Retinal pigment epithelium (RPE) tears are well recognised complications of pigment epithelial detachments (PED) in age related macular degeneration (AMD) and may arise spontaneously after trauma, photocoagulation, or photodynamic therapy (PDT).1 Rosenfeld et al recently reported favourable results after intravitreal (IV) bevacizumab (Avastin) injection in neovascular AMD.2 We present two patients, who developed an RPE tear after an intravitreal Avastin injection.
Case reports
The first case was a 64 year old man with an occult CNV with a PED in the right eye (fig 1A–C). His visual acuity (VA) gradually declined from 20/30 to 20/60. Four days after an uneventful IV injection of 0.05 ml Avastin, the patient noted a sudden drop in VA. His VA was 20/80 while fluorescein angiography (FA) and optical coherence tomography revealed a large RPE tear (fig 2A–C). The second case was a 84 year old woman with an occult CNV with a PED. Her VA was 20/60 when she required an IV Avastin injection. When she returned for her second IV injection, we noticed a fresh RPE tear in the inferotemporal quadrant. Both patients developed an RPE tear after their first IV injection. Both RPE tears were observed also among the first 50 intravitreal Avastin injections at our institution.
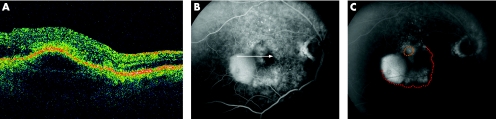
Figure 1 (A) Optical coherence tomography (OCT) before an intravitreal injection. The horizontal OCT scan shows a curved hyper‐reflective band under the retina, corresponding to a shallow pigment epithelial detachment. (B, C) Fluorescein angiography (FA) before an intravitreal injection. The early frames of the FA demonstrate a hyperfluorescence temporal to the fovea. This round PED has a connection to an occult CNV, superior to the fovea. The white arrow indicates the length, location, and direction of the corresponding OCT scan. (C) In the late phase of the FA there is a moderate pooling of dye in the PED. The RPE tear will later occur at the margin between attached and detached RPE. The red dots indicate the edge of the RPE tear, the brown dots indicate the location of the contracted RPE.
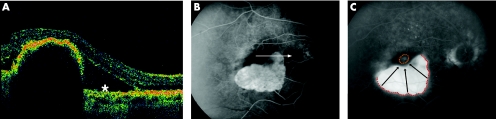
Figure 2 (A) Optical coherence tomography (OCT) after the intravitreal injection. On OCT, there is a dome‐shaped hyper‐reflective band of the contracted RPE. Nasal to the RPE tear is the missing RPE choriocapillaris‐complex (asterisk). The hyper‐reflective area under the retina corresponds to subretinal fluid. (B, C) Fluorescein angiography (FA) after the intravitreal injection. In the early FA, there is a large hyperfluorescent window defect in the area of the former PED including the adjacent occult CNV. A square dark, hypofluorescent band corresponds to the contracted and heaped up RPE. The white arrow indicates the length, location, and direction of the corresponding OCT scan. (C) The late phase of the FA demonstrates an increased fluorescence in the bed of the denuded RPE. The inferior edge of the RPE tear is marked by red dots. The RPE contracted from the inferior edge of the PED towards the superior location of the occult CNV (brown dots) in a radial fashion (black arrows).
Comment
Four possible mechanisms may have induced the development an acute RPE tear in our patients. Firstly, a spontaneous rupture of a PED may occur. Secondly, the deformation of the globe during the insertion of the needle may cause a tearing of the RPE. Thirdly, the IV injection may induce a syneresis and vitreous incarceration at the insertion site, leading to a consecutive vitreoretinal traction.3 Fourthly, the antiangiogenic drug itself can modulate the permeability and activity of the CNV, thus inducing a contraction of the CNV. As the RPE tears in our patients occurred soon after the IV injection, they developed presumably as a direct consequence of the therapy, rather than the natural progression of the lesion.
For more than 10 years at our institution we performed several hundred intravitreal injections with a variety of different drugs for numerous vitreoretinal diseases including AMD.4 Also the VEGF Inhibition Study in Ocular Neovascularisation (VISION) treated 1186 patients with more than 9000 IV Macugen injections and reported no RPE tears during a 2 year follow up.5 As IV Avastin injections are an “off‐label use of a FDA approved drug,” several physicians established an internet register to track adverse events (https://www.formrouter.net/forms@PACEA/AvastinSafetySurvey05_A.aspx). This register so far contains no RPE tear (Phil Rosenfeld, Anne Fung, personal communication).
In conclusion, we present two patients with occult CNV and PED who developed a RPE tear early after the first IV injection of Avastin. The role of intravitreal Avastin therapy in the development of this RPE tear is not clear.6 As occult CNV are frequently accompanied by a PED, we may face a higher incidence of acute RPE tears after intravitreal antiangiogenic injections compared to classic CNV after PDT.1 Patients need to be informed about this possible complication in this novel off‐label use drug.
Footnotes
Financial support: none.
Proprietary interest: none.
In part presented at the ASRS, Cannes 2006.
References
- 1.Gelisken F, Inhoffen W, Partsch M.et al Retinal pigment epithelial tear after photodynamic therapy for choroidal neovascularization. Am J Ophthalmol 2001131518–520. [DOI] [PubMed] [Google Scholar]
- 2.Rosenfeld P J, Moshfeghi A A, Puliafito C A. Optical coherence tomography findings after an intravitreal injection of bevacizumab (Avastin) for neovascular age‐related macular degeneration. Ophthalmic Surg Lasers Imaging 200536331–335. [PubMed] [Google Scholar]
- 3.Meyer C H, Toth C A. Retinal pigment epithelial tear with vitreomacular attachment: a novel pathogenic feature. Graefes Arch Clin Exp Ophthalmol 2001239325–333. [DOI] [PubMed] [Google Scholar]
- 4.Hesse L. Tissue‐type plasminogen activator. An enzyme with multiple uses in ophthalmology. Ophthalmologe 199794366–371. [PubMed] [Google Scholar]
- 5.Gragoudas E S, Adamis A P, Cunningham E T., Jret al VEGF Inhibition Study in Ocular Neovascularization Clinical Trial Group. Pegaptanib for neovascular age‐related macular degeneration. N Engl J Med 20043512805–2816. [DOI] [PubMed] [Google Scholar]
- 6.Kroll P, Meyer C H. Which treatment is best for which AMD patient? [editorial]. Br J Ophthalmol 200690128–130. [DOI] [PMC free article] [PubMed] [Google Scholar]