Abstract
Background
Bevacizumab (Avastin) is a recombinant protein that targets vascular endothelial growth factor (VEGF). In vitro, bevacizumab inhibits VEGF induced cell proliferation and tissue factor production. Abnormal angiogenesis involving VEGF is a central event during the development of choroidal neovascularisation (CNV). The present study was designed to evaluate the short term toxic effects of bevacizumab on retinal function for a therapeutic intraocular application.
Methods
Isolated bovine retinas were perfused with an oxygen pre‐incubated nutrient solution. The electroretinogram (ERG) was recorded as a transretinal potential using silver/silver chloride electrodes. Bevacizumab was added in different concentrations to the nutrient solution for 45 minutes. Thereafter the retina was reperfused for 60 minutes with normal nutrient solution. The percentage of a‐wave and b‐wave reduction during the application of bevacizumab was calculated and compared to control recordings.
Results
During the application of three different concentrations of bevacizumab (0.08 mg/ml, 0.25 mg/ml, 0.8 mg/ml) no significant reduction of the a‐wave and b‐wave amplitude was observed. During the washout, the ERG amplitudes were unchanged.
Conclusion
The present study suggests that an intraocular application of 0.25 mg/ml bevacizumab for the treatment of CNV is reasonable. No significant short term effects of bevacizumab on retinal function were detected, but long term effects cannot be excluded.
Keywords: exudative age related macular degeneration, bevacizumab, electroretinogram, isolated perfused retina, ocular toxicity
Age related macular degeneration (AMD) is the most relevant cause of legal blindness in the elderly population of the industrialised countries.1 The neovascular form of the disease is characterised by the growth of choroidal neovascularisation (CNV) and associated with a dramatic loss in central vision and an irreversible damage of the neurosensory retina.2
Although the exact mechanisms of the CNV development are still not completely clarified, recent studies indicate that an imbalance between angiogenic and antiangiogenic factors may have an important role. One of the major stimuli for ocular neovascularisation seems to be ischaemia, leading to an increase in vascular endothelial growth factor (VEGF) expression.3,4 However, it is not yet clear whether VEGF overexpression is the primary stimulus for the development of CNV.5 The role of other growth factors like transforming growth factor (TGF) or fibroblastic growth factor (FGF), or an additional damage of Bruch's membrane in the pathogenesis, cannot be excluded.6,7 Nevertheless, in current animal models it was shown that VEGF overexpression in the RPE was sufficient to induce CNV.6
Meanwhile, the efficiency of different treatment modes like photosensitising dyes and surgical methods was investigated. However, recent new therapeutic agents like ranibizumab and pegaptanib have been developed for the treatment of exudative AMD targeting VEGF. Another new therapeutic agent is bevacizumab (Avastin), a recombinant humanised anti‐VEGF IgG1, first approved as an antiangiogenic drug for the treatment of metastatic colorectal cancer in combination with chemotherapy.8
Bevacizumab was shown in vitro to inhibit VEGF induced cell proliferation and tissue factor production.9 Bevacizumab is currently used in off‐label treatment and recent studies proposed its application for the treatment of exudative AMD and other devastating eye diseases.10,11,12,13
Today only few data about toxic side effects of bevacizumab on retinal function are available. Recent studies revealed no electrophysiological or histopathological changes, when used at clinically relevant therapeutic concentrations.14,15,16 Our study was designed to investigate the effects of bevacizumab on retinal function using the isolated perfused vertebrate retina technique, an electrophysiological in vitro technique for evaluation of retinal toxicity.17,18
Materials and methods
Materials
Aspartate, glucose, and other chemicals were obtained from Merck at pro analysis grade. Bevacizumab, 100 mg, (Avastin), was purchased from Roche Pharma (Switzerland). Bevazicumab was dissolved in 4 ml of a solvent carrier containing 240 mg α,α‐trehalose × 2H2O, 23.2 mg NaH2PO4 × H2O, 4.8 mg Na2HPO4, 1.6 mg polysorbate 20 and water for injection. The dilution with dissolved bevacizumab, which was prepared for intravenous application, was used in a final concentration of 25 mg/ml as a stock solution, and was stable when stored at 4°C.
