Fewer than 50 cases of invasive group A streptococcal (iGAS) eyelid infections have been reported.1 Predisposing factors include skin trauma or surgery2,3,4,5,6,7 and immunosuppression.3,4 iGAS preseptal cellulitis can be devastating; potentially leading to streptococcal gangrene of the eyelids,1 which can be fatal with a mortality of 40% in the presence of bacteraemia, and an overall mortality of 18%.1
Case report
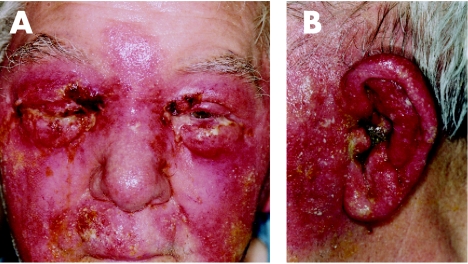
An 80 year old man with rheumatoid arthritis presented with rapidly spreading periorbital erythema involving both eyes within 12 hours, having started at the left pinna which was markedly swollen and discharging (fig 1).
Figure 1 Preseptal cellulitis with pinna involvement.
Empirical treatment was begun for possible necrotising streptococcal infection with clindamycin 900 mg four times daily and imipenem 500 mg four times daily. Features suggestive of iGAS infection included the elevated creatine kinase (243 IU/l) and, in particular, marked blistering and a serosanguinous discharge rarely found in staphylococcal infections.
GAS sensitive to penicillin, clindamycin and linezolid was cultured from eye and ear swabs. Despite aggressive treatment, on day 3 he remained pyrexial, the C reactive proyein (CRP) peaking at 374 g/l.
However, within 24 hours of adding oral linezolid, 600 mg twice daily, the CRP fell to 208, with a dramatic improvement in the cellulitis. Examination of the right eye was impossible because of gross swelling, subcutaneous emphysema and thick scab. Very limited left eye examination was possible; visual acuity was 6/9. There was no relative afferent pupil defect.
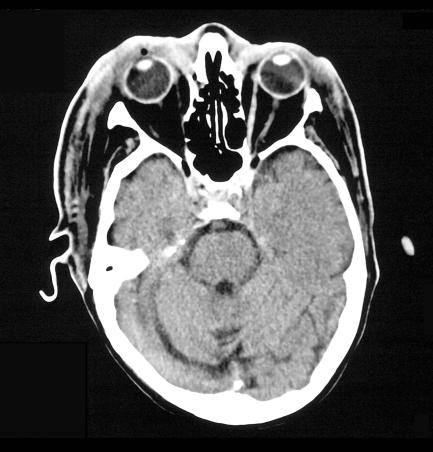
Computed tomography imaging (fig 2) confirmed the clinical impression of preseptal infection.
Figure 2 Computed tomography showing preseptal cellulites.
By day 8, the cellulitis had largely resolved, exposing a tense right upper lid abscess yielding sterile pus on drainage. There was localised eyelid necrosis but debridement was unnecessary. By day 21, both eyes could close adequately despite upper lid skin defects (right larger than left, fig 3). On discharge at 3 weeks, the right upper lid had mild ectropion secondary to healing, and corrective lid surgery was deferred.
Figure 3 Upper lid skin defects after cellulitis resolution.
Comment
Our patient presented with a severe iGAS infection, his only risk factor was rheumatoid arthritis. Fortunately he did not develop orbital cellulitis where more serious surgical intervention has been necessary—for example, multiple drainage of abscesses or evisceration8 and even exploration of the neck.3
Our case demonstrates how difficult iGAS can be to treat. Although the creatine kinase was raised, there were no other features of myositis or toxic shock syndrome.6
Penicillins are largely ineffective in severe iGAS infection because of the Eagle9 effect; bacteria in the non‐dividing or stationary phase being immune to cell wall active antibiotics.
Debridement being unnecessary once linezolid was added, there was no definitive histopathological evidence of necrotising fasciitis.
This is the first case of iGAS periorbital infection treated successfully with linezolid. A novel synthetic oxazolidinone antibiotic, linezolid is equally active orally and intravenously, and effective against Gram positive organisms, including streptococci and methicillin resistant Staphylococcus aureus (MRSA).10 Both clindamycin and linezolid prevent toxin production by inhibiting bacterial protein synthesis initiation at the ribosome, but linezolid acts earlier in the process.
Clindamycin has been the drug of choice for severe iGAS infections. In our experience, the delayed response to high dose clindamycin was unusual. The addition of linezolid had a dramatic clinical effect, but we are uncertain whether linezolid's earlier mechanism of action explains why it appeared to be more effective than clindamycin in our patient. The suggestion11 that using both agents together dramatically decreases toxin release could equally be borne out in this case.
Footnotes
The authors have no financial interest in the products discussed.
The patient has given full verbal and written consent for publication of the case and of the included photographs and scan image.
References
- 1.Shayegani A, MacFarlane D, Kazim M.et al Streptococcal gangrene of the eyelids and orbit. Am J Ophthalmol 1995120784–792. [DOI] [PubMed] [Google Scholar]
- 2.Overholt E W, Flint P W, Overholt E L. Necrotizing fasciitis of the eyelids. Otolaryngol Head Neck Surg 1992106339–343. [DOI] [PubMed] [Google Scholar]
- 3.Rose G E, Howard D J, Watts M R. Periorbital necrotising fasciitis. Eye 19915736–740. [DOI] [PubMed] [Google Scholar]
- 4.Marshall D H, Jordan D R, Gilberg S M.et al Periocular necrotising fasciitis. Ophthalmology 19971041857–1862. [DOI] [PubMed] [Google Scholar]
- 5.Jordan D R, Mawn L, Marshall D H. Necrotising fasciitis caused by group A streptococcus infection after a laser blepharoplasty. Am J Ophthalmol 1998125265–266. [DOI] [PubMed] [Google Scholar]
- 6.Ingraham H J, Ryan M E, Burns J T.et al Streptococcal preseptal cellulitis complicated by the toxic streptococcus syndrome. Ophthalmology 19951021223–1226. [DOI] [PubMed] [Google Scholar]
- 7.Kronish J W, McLeish W M. Eyelid necrosis and periorbital necrotizing fasciitis: report of a case and review of the literature. Ophthalmology 19919892–98. [DOI] [PubMed] [Google Scholar]
- 8.Ng S G, Nazir R, Sabhudi C P K.et al Necrotizing orbital cellulitis. Eye 200215173–177. [DOI] [PubMed] [Google Scholar]
- 9.Eagle H. Experimental approach to the problem of treatment failure with penicillin. I. Group A streptococcal infection in mice. Am J Med 195213389–399. [DOI] [PubMed] [Google Scholar]
- 10.Stalker D J, Junbluth G L. Clinical pharmacokinetics of linezolid, a novel oxazolidinone antibacterial. Clin Pharmacokinet 2003421129–1140. [DOI] [PubMed] [Google Scholar]
- 11.Coyle E A, Cha R, Rybak N J. Influences of linezolid, penicillin, and clindamycin, alone and in combination, on streptococcal pyrogenic exotoxin A release. Antimicrob Agents Chemother 2003471752–1755. [DOI] [PMC free article] [PubMed] [Google Scholar]