Peripapillary choroidal neovascularisation is an uncommon entity that can be associated with significant visual loss. It has been noted with papilloedema resulting from pseudotumour cerebri.1 Treatment for peripapillary choroidal neovascularisation has involved observation, thermal laser photocoagulation, or surgical excision.2 We report a case of peripapillary choroidal neovascularisation from papilloedema secondary to pseudotumour cerebri that was successfully treated with combination photodynamic therapy and juxtascleral triamcinolone acetonide.
Case report
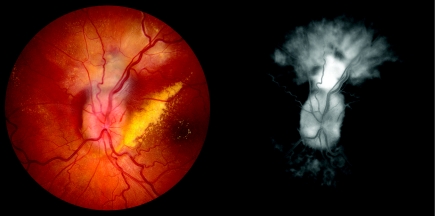
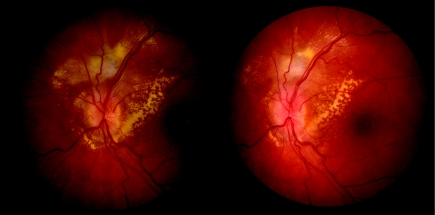
A 27 year old woman presented to the neuro‐ophthalmology clinic for headaches and transient visual obscurations in both eyes. Visual acuity was 20/20 in both eyes and fundus examination was significant for optic nerve oedema in both eyes. After undergoing diagnostic testing, which included visual field analysis, lumbar puncture, and magnetic resonance imaging, a diagnosis of pseudotumour cerebri was firmly established. The patient was started on oral acetazolamide and noticed improvement of symptoms. At a follow up visit 4 months later, she presented with progressive vision loss in the left eye. Visual acuity was 20/30 in the left eye and fundus examination revealed optic nerve oedema, in addition to subretinal fluid and blood adjacent to the nerve. Fluorescein angiography was performed and confirmed the presence of a peripapillary choroidal neovascular membrane (fig 1). The patient underwent combination treatment with photodynamic therapy with verteporfin (Visudyne, Novartis Pharmaceuticals, East Hanover, NJ, USA) and juxtascleral triamcinolone acetonide on the same day. The spot size for photodynamic therapy was determined by measuring the greatest radial distance from the optic nerve edge to the border of the area of leakage on the fluorescein angiogram and a total dose of 18 J/cm2 was delivered. Triamcinolone acetonide, 40 mg, was injected into the juxtascleral space after a conjunctival cutdown was performed 8 mm posterior to the limbus. Six months after combination therapy, visual acuity in the left eye improved to 20/20 and there was resolution of the subretinal fluid and no evidence of leakage from the choroidal neovascular membrane (fig 2). In addition, intraocular pressure remained within normal limits at all office visits.
Figure 1 Left eye of a patient with papilloedema and a peripapillary choroidal neovascular membrane. There is prominent subretinal haemorrhage and exudation near the peripapillary choroidal neovascular membrane in the colour photograph (left), and a fluorescein angiogram reveals late leakage (right).
Figure 2 Colour photographs after treatment with combination photodynamic therapy and juxtascleral triamcinolone acetonide. At 2 months after treatment (left), there is a resolving edge of exudation and at 6 months after treatment (right), the choroidal neovascular membrane has decreased in size and there is resolution of subretinal blood.
Comment
The association of choroidal neovascularisation with papilloedema is not completely understood. It has been suggested that the physical deformation of the peripapillary tissues may create the required path for the growth of the choroidal neovascular membrane.3 Laser photocoagulation for peripapillary choroidal neovascularisation causes damage to the overlying retina and has been associated with vitreous haemorrhage and