Abstract
This study examined the construct validity of Narcissistic Personality Disorder (NPD) by examining the relations between NPD and measures of psychological distress and functional impairment both concurrently and prospectively across two samples. In particular, the goal was to address whether NPD typically “meets” Criterion C of the DSM-IV definition of Personality Disorder, which requires that the symptoms lead to clinically significant distress or impairment in functioning. Sample 1 (N =152) was composed of individuals receiving psychiatric treatment, while Sample 2 (N=151) was composed of both psychiatric patients (46%) and individuals from the community. NPD was linked to ratings of depression, anxiety, and several measures of impairment both concurrently and at 6-month follow-up. However, the relations between NPD and psychological distress were (a) small, especially in concurrent measurements, and (b) largely mediated by impaired functioning. NPD was most strongly related to causing pain and suffering to others, and this relationship was significant even when other Cluster B personality disorders were controlled. These findings suggest that NPD is a maladaptive personality style which primarily causes dysfunction and distress in interpersonal domains. The behavior of narcissistic individuals ultimately leads to problems and distress for the narcissistic individuals and for those with whom they interact.
Narcissistic Personality Disorder: Relations with distress and functional impairment
Narcissistic personality disorder (NPD), despite substantial interest from a theoretical perspective, has received very little empirical attention (1). In fact, some have concluded that “most of the literature regarding patients suffering with narcissistic personality disorder is based on clinical experience and theoretical formulations, rather than empirical evidence” (2; p. 303). A large majority of empirical studies on narcissism come from a social-personality psychology perspective which, while methodologically sophisticated and important, may not pertain to Narcissistic PD given the reliance on undergraduate samples and the use of the Narcissistic Personality Inventory (NPI, 3). Trull and McCrae (4) have noted that narcissism measured by the NPI appears to be made up of high Extraversion, low Agreeableness, and low Neuroticism from the Five-Factor Model of personality (5), while DSM definitions suggest low Agreeableness, high Neuroticism and no relation with Extraversion. These authors suggest that “most narcissistic scales do not square well with DSM-III-R criteria for NAR” (4; p.53). The field must be cautious about relying on these studies to inform our knowledge of NPD. The few empirical studies of NPD that have used clinical samples and DSM based measures have focused on the underlying factor structure and item content (6–8). In particular, there is a striking lack of data regarding the impairment and distress associated with NPD. Central to the issue of validity for any DSM disorder is whether it is actually associated with distress or impairment – in fact criterion C for PD from the DSM-IV (9, p. 689) mandates that one of the two be present in order to make a PD diagnosis. While there is good evidence for the functional impairment of PDs in general (10–11), and certain specific PDs such as borderline (12), schizotypal and avoidant (13), it is still quite unclear whether NPD predicts psychological distress and problems in various life domains.
As noted, the association between NPD and psychological distress is particularly unclear. The DSM-IV suggests that these individuals have a “very fragile” self-esteem (p. 714), are “very sensitive to injury from criticism or defeat” (p. 715), and that “sustained feelings of shame or humiliation…may be associated with social withdrawal” and “depressed mood” (p. 716). However, given the derivation of the DSM over time, these statements appear to be the result of expert opinion rather than empirical findings. Results from clinical samples are both sparse and contradictory. In fact, a meta-analysis of the relations between the FFM and DSM PDs found an effect size (i.e., r) of only .03 between Narcissism and Neuroticism, which measures emotional stability and the tendency to experience negative affective states such as depression, anxiety, and shame (14). However, this hides the substantial variability of the findings; of the 18 included effects, 5 were significantly positive, 7 were significantly negative, and 6 were nonsignificant. Within clinical samples, the effect size was .14 suggesting a small but significant relation to Neuroticism. There has also been some speculation that narcissism may be linked to higher rates of suicide (2), although the data are quite limited.
Alternatively, Watson, Sawrie, Greene, and Arredondo (15) found significant negative relations between measures of narcissism (derived from the Minnesota Multiphasic Personality Inventory-2; 16) and depression in two clinical samples. Studies on comorbidity between PDs and Axis I disorders have not found a relation between NPD and depression or anxiety-related disorders (17–20). Furthermore, findings from the large non-psychiatric literature on narcissism conducted from a social-personality perspective suggest a negative relation between narcissism and psychological distress. Research using the Narcissism Personality Inventory has suggested that narcissistic individuals are psychologically resilient, relatively immune to psychopathology, and manifest primarily interpersonal impairment (21–22). Indeed, a reading of the social personality might lead one to conclude that narcissism, as a result of being composed of high positive and low negative affect and high self-esteem, is an adaptive trait (23).