Methods
Superfused vertebrate retina assay
Bovine eyes were obtained directly post mortem and transported in darkness in a serum free standard medium containing 120 mM NaCl, 2 mM KCl, 0.1 mM MgCl2, 0.15 mM CaCl2, 1.5 mM NaH2PO4, 13.5 mM Na2HPO4, and 5 mM glucose. The preparation was performed as described recently.17,18
The electroretinogram was recorded in the surrounding nutrient medium via two silver/silver chloride electrodes on either side of the retina. The recording chamber containing a piece of retina was placed in an electrically and optically insulated box. The perfusion velocity was controlled by a roller pump and set to 1 ml/min. The temperature was constantly kept at 30°C. The perfusing medium was pre‐equilibrated and saturated with oxygen. The retina was dark adapted and the electroretinogram was elicited at intervals of 5 minutes using a 1 Hz single white xenon flash for stimulation. The flash intensity was set to 6.3 Mlx at the retinal surface using calibrated neutral density filters (Kodak Wratten Filter).
The duration of light stimulation was 10 μs controlled by a timer (Photopic Stimulator PS33 Plus; Grass, Warwick, RI, USA). The electroretinogram (ERG) was filtered and amplified (100 Hz high pass filter, 50 Hz notch filter, 100 000 × amplification) using a Grass RPS312RM amplifier. The data were processed and converted with an analogue to digital data acquisition board (PCI‐MIO‐16XE‐50; National Instruments, Austin, TX, USA) in a desktop computer (PC compatible) including ERG analysing software (“LabView 7 Express”, National Instruments, Austin, TX, USA).
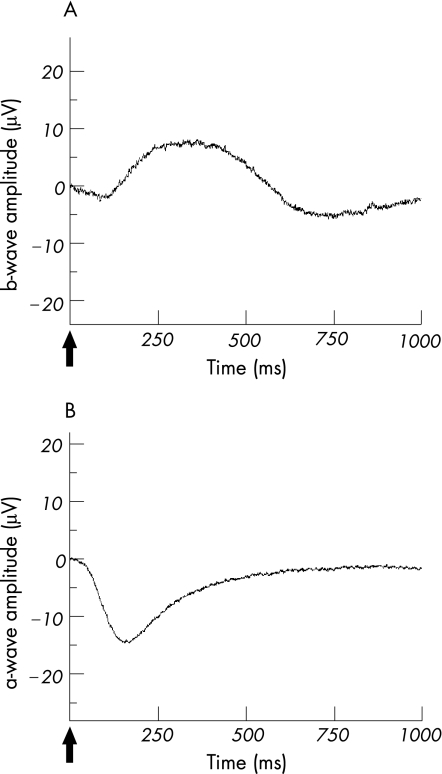
For each experiment a new retina was prepared. The retina was superfused with the serum free nutrient solution and stimulated repeatedly until stable amplitudes were recorded. Bevacizumab from the stock solution was added to the nutrient solution, and responses were recorded for 45 minutes. Thereafter, perfusion with standard solution was resumed for another 60 minutes to observe the b‐wave recovery. The b‐wave amplitude was measured from the trough of the a‐wave to the peak of the b‐wave (fig 1A). Bevacizumab was added to the perfusate at three different concentrations 0.08 mg/ml, 0.25 mg/ml, and 0.8 mg/ml.
Figure 1 The ERG from the isolated perfused bovine retina. (A) The b‐wave is dominant in the ERG of the isolated perfused bovine retina under scotopic light conditions. It results from a 10 μs of light stimulus at a light intensity of 6.3 Mlx. (B) The a‐wave is dominant in the ERG of the isolated perfused bovine retina after blocking the b‐wave by 1 mM aspartate to the nutrient solution. The a‐wave was generated by using a 10 μs light stimulus of 6.3 Mlx at scotopic lighting conditions.
To investigate the effects of bevacizumab on the photoreceptors under scotopic conditions (6.3 Mlx flash light intensity), the b‐wave was suppressed by adding 1 mM aspartate to the nutrient solution and the influence of bevacizumab on the photoreceptor potential P III was analysed. Aspartate is an inhibitor of synaptic transmission at the level of the first retinal synapse and enables the recording of unmasked photoreceptor potential P III by abolishing the b‐wave (fig 1B).19 We recorded stable photoreceptor potential P III for 30 minutes. Thereafter, bevacizumab was added in a concentration of 0.8 mg/ml to the aspartate containing nutrient solution for 45 minutes, because no significant reduction of the a‐wave amplitude was detected at lower concentrations of bevacizumab (data not shown). The changes of the a‐wave amplitude during the application of bevacizumab were recorded and the recovery was followed up for 60 minutes under perfusion with the aspartate containing nutrient solution.
To test the effects of the solvent carrier on the b‐wave amplitude the dilution without bevacizumab was used as a control. Equivalent amounts of the solvent carrier were applied to the nutrient solution for 45 minutes under the same conditions as during the testing of the highest concentration of bevacizumab. Subsequently, the b‐wave recovery was observed for 60 minutes.
Data analysis
The percentage reduction of the a‐wave and b‐wave amplitude was calculated. The ERG recovery was compared with the ERG amplitudes before application of bevacizumab. For the statistical analysis the software “Origin 6.0” (Microcal) was used. Significance was estimated by the Student's t test and levels of p⩽0.05 were considered as statistically significant.
Results
The perfusion of the isolated bovine retina was performed under stable environmental conditions. Osmotic pressure, temperature, and pO2 remained unchanged during perfusion, of either bevacizumab or the control solution.
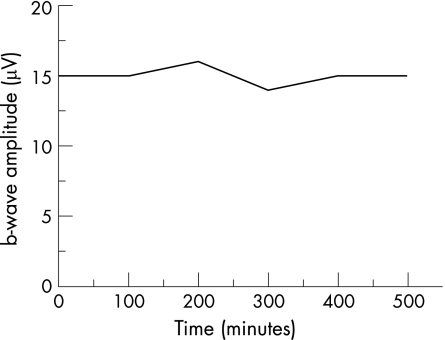
In our experimental setting stable ERG amplitudes were reached within 2 hours of perfusion and the retinal preparations responded constantly to light stimulation for more than 8 hours (fig 2).
Figure 2 Control of long term stability of the isolated perfused bovine retina preparation. The ERG of the isolated perfused retina from a representative experiment was recorded for 8 hours. During this control recording, the standard nutrient solution was used throughout. The altitude of the b‐wave amplitudes remained constant and no reduction of the b‐wave amplitude was observed.
Bevacizumab was effective at an intravitreal applied amount of 1.25 mg.12,13 Therefore, according to the volume of the vitreous humour of approximately 5 ml, the averaged intraocular concentration of bevacizumab was calculated to be 0.25 mg/ml.
Consecutively, we studied the effects of bevacizumab on the parameters of the electroretinogram at 0.08 mg/ml, 0.25 mg/ml, and 0.8 mg/ml.
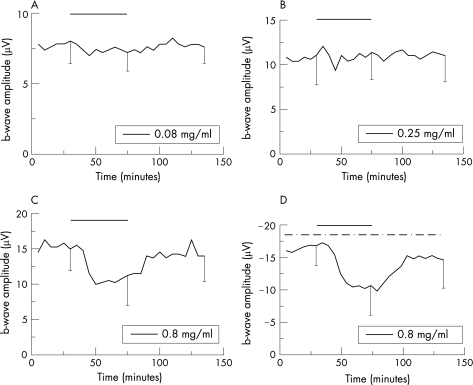
During the application of bevacizumab at 0.08 and 0.25 mg/ml no change of the b‐wave amplitude was found during the exposure time (p = 0.868, p = 0.20; fig 3A and B). Furthermore, after the incubation at these concentrations the b‐wave amplitude remained stable throughout the washout with the standard solution showing no significant difference of the b‐wave amplitude before and after the application of both concentrations of bevacizumab (p = 0.999, p = 0.194; fig 3A and B).
Figure 3 Effects of bevacizumab on the ERG of the isolated perfused bovine retina. Average of representative drug series. The horizontal bar marks the time of bevacizumab application. The dash dotted line in (D) marks the time of aspartate co‐application (1 mM). Bevacizumab concentrations: in (A) a bevacizumab concentration of 0.08 mg/ml was used (n = 5); in B 0.25 mg/ml bevacizumab was applied (n = 5); in (C) and (D) a bevacizumab concentration of 0.8 mg/ml was added (n = 5). Three representative standard deviations for each drug series are given.
At the highest tested concentration of bevacizumab (0.8 mg/ml) we detected a slight reduction of the b‐wave amplitude by 21.4%, which, however, did not reach the level of significance (p = 0.091; fig 3C). During the washout the b‐wave amplitude recovered completely reaching the mean value of b‐wave amplitudes before the application of bevacizumab (p = 0.107; fig 3C).
