Agriculture. [accessed June 21, 2005];Measuring rurality: Rural-urban continuum codes. Available from URL: http://www.ers.usda.gov/Briefing/Rurality/RuralUrbCon/
- 39.National Comprehensive Cancer Network. Distress Treatment Guidelines Management Version 1.2004. [accessed Nov 16, 2004];Clinical Practice Guidelines in Oncology. Available from URL: http://www.nccn.org/professionals/physician_gls/PDF/distress.pdf.
- 40.Bardwell WA, Natarajan L, Dimsdale JE, Rock CL, Mortimer JE, Hollenbach K, Peirce JP. Objective cancer-related variables are not associated with depressive symptoms in women treated for early-stage breast cancer. J Clin Onc. 2006;24:2420–2427. doi: 10.1200/JCO.2005.02.0081. [DOI] [PubMed] [Google Scholar]
- 41.Cooley M, Short T, Moriarty H. Patterns of symptom distress in adults receiving treatment for lung cancer. J Palliat Care. 2002;18:150–159. [PubMed] [Google Scholar]
- 42.Schnoll RA, Miller SM, Unger M, McAleer C, Halbherr T, Bradley P. Characteristics of female smokers attending a lung cancer screening program: a pilot study with implications for program development. Lung Cancer. 2002;37:257–65. doi: 10.1016/s0169-5002(02)00106-x. [DOI] [PubMed] [Google Scholar]
- 43.Keller M, Sommerfeldt S, Fischer C, Knight L, Riesbeck M, Löwe B, Herfarth C, Lehnert T. Recognition of distress and psychiatric morbidity in cnacer patients: A multi-method approach. Ann Oncol. 2004;15:1243–1249. doi: 10.1093/annonc/mdh318. [DOI] [PubMed] [Google Scholar]
- 44.Söllner W, Maislinger S, Konig A, Devries A, Lukas P. Providing psychosocial support for breast cancer patients based on screening for distress within a consultation-liaison service. Psychooncology. 2004;13:893–897. doi: 10.1002/pon.867. [DOI] [PubMed] [Google Scholar]
- 45.Angell KL, Kreshka MA, McCoy R, Donnelly P, Turner-Cobb JM, Graddy K, Kraemer HC, Koopman C. Psychosocial intervention for rural women with breast cancer: The Sierra-Stanford Partnership. J Gen Intern Med. 2003;18:499–507. doi: 10.1046/j.1525-1497.2003.20316.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Davis C, Williams P, Redman S, White K, King E. Assessing the practical and psychosocial needs of rural women with early breast cancer in Australia. Soc Work Health Care. 2003;36:25–36. doi: 10.1300/j010v36n03_02. [DOI] [PubMed] [Google Scholar]
- 47.Coyne J, Palmer S, Shapiro P, Thompson R, DeMichele A. Distress, psychiatric morbidity, and prescriptions for psychotropic medication in a breast cancer waiting room sample. Gen Hosp Psychiatry. 2004;26:121–128. doi: 10.1016/j.genhosppsych.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 48.Edgar L, Remmer J, Rosberger Z, Fournier M. Resource use in women completing treatment for breast cancer. Psychooncology. 2000;9:428–438. doi: 10.1002/1099-1611(200009/10)9:5<428::aid-pon481>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 49.Eakin EG, Strycker LA. Awareness and barriers to use of cancer support and information resources by HMO patients with breast, prostate, or colon cancer: Patient and provider perspectives. Psychooncology. 2001;10:103–113. doi: 10.1002/pon.500. [DOI] [PubMed] [Google Scholar]
- 50.Fallowfield L, Ratcliffe D, Jenkins V, Saul J. Psychiatric morbidity and its recognition by doctors in patients with cancer. Br J Cancer. 2001;84:1011–1015. doi: 10.1054/bjoc.2001.1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Matthews BA, Baker F, Spillers RL. Oncology professionals and patient requests for cancer support services. Support Care Cancer. 2004;12:731–738. doi: 10.1007/s00520-004-0647-9. [DOI] [PubMed] [Google Scholar]