Where the clinical lore and social-personality data do converge is on the interpersonal impairment linked with narcissism. The DSM-IV postulates that “interpersonal relations are typically impaired due to problems derived from entitlement, the need for admiration, and the relative disregard for the sensitivities of others” (p.716). Empirical studies of narcissism in the social-personality literature find that it predicts a self-centered, selfish and exploitative approach to interpersonal relationships, including game-playing, infidelity, a lack of empathy, and even violence (24–25). The negative consequences of narcissism are felt especially strongly by those who are involved with the narcissist (26). How quickly this personality style manifests this interpersonal impairment is up for debate. There is some evidence that the interpersonal difficulties associated with narcissism are only apparent over time, with narcissism being associated with apparently positive interpersonal functioning during initial relationship stages (27–28). However, other studies have found that individuals with unrealistically high positive self-evaluations are rated negatively by independent raters following a very brief competitive interaction with a peer (29). Unfortunately, there are very few data on NPD and interpersonal impairment using clinical samples. There are data from therapeutic relationships where items from a measure of countertransference were rated by a sample of psychiatrists and psychologists for patients with NPD. The authors of this study found that “clinicians reported feeling anger, resentment, and dread in working with narcissistic personality disorder patients; feeling devalued and criticized by the patient; and finding themselves distracted, avoidant, and wishing to terminate the treatment” (30, p. 894). These findings provide strong support for the interpersonal impairment these individuals experience as even trained clinicians experience strong negative feelings about these types of clients.
Given the relatively stronger evidence of a link between NPD and interpersonal impairment than between NPD and psychological distress, it is plausible that NPD, at times, leads to clinically significant depression and/or anxiety but these negative affective states are probably secondary to the interpersonal impairment. That is, NPD may lead individuals to experience failure in a number of important domains (e.g., romance) that might lead to psychological distress; however, this distress may not be endemic to NPD. This may differ from other PDs such as borderline in which negative affectivity appears to be an intrinsic part of the disorder.
The goals of the current study are to: 1. Assess the association between NPD and psychological distress including depression and anxiety. 2. Assess the association between NPD and impairment, including indices of romantic, social, occupational, and general impairment, as well as the spillover effects of NPD on significant others. 3. Assess the predictive power of NPD in relation to psychological distress and impairment over a 6-month period. 4. Test a model in which any positive link between narcissism and psychological distress is accounted for by impairment. 5. Assess the unique predictive power of NPD in predicting psychopathology and impairment, when controlling for the other Cluster B personality disorders.
Method
Participants and Procedures
Sample 1
Participants (n = 152) were solicited from inpatient and outpatient programs at Western Psychiatric Institute and Clinic (WPIC) in Pittsburgh, PA. Patients with psychotic disorders, organic mental disorders, and mental retardation were excluded, as were patients with major medical illnesses that influence the central nervous system and might be associated with organic personality disturbance. Participants (in both samples) provided written informed consent after all study procedures had been explained. See Table 1 for current Axis I diagnostic information.
Table 1.
| Sample 1 | Sample 2 | |||
|---|---|---|---|---|
| Axis I Diagnoses - Current | n | % | n | % |
| Affective disorders only | 54 | 35.5 | 31 | 20.5 |
| Anxiety disorders only | 13 | 8.6 | 12 | 7.9 |
| Substance abuse disorders only | 6 | 3.9 | 7 | 4.6 |
| Comorbid affective and anxiety disorders | 31 | 20.4 | 19 | 12.6 |
| Comorbid affective and substance abuse disorders | 11 | 7.2 | 7 | 4.6 |
| Comorbid anxiety and substance abuse disorders | 3 | 2.0 | 1 | 0.7 |
| Comorbid affective, anxiety, and substance abuse disorders | 7 | 4.6 | 2 | 1.3 |
| Other diagnoses (e.g., eating disorders, somatoform do.) | 14 | 9.2 | 17 | 11.3 |
| None (V-codes or past diagnoses only) | 13 | 8.6 | 55 | 36.4 |
Note. Total n = 152 (sample 1) patients who received a “best estimate” consensus diagnosis at intake. Total n = 151 (sample 2) who received a “best estimate” consensus diagnosis at intake.
Of the 152 individuals, 85 were women (56%), 135 were Caucasians (89%), 16 were African Americans (11%), and 1 was Asian American (1%), 121 were outpatients (80%), and the mean age was 34.5 years (SD = 9.4). Of the original sample, 105 (69%) were also assessed at a 6-month follow up. Attrition analyses were conducted on the following 16 variables: age, sex, race, treatment condition, marital status, education, and symptom counts for the 10 DSM III-R PDs that remain in the DSM-IV. No significant differences were found.
Sample 2
This sample (n = 151) was comprised of 70 psychiatric patients and 81 non-psychiatric participants. The non-psychiatric patients were recruited from two sources: diabetic patients (n = 23) or university faculty or staff (n = 58). This sample was part of a larger sample (n = 624) that was first screened for PDs. The larger sample was stratified on the basis of initial scores and individuals were randomly selected to participate in the interview portion of the study. The goal was to create a sample that had a 50% prevalence rate for PD. The psychiatric patients were solicited from an adult outpatient clinic at WPIC. The rule-outs used in Sample 1 were also utilized in this study. See Table 1 for Axis I information.