To investigate the effects of bevacizumab on the photoreceptor potential P III 1 mM aspartate was added and the b‐wave amplitude was reduced continuously until unmasked photoreceptors potential could be recorded.19 The concentration of 0.8 mg/ml bevacizumab was added to the nutrient solution containing aspartate for 45 minutes. According to the previous results no effects of bevacizumab have been observed on the a‐wave amplitude at the lower tested concentrations (data not shown). The washout for the a‐wave recovery was comparably limited to 60 minutes (fig 3D).
The photoreceptor potential P III amplitude was not significantly changed by the concentration of 0.8 mg/ml bevacizumab, but a reduction of the a‐wave amplitude of 35.2% (p = 0.076; fig 3D) was observed during the exposure. This was at a similar degree as it was demonstrated for the b‐wave amplitude. At the washout the a‐wave amplitude recovered fully and no significant difference of the a‐wave amplitudes before the application and at the end of the washout was detected (p = 0.15; fig 3D).
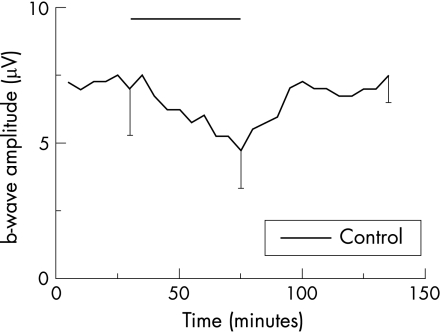
To investigate the cause for the decrease of the ERG responses at the highest tested concentration of bevacizumab, the solvent carrier was used as a control and added to the nutrient solution in an identical amount.
During a 45 minute incubation period, the excipient caused an identical reduction of 28.87% (p = 0.093). This has been recorded in the presence of bevacizumab suggesting that the reduction of the b‐wave amplitude was equivalent to the highest tested concentration of bevacizumab and related to the solution rather than to the drug. During the washout the b‐wave amplitude recovered completely (p = 0.40; fig 4).
Figure 4 Effects of the solvent carrier on the b‐wave amplitude of the isolated perfused bovine retina. Average of representative drug series (n = 4). After reaching equilibrium at a stable b‐wave amplitude, the solvent carrier without bevacizumab was added to the nutrient solution. The black horizontal bar labels the time of the solvent carrier application. After 45 minutes, the solvent carrier was washed out leading to a subsequent recovery of the b‐wave amplitude. Three representative standard deviations are given.
Discussion
The technique of the isolated perfused bovine retina has been often proved to be a reliable and sensitive tool for pharmacological research on retinal function.17,18 The concentrations of the applied drugs are precisely specified and separated from pharmacokinetic effects.
The ERG is a useful indicator. Changes of the ERG during the application reflect toxic effects of the drug directly and exclusively on retinal function, in which a reduced b‐wave indicates a significant dysfunction of retinal neurons. A detailed localisation, which neuronal layer is affected by the applied drug, is enabled by a separate investigation of the photoreceptor function using aspartate.
Strong similarities were detected in the drug induced changes of the ERG when retinas from human and vertebrate animals were compared.20,21 Therefore, the results from the animal experimentation with the isolated perfused retina may be transferred carefully to the human retina.
The aim of our study was to evaluate safe concentrations of bevacizumab for an intravitreal injection. Our study revealed no significant decrease of the ERG amplitudes during the exposure of each tested concentration. At the washout the a‐wave and b‐wave amplitudes remained constant and no delayed reduction was observed.
The highest applied concentration, however, compares to three times the concentration currently being used in clinical practice and the observed slight reduction of the ERG amplitudes seems to be related to the solvent solution rather than bevacizumab itself. The solution contains a phosphate buffer with a pH 6.2. The nutrient solution also includes a phosphate buffer with a pH 7.8. After adding bevacizumab at the highest concentration the nutrient solution obtained a final pH of 7.4. A reduction of the ERG amplitudes caused by a changed pH of the nutrient solution is a known phenomenon, which was observed during the establishment of this in vitro model.17,18 During the last few years several parameters were changed to improve the b‐wave responses. It was disclosed that the pH optimum lies at 7.8 and is required to buffer the acid metabolic products and to keep CO2 in solution. Any variation of the pH of the nutrient solution results in a decrease of the ERG amplitudes. Therefore, the reduction of the ERG amplitudes during our experiments with bevacizumab is caused by a drop in the pH of the nutrient solution and is not related to the drug itself.