Of the 151 individuals, 103 women (68%) were women, 131 were Caucasians (86.8%), 16 were African Americans (10.6%), 4 were Asian Americans (2.6%), and the mean age was 38.85 years (range = 20 to 60, SD = 11.18). Of the original sample, 126 (83%) were assessed at a 6-month follow up. Attrition analyses were conducted on the following 16 variables: age, sex, race, treatment condition, marital status, education, and symptom counts for the 10 DSM-IV PDs. No significant differences were found.
Measures
Consensus ratings of DSM-III-R (Sample 1) and DSM-IV (Sample 2) personality disorder criteria
Complete details of the assessment methodology are provided elsewhere (11, 31). At intake, participants were interviewed for 6–10 hours in a minimum of 3 assessment sessions. The assessments sessions included structured symptom ratings, structured interviews for Axis I and Axis II disorders (e.g., the SCID, the PDE, SIDP-III-R, or SIDP-IV) and a detailed social and developmental history. Patients also completed self-report questionnaires between interviews. Following the evaluation, the primary interviewer presented the case at a two-hour diagnostic conference with colleagues from the research team. All available data (historical and concurrent) were reviewed and discussed at the conference: current and lifetime Axis I information, symptomatic status, social and developmental history, and personality features acknowledged on the Axis II interviews. In addition, significant others (e.g., romantic partners, family members, friends) were interviewed (when available) about patients’ characteristic personality features. Each PD symptom was rated on a scale of 0 to 2. The symptom counts used are the addition of these scores across symptoms for each PD. In Sample 1, we altered the NPD count by deleting one DSM-III-R symptom (i.e., reacts to criticism with feelings of rage, shame, or humiliation) in order to approximate the current DSM-IV conceptualization of NPD.
PDQ-4+ (Sample 2)
The PDQ-4+ (32) is 99-item self-report measure of DSM-IV PDs and was used in Sample 2. The mean NPD symptom count was 1.98 (SD =1.61).
Consensus ratings of impairment (Sample 1 and 2)
Consensus ratings of functional impairment were made separately for romantic relationships, other social relationships (e.g., friends, family members), occupational impairment, distressed caused to significant others (e.g., romantic partners, parents, children, close friends), and an overall impairment. The ratings ranged from 1 to 5 with higher scores indicating greater impairment (e.g., unable to work, no friends, no history of romantic relationships or history of chaotic relationships). As with PD ratings, all ratings were made using the LEAD model. As such, all information gleaned from the extensive interviews with participants and significant others (when available) pertaining to Axis I and II symptomatology, as well as past and present social, romantic, and educational/occupational histories was used to determine consensus ratings of impairment.
Clinical ratings of depression, anxiety, and functioning (Sample 1 and 2)
Ratings of psychological distress were conducted with the Hamilton Rating Scale for Depression (HAM-D) and the Hamilton Rating Scale for Anxiety (HAM-A). Functioning was assessed via the Global Assessment of Functioning (GAF). For both samples, intraclass correlation coefficients (ICCs), computed with all available reliability data, documented good to excellent levels of reliability within our own group of judges. The ICCs for the HAM-D were .96 (Sample 1) and .98 (Sample 2. The ICCs for the HAM-A were .97 (Sample 1) and .94 (Sample 2). The ICCs for the GAF were .75 (Sample 1) and .80 (Sample 2).
Six-month follow-up
The assessment procedures completed at intake were used again at the 6-month follow-up, with the exception of the social/developmental history, which is not repeated. As with intake, all sources of available data were used to inform consensus ratings (i.e., ratings of impairment; GAF) via the LEAD model. The 6-month ratings of depression and anxiety (e.g., HAM-D; HAM-A) were again based on the clinical interviewer’s ratings, not consensus.
Statistical Analyses
First, Pearson’s rs were used to examine the relations between narcissism and measures of anxiety, depression and various forms of functional impairment both concurrently and longitudinally. Next, we examined a model in which the prospective relations between narcissism and measures of psychopathology are mediated by impairment. Finally, we used hierarchical linear regression analyses to examine the unique predictive relations between Narcissism at Time 1 and distress and impairment measured at 6-month follow-up, after controlling for the effects of the other Cluster B PDs. Two-tailed p values were computed in all analyses. The distributions of all variables were examined and none showed signs of a significant departure from normality using existing guidelines (33; skewness ≥2.0 and/or kurtosis ≥ 7.0). As such, Pearson rs are used.
Results
Capturing narcissism: Concurrent and longitudinal relations
Sex differences
There were significant sex differences for narcissism in Sample 1, t(150) =4.14, p≤.001, and Sample 2, t(149) =1.98, p≤.05, such that men had higher NPD symptom counts. All correlations presented in Table 2 were tested separately for men and women; no significant differences were found.
Table 2.
Characterizing Narcissistic PD: Relations with Axis I psychopathology and impairment.
| M | SD | NPD Symptoms-Sample 1 | M | SD | NPD symptoms-Sample 2 | wr | |
|---|---|---|---|---|---|---|---|
| Distress/Psychopathology (concurrent) | |||||||
| Depression (HAM-D) | 14.4 | 7.9 | .05 | 10.93 | 7.5 | .18* | .12* |
| Anxiety (HAM-A) | 15.0 | 8.8 | −.01 | 11.85 | 8.2 | .24** | .11* |
| Distress/Psychopathology (longitudinal) | |||||||
| Depression (HAM-D) | 7.86 | 6.6 | .15 | 8.33 | 7.1 | .26** | .21** |
| Anxiety (HAM-A) | 8.55 | 7.5 | .20* | 9.08 | 7.4 | .25** | .23** |
| Impairment (concurrent) | |||||||
| GAF scores | 54.6 | 7.2 | −.12 | 61.73 | 11.5 | −.26** | −.19** |
| Overall Impairment | 3.22 | .67 | .44** | 2.71 | .83 | .34** | .39** |
| Social | 2.85 | .88 | .37** | 2.77 | .88 | .16* | .27** |
| Romantic | 3.70 | .72 | .22** | 3.14 | .91 | .23** | .22** |
| Work | 2.86 | .94 | .36** | 2.36 | .98 | .27** | .32** |
| Distress-in a significant other | 3.01 | .67 | .42** | 2.38 | .89 | .50** | .46** |
| Impairment (6 months) | |||||||
| GAF scores | 62.20 | 8.5 | −.20* | 62.00 | 11.51 | −.30** | −.26** |
| Overall Impairment | 3.24 | .71 | .43** | 2.81 | .85 | .35** | .39** |
| Social | 2.91 | .87 | .33** | 2.85 | .90 | .17* | .24** |
| Romantic | 3.63 | .84 | .27** | 3.21 | .88 | .24** | .25** |
| Work | 2.96 | .95 | .24* | 2.48 | .99 | .31** | .28** |
| Distress-in a significant other | 3.03 | .80 | .42** | 2.51 | .94 | .52** | .48** |
p≤.05,
p≤.01; wr = weighted mean effect size
Relations with psychological distress and impairment: Concurrent and longitudinal findings
Concurrently, narcissism was related to ratings of depression and anxiety only in Sample 2 (see Table 2). Longitudinally, narcissism was related to Time 2 depression in Sample 2 and anxiety in both samples. The weighted effects sizes (taking into account the correlations from both samples and weighting them on the basis of sample sizes) were small in all cases.
The pattern of findings between narcissism and impairment was quite consistent across assessments and samples. NPD symptoms were related to lower GAF scores in three of four instances. In addition, NPD symptoms were related to overall impairment, as well as all specific indices of impairment including impairment in romance, work, social life, and causing distress to significant others. Of the specific impairment scores, “distress to significant others” demonstrated the largest weighted effect sizes (rs =.46 and .48).
Impairment as a mediator of the relationship between narcissism and psychological distress
We next examined the hypothesis that narcissism may be related to psychological distress primarily due to the impairment it causes in various life domains (see Figure 1). To examine this, we conducted a series of regression analyses. First, we regressed Time 2 distress (e.g., depression, anxiety, GAF) on Time 1 narcissism. Next, we regressed the mediator (Time 2 overall impairment) on Time 1 narcissism. Finally, we regressed Time 2 distress variables on Time 2 impairment and Time 1 narcissism. These path analyses test whether functional impairment mediates the relations between narcissism and later distress. Additionally, Sobel tests (which yield a z-score) were used to test for statistical mediation. In Sample 1, there was significant mediation by impairment for the relation between NPD and Time 2 depression (z = 2.81, p≤.01) and Time 2 GAF scores (z = 4.14, p≤.01). In addition, there was a trend toward significant mediation (z = 1.81, p≤.07) for the relation between NPD and Time 2 anxiety. In Sample 2, the relations between NPD symptoms and depression, anxiety, and GAF scores were all significantly mediated (zs = 3.31, 3.26, and 3.59, p≤.001, respectively) by the impairment rating. Across these mediation models, the direct effect of narcissism on psychopathology decreased significantly after impairment was included in the model; in all six cases, narcissism was no longer significantly related to the distress outcome once impairment was included. In fact, the direct effect of narcissism was reduced by between 40% (anxiety, Sample 1) to 100% (depression, Sample 1; GAF, Sample 1; depression, Sample 2)
Figure 1.
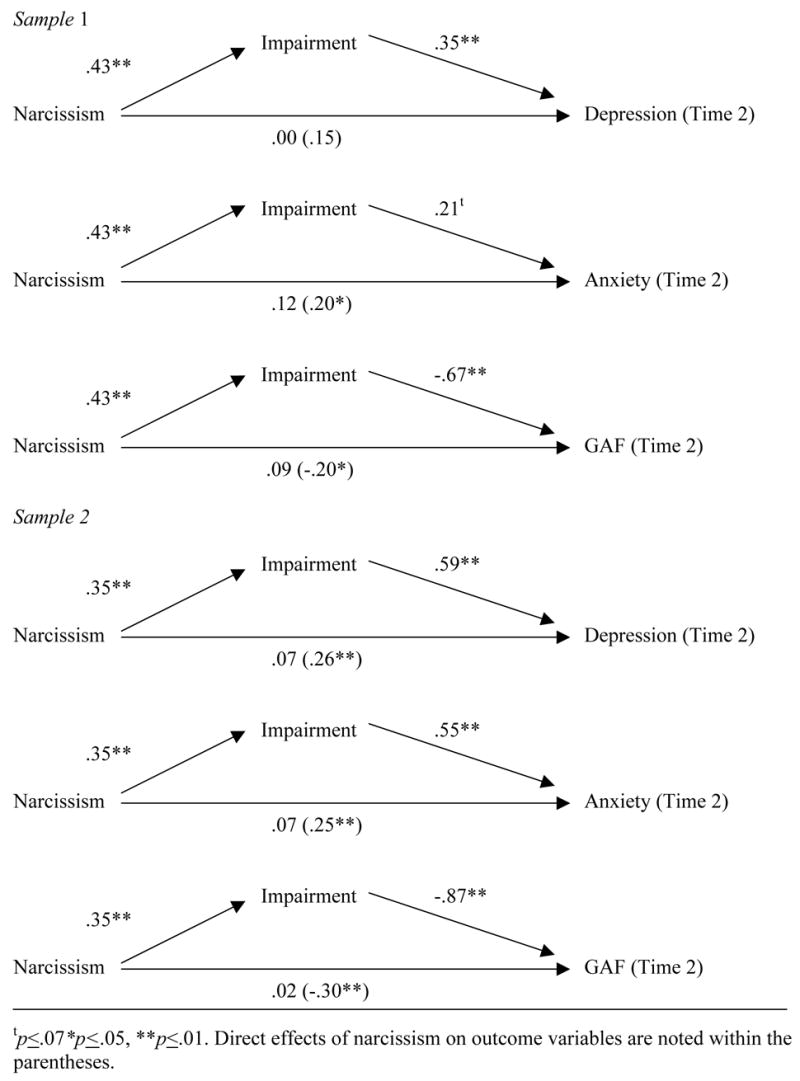
Mediation of the relation between NPD and psychological distress
Replicating mediation analyses with self-reported PDQ narcissism scores
In order to reduce concern that the previous results might be due, in part, to common method variance (i.e., consensus rating of both predictor and outcome variables), we replicated the same aforementioned model in Sample 2 but used self-reported symptoms of narcissism (i.e., PDQ) in place of consensus ratings of NPD. The results were nearly identical. Again, Sobel tests were used to test for statistical mediation. There was significant mediation by impairment for the relations between PDQ NPD and Time 2 depression (z = 2.78, p≤.01), Time 2 anxiety (z = 2.70, p≤.01), and Time 2 GAF scores (z = 2.93, p≤.01). The direct effect of narcissism was reduced by between 45% (anxiety) to 70% (GAF).
Narcissism: Unique predictive relations of 6-month outcomes controlling for Cluster B PDs
Finally, we examined whether narcissism was a unique predictor of psychopathology and impairment once we controlled for the symptoms of antisocial, borderline and histrionic PDs (see Table 3). This is an extremely conservative test because it requires narcissism to predict above and beyond PDs that are significantly related to NPD (across both current samples, NPD was significantly related antisocial, borderline and histrionic PDs; mdn r =.40) and that might be associated with more serious psychopathology. We conducted a series of regression analyses in which sex, antisocial, borderline, and histrionic PD symptom counts were entered at step 1, followed by NPD symptoms at step 2. As can be seen in Table 3, narcissism was not a unique significant predictor of depression or anxiety at 6-month follow-up, although there was a trend for narcissism predicting anxiety in Sample 1. Importantly, of the impairment indices tested, narcissism was a consistent significant unique predictor for only one form of impairment - causing distress to significant others. This pattern was found in both samples. There was also a trend for narcissism predicting romantic impairment in Sample 1.
Table 3.
Unique predictive relations across 6 months: narcissism and psychopathology
| Depression | Anxiety | GAF | Social | Romantic | Work | Distress to Others | |
| Sample 1 | β | β | β | β | β | β | β |
| Step 1 | |||||||
| Sex | .07 | .08 | .08 | −.27** | −.04 | −.18* | .01 |
| Antisocial | −.16 | −.06 | −.02 | .03 | −.03 | .12 | .10 |
| Borderline | .36** | .17 | −.42** | .50** | .48** | .45** | .44** |
| Histrionic | .02 | .09 | .09 | −.14 | −.08 | −.11 | .16 |
| R2 | .12* | .06 | .16** | .30** | .19** | .26** | .35** |
| Step 2 | |||||||
| Narcissism | .13 | .27 t | −.09 | .19 | .24t | .04 | .26* |
| ΔR2 | .00 | .04t | .00 | .02 | .03t | .00 | .03* |
| Depression | Anxiety | GAF | Social | Romantic | Work | Distress to Others | |
| Sample 2 | β | β | β | β | β | β | β |
| Step 1 | |||||||
| Sex | −.06 | .02 | .00 | −.02 | −.11 | −.12 | −.02 |
| Antisocial | −.05 | .05 | −.08 | .08 | −.01 | .29** | .15 |
| Borderline | .52** | .39** | −.52** | .35** | .43** | .40** | .41** |
| Histrionic | .14 | .22** | −.12 | .02 | .19* | .08 | .33** |
| R2 | .31** | .30** | .39** | .16** | .28** | .42** | .51** |
| Step 2 | |||||||
| Narcissism | .05 | .02 | −.04 | .03 | −.04 | .02 | .23** |
| ΔR2 | .00 | .00 | .00 | .00 | .00 | .00 | .03** |
p≤.10
p≤.05,
p≤.01
Discussion
Despite its placement in the last three editions of the DSM as one of only 10 officially recognized personality disorders, narcissistic PD has received scant empirical attention. Specifically, there has been little data presented that makes a clear and persuasive argument for its inclusion on the basis of the distress and impairment NPD causes. One strategy for dealing with this dearth of data on NPD would be to turn to the substantial empirical literature on narcissism that exists in the fields of social-personality psychology. However, this is problematic due to the use measures (e.g., NPI) that appear to capture only partially the construct as it is currently conceptualized by the DSM-IV and the reliance on undergraduate samples. Even if one were to rely on this body of literature, the central question would remain unresolved as to whether narcissistic individuals experience psychological distress (this literature suggests they do not; 21) or substantial impairment (24, 26). The current study addresses these issues by presenting data on the concurrent and longitudinal relations between narcissistic PD and psychological distress and functional impairment in two clinical samples. These constructs are of vital importance in determining whether narcissism warrants continued presence in our diagnostic nomenclature.
The current results suggest that NPD symptoms are significantly, but modestly, related to depression and anxiety both concurrently (Sample 2 only) and prospectively. NPD was also significantly and more strongly related to two general measures of impairment and more specific indices of impaired functioning in work, social, and romantic domains. These findings were consistent across samples and assessments (i.e., Times 1 and 2) and are consistent with findings regarding the broad array of impairment attached to other specific PDs (12–13). The GAF scores demonstrated the weakest relations, albeit still significant in 3 of 4 analyses. Across assessments, the weighted effect sizes were largest for impairment related to causing distress for important significant others. Indeed, NPD was only uniquely related to causing significant others pain and duress. This finding is consistent with knowledge gathered about the impact of narcissism in non-clinical samples, where narcissism is associated largely with costs suffered by others (24, 26).
We found evidence in both samples for a model in which the relation between narcissism and psychological distress was mediated by impaired functioning. That is, overall impairment accounted for the relationship between Time 1 narcissism and lower GAF scores, higher depression and anxiety at Time 2. These findings support the notion that depression and anxiety may not be endemic to narcissism but develop as a result of problems or failures in a variety of contexts. Narcissistic individuals may eventually feel sad or worried as they gain insight into the fact that they are not as successful in their work, love, and friendship relations as they hoped or in comparison to their peers. This finding might also partially explain the differences in the relationship between narcissism and psychological distress as reported in the clinical and social-personality literatures. Most narcissists would enter a clinical setting as a result of some form of failure in their personal or professional life, and this failure would eventually be expected to lead to psychological distress. Individuals with narcissistic personality traits who are able to avoid personal or professional failure, however, may both avoid clinical settings and report low levels of psychological distress.
Limitations
One potential limitation of the current study is that the samples were somewhat different; the results from Sample 1 used a slight variation of the DSM-III-R criteria rather than the DSM-IV, while Sample 2 was a hybrid in that it included clinical patients and individuals from the community. These differences should have worked to make replication less likely, which was not the case. Another limitation is that the expert raters for the consensus ratings of impairment also generated the PD ratings and it is possible that raters’ preconceived notions regarding the types of impairment attached to certain PDs could impact later impairment ratings. The likelihood that this impacted the current finding is diminished by the presentation of an ancillary analysis using the data from Sample 2 in which the findings were nearly identical when different sources of ratings were used (i.e., self-reports of narcissistic PD).
Conclusions
These results suggest that it is accurate to think of NPD as a pathological personality style that predicts impaired functioning across a variety of life domains. This impaired functioning appears largely to explain NPD’s weak but significant relation with intrapersonal distress. Importantly, the strongest impairment associated with NPD is the distress or “pain and suffering” experienced not by the narcissist but by his or her significant others. In fact, the suffering experienced by others is uniquely predicted by NPD when controlling for other PDs. It appears that there are traits specific to NPD that are especially difficult to tolerate when faced regularly.
Acknowledgments
This research was supported by NIMH grants R01 MH44672, Validity in the Diagnosis of Personality Disorders (PI: P. A. Pilkonis), and R01 MH56888, Screening for Personality Disorders (PI: P. A. Pilkonis).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Paris J. Personality disorders over time: Precursors, course and outcome. J Personal Disord. 2003;17:479–488. doi: 10.1521/pedi.17.6.479.25360. [DOI] [PubMed] [Google Scholar]
- 2.Links PS, Gould B, Ratnayake R. Assessing suicidal youth with antisocial, borderline, or narcissistic personality disorder. Can J Psychiatry. 2003;48:301–310. doi: 10.1177/070674370304800505. [DOI] [PubMed] [Google Scholar]
- 3.Raskin RN, Terry H. A principle components analysis of the Narcissistic Personality Inventory and further evidence of its construct validity. J Pers Soc Psychol. 1988;54:890–902. doi: 10.1037//0022-3514.54.5.890. [DOI] [PubMed] [Google Scholar]
- 4.Trull TJ, McCrae RR. A five-factor perspective on personality disorder research. In: Costa PT, Widiger TA, editors. Personality disorders and the five-factor model of personality. Washington, DC: American Psychological Association; 2002. pp. 45–58. [Google Scholar]
- 5.Costa PT, McCrae RR. The NEO Personality Inventory manual. Odessa, FL: Psychological Assessment Resources; 1985. [Google Scholar]
- 6.Blais MA, Hilsenroth MJ, Castlebury FD. Content validity of the DSM-IV borderline and narcissistic personality disorder criteria sets. Compr Psychiatry. 1997;38:31–37. doi: 10.1016/s0010-440x(97)90050-x. [DOI] [PubMed] [Google Scholar]
- 7.Fossati A, Beauchaine TP, Grazioli F, Carretta I, Cortinovis F, Maffei C. A latent structure analysis of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Narcissistic Personality Disorder criteria. Compr Psychiatry. 2005;46:361–367. doi: 10.1016/j.comppsych.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 8.Holdwick DJ, Hilsenroth MJ, Castlebury FD, Blais MA. Identifying the unique and common characteristics among the DSM-IV antisocial, borderline and narcissistic personality disorders. Compr Psychiatry. 1998;39:277–286. doi: 10.1016/s0010-440x(98)90036-0. [DOI] [PubMed] [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and Statistical Manual. 4. Washington, DC: 2000. Text Revision. [Google Scholar]
- 10.Drake RE, Vaillant GE. A validity study of Axis II of DSM-III. Am J Psychiatry. 1985;142:553–558. doi: 10.1176/ajp.142.5.553. [DOI] [PubMed] [Google Scholar]
- 11.Pilkonis PA, Heape CL, Ruddy J, Serrao PS. Validity in the diagnosis of personality disorders: The use of the LEAD standard. Psychol Assess. 1991;3:46–54. [Google Scholar]
- 12.Zanarini MC, Frankenburg FR, Hennen J, Reich B, Silk KR. Psychosocial functioning of borderline patients and Axis II comparison subjects followed prospectively for six years. J Personal Disord. 2005;19:19–29. doi: 10.1521/pedi.19.1.19.62178. [DOI] [PubMed] [Google Scholar]
- 13.Skodol AE, Gunderson JG, McGlashan TH, Dyck IR, Stout RL, Bender DS, Grilo CM, Shea MT, Zanarini MC, Morey LC, Sanislow CA, Oldham JM. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry. 2002;159:276–283. doi: 10.1176/appi.ajp.159.2.276. [DOI] [PubMed] [Google Scholar]
- 14.Saulsman LM, Page AC. The five-factor model and personality disorder empirical literature: A meta-analytic review. Clin Psychol Rev. 2004;23:1055–1085. doi: 10.1016/j.cpr.2002.09.001. [DOI] [PubMed] [Google Scholar]
- 15.Watson PJ, Sawrie SM, Greene RL, Arredondo R. Narcissism and depression: MMPI-2 evidence for the continuum hypothesis in clinical samples. J Pers Assess. 2002;79:85–109. doi: 10.1207/S15327752JPA7901_06. [DOI] [PubMed] [Google Scholar]
- 16.Butcher JN, Dahlstrom WG, Graham JR, Tellegen A, Kaemmer B. MMPI-2: Minnesota Multiphasic Personality Inventory-2: Manual for administration and scoring. Minneapolis, MN: University of Minnesota Press; 1989. [Google Scholar]
- 17.Junemann SH. Affective disorders, personality and personality disorders. Acta Psychiatr Scand. 2003;108:34–40. doi: 10.1034/j.1600-0447.108.s418.8.x. [DOI] [PubMed] [Google Scholar]
- 18.Pfohl B, Black DW, Noyes R, Coryell WH, Barrash J. Axis I and II comorbidity findings: implications for validity. In: Oldham JM, editor. Personality disorders: new perspectives on diagnostic validity. Washington, DC: American Psychiatric Press; 1991. pp. 145–161. [Google Scholar]
- 19.Alnaes R, Torgersen S. The relationship between DSM-III symptom disorders (Axis I) and personality disorder (Axis II) in an outpatient population. Acta Psychiatr Scand. 1988;78:485–492. doi: 10.1111/j.1600-0447.1988.tb06371.x. [DOI] [PubMed] [Google Scholar]
- 20.Skodol AE, Stout RL, McGlashan TH, Grilo CM, Gunderson JG, Shea MT, Morey LC, Zanarini MC, Dyck IR, Oldham JM. Co-occurrence of mood and personality disorders: A report from the Collaborative Longitudinal Personality Disorders Study (CLPS) Depress Anxiety. 10:175–182. [PubMed] [Google Scholar]
- 21.Sedikides C, Rudich EA, Gregg AP, Kumashiro M, Rusbult C. Are normal narcissists psychologically healthy? : Self-esteem matters. J Pers Soc Psychol. 2004;87:400–416. doi: 10.1037/0022-3514.87.3.400. [DOI] [PubMed] [Google Scholar]
- 22.Rose P. The happy and unhappy faces of narcissism. Personality and Individual Differences. 2002;33:379–392. [Google Scholar]
- 23.Campbell WK. Is narcissism really so bad? Psychological Inquiry. 2001;12:214–216. [Google Scholar]
- 24.Campbell WK, Foster CA, Finkel EJ. Does self-love lead to love for others? A story of narcissistic game playing. J Pers Soc Psychol. 2002;83:340–354. doi: 10.1037/0022-3514.83.2.340. [DOI] [PubMed] [Google Scholar]
- 25.Bushman BJ, Baumeister RF. Threatened egotism, narcissism, self-esteem, and direct and displaced aggression: Does self-love or self-hate lead to violence? J Pers Soc Psychol. 1999;76:367–376. doi: 10.1037//0022-3514.75.1.219. [DOI] [PubMed] [Google Scholar]
- 26.Campbell WK, Bush CP, Brunell AB, Shelton J. Understanding the social costs of narcissism: The case of tragedy of the commons. Personality and Social Psychology Bulletin. 2006;31:1358–1368. doi: 10.1177/0146167205274855. [DOI] [PubMed] [Google Scholar]
- 27.Oltmanns TF, Friedman JN, Fiedler ER, Turkheimer E. Perceptions of people with personality disorders based on thin slices of behavior. Journal of Research in Personality. 2004;38:216–229. [Google Scholar]
- 28.Paulhus DL. Interpersonal and intrapsychic adaptiveness of trait self-enhancement: A mixed blessing? J Pers Soc Psychol. 1998;74:1197–1208. doi: 10.1037//0022-3514.74.5.1197. [DOI] [PubMed] [Google Scholar]
- 29.Colvin CR, Block J, Funder DC. Overly positive self-evaluations and personality: Negative implications for mental health. J Pers Soc Psychol. 1995;68:1152–1162. doi: 10.1037//0022-3514.68.6.1152. [DOI] [PubMed] [Google Scholar]
- 30.Betan E, Heim AK, Conklin CZ, Westen D. Countertransference phenomena and personality pathology in clinical practice: An empirical investigation. Am J Psychiatry. 2005;162:890–898. doi: 10.1176/appi.ajp.162.5.890. [DOI] [PubMed] [Google Scholar]
- 31.Pilkonis PA, Heape CL, Proietti JM, Clark SW, McDavid JD, Pitts TE. The reliability and validity of two structured diagnostic interviews for personality disorders. Arch Gen Psychiatry. 1995;52:1025–1033. doi: 10.1001/archpsyc.1995.03950240043009. [DOI] [PubMed] [Google Scholar]
- 32.Hyler SE. Personality Disorder Questionnaire-4. Unpublished test; NYSPI: 1994. [Google Scholar]
- 33.Curran PJ, West SG, Finch JF. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods. 1:16–29. [Google Scholar]