The intravitreal preparations of ranibizumab and pegaptanib also contain a buffer system with a pH of 5.5 and 6–7, respectively. The injected volume of pegaptanib is limited to 90 µl and for ranibizumab to 50 µl. An equivalent intravitreal injected volume at the highest tested concentration of bevacizumab, which showed the transient slight reduction of the ERG responses, accords to a volume of 150 µl. Effects on retinal function because of a changed pH following an intravitreal application of pegaptanib or ranibizumab could therefore only be expected at a higher applied volume, which is in the range of 150 µl.
However, in our study no significant acute or prolonged toxic effects of bevacizumab on retinal function were detected at the clinical used concentration of 0.25 mg/ml.12,13
Rosenfeld and Michels reported that both systemic and intraocular administration of bevacizumab were effective in the treatment of CNV.11,13 After treatment the leakage from the CNV decreased and retinal thickening as well as subretinal fluid was reduced.13 The anatomical improvement was actually associated with an increase in visual acuity and well tolerated without any serious ocular adverse events.13
An analogous effect was observed in the treatment of CNV caused by pathological myopia.22 Two of three patients with CNV, which was refractory to other treatments, responded after the intravenous application of bevacizumab. Concomitant with the morphological recovery an increase of visual acuity was detected in both patients.22
Owing to the clinically intriguing results an intraocular application of bevacizumab seems to be a promising treatment of the exudative AMD and other neovascular eye diseases.
The possibility of an intraocular application reduces the systemic exposure to a certain degree, although a systemic load cannot be excluded after multiple re‐injections. Little has been published on the ocular toxicity following intraocular application. Patients treated with bevacizumab showed no severe ocular adverse effects related to the drug itself.12,13 Recent electrophysiological and histopathological animal studies did not suggest any ocular toxicity for bevacizumab at therapeutic concentrations.14,16 Ganzfeld ERGs from humans were not impaired. Multifocal ERGs even showed an improvement of the macular responses.15
A single intraocular injection of bevacizumab is limited by the reduction of effective vitreous drug levels over time. In addition, it must be considered that bevacizumab targets only VEGF and has no direct effect on other mediators like FGF and TGF. Because of this, and the fact that the therapy is symptomatic rather than causative, a single injection may not be sufficient to halt the progression of the CNV for a longer period. Repeated injections are required unless the stimulus for VEGF synthesis is shut down. Therefore, attention must be focused on a possible onset of long term effects from intraocular anti‐VEGF treatment. To avoid adverse events the number of anti‐VEGF treatments should be limited and patients receiving bevacizumab, pegaptanib, or ranibizumab should be controlled using fine meshed medical and ophthalmological monitoring.
In conclusion, the isolated superfused retina is well defined to evaluate short term effects on retinal function. However, long term effects cannot be excluded. Short term toxic effects were not detected at a concentration of 0.25 mg/ml, which is closest to the estimated concentration in vivo.
Clinical and experimental changes of retinal function allow careful conclusion concerning the clinical situation. We are aware that no definitive conclusions can be drawn based on a single in vitro study. However, an impairment of the electroretinogram because of the drug bevacizumab could not be detected. Therefore, the treatment of exudative AMD and other neovascular eye diseases with bevacizumab seems reasonable.
Acknowledgements
We thank Ms Kayalvizhi Radhakrishnan for checking the manuscript.
The Tuebingen Bevacizumab Study Group
Sabine Aisenbrey; Karl Ulrich Bartz‐Schmidt; Christioph Deuter; Faik Gelisken; Salvatore Grisanti; Sylvie Julien; Sigrid Henke‐Fahle; Peter Heiduschka; Werner Inhoffen; Martin Leitritz; Matthias Lüke; Swaantje Peters; Katrin Petermeier; Ulrich Schraermeyer; Ana Sierra; Heike Strotmann; Martin Spitzer; Peter Szurman; Olcay Tatar; Aysegül Tuara; Michael Völcker; Max Warga; Efdal Yörük; Barbara Wallenfels‐Thilo; Focke Ziemssen
Abbreviations
AMD - age related macular degeneration
CNV - choroidal neovascularisation
ERG - electroretinogram
FGF - fibroblastic growth factor
TGF - transforming growth factor
VEGF - vascular endothelial growth factor
References
- 1.Hyman L. Epidemiology of eye disease in the elderly. Eye 19871330–341. [DOI] [PubMed] [Google Scholar]
- 2.Bressler N, Bressler S, Fine S. Age related macular degeneration. Surv Ophthalmol 198832375–413. [DOI] [PubMed] [Google Scholar]
- 3.Ferrara N. Vascular endothelial growth factor: basic science and clinical progress. Endocr Rev 200425581–611. [DOI] [PubMed] [Google Scholar]
- 4.Shweiki D, Itin A, Soffer D.et al Vascular endothelial growth factor induced by hypoxia may mediate hypoxia‐initiated angiogenesis. Nature 1992359843–845. [DOI] [PubMed] [Google Scholar]
- 5.Kvanta A, Algvere P V, Berglin L.et al Subfoveal fibrovascular membranes in age‐related macular degeneration express vascular endothelial growth factor. Invest Ophthalmol Vis Sci 1996371929–1934. [PubMed] [Google Scholar]
- 6.Schwesinger C, Yee C, Rohan R M.et al Intrachoroidal neovascularization in transgenic mice overexpressing vascular endothelial growth factor in the retinal pigment epithelium. Am J Ophthalmol 20011581161–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spilsbury K, Garrett K L, Shen W Y.et al Overexpression of vascular endothelial growth factor (VEGF) in the retinal pigment epithelium leads to the development of choroidal neovascularization. Am J Ophthalmol 2000157135–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Horwitz H, Fehrenbacher J, Novotny W.et al Bevacizumab plus irnotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 20043502335–2342. [DOI] [PubMed] [Google Scholar]
- 9.Wang Y, Fei D, Vanderlaan M.et al Biological activity of bevacizumab, a humanized anti‐VEGF antibody in‐vitro. Angiogenensis 20057335–345. [DOI] [PubMed] [Google Scholar]
- 10.Grisanti S, Biester S, Peters S.et al Intracameral bevacizumab for rubeosis iridis. Am J Ophthalmol 2006;(in press) [DOI] [PubMed]
- 11.Michels S, Rosenfeld J R, Puliafito C A.et al Systemic bevacizumab (Avastin) therapy for neovascular age‐related macular degeneration.twelve‐week results of an uncontrolled open‐label clinical study. Ophtalmology 20051121035–1047. [DOI] [PubMed] [Google Scholar]
- 12.Rosenfeld J R, Fung A E, Puliafito C A. Optical coherence tomography findings after an intravitreal injection of bevacizumab (Avastin) for macular edema from central vein occlusion. Ophthalmic Surg Lasers Imaging 200636336–339. [PubMed] [Google Scholar]
- 13.Rosenfeld P J, Mosfeghi A A, Puliafito C A. Optical coherence tomography findings after an intravitreal injection of bevacizumab (Avastin) for neovascular age‐related macular degeneration. Ophthalmic Surg Lasers Imaging 200536331–335. [PubMed] [Google Scholar]
- 14.Manzano R P, Peyman G A, Khan P.et al Testing intravitreal toxcitiy of bevacizumab (Avastin). Retina 200626257–261. [DOI] [PubMed] [Google Scholar]
- 15.Maturi R K, Bleau L A, Wilson D L.et al Electrophysiologic findings after intravitreal bevacizumab (Avastin) treatment. Retina 200626270–274. [DOI] [PubMed] [Google Scholar]
- 16.Shahar J, Avery R L, Heilweil G.et al Electrophysiologic and retinal penetration studies following intravitreal injection of bevacizumab (Avastin). Retina 200626262–269. [DOI] [PubMed] [Google Scholar]
- 17.Lüke M, Weiergräber M, Brand C.et al The isolated perfused bovine retina‐A sensitive tool for pharmacological research on retinal function. Brain Res Brain Res Protoc 20051627–36. [DOI] [PubMed] [Google Scholar]
- 18.Sickel W. Respiratory and electrical responses to light stimulation in the retina of the frog. Science 1965148648–651. [DOI] [PubMed] [Google Scholar]
- 19.Hanawa I, Tateishi T. The effect of aspartate on the electroretinogram of the vertebrate retina. Experientia 1970261311–1312. [DOI] [PubMed] [Google Scholar]
- 20.Lüke C, Walter P, Bartz‐Schmidt K U.et al Effects of antiviral agents on retinal function in vertebrate retina. In: Green K, ed. Advances in ocular toxicology. New York: Plenum Press, 1997112
- 21.Walter P, Lüke C, Sickel W.et al Antibiotics and light responses in superfused bovine retina. Cell Moll Neurobiol 19991987–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nguyori Q D, Shah S, Tatlipinar S.et al Bevacizumab suppresses choroidal neovascularisation caused by pathological myopia. Br J Ophthalmol 2005891368–1370. [PMC free article] [PubMed] [Google Scholar]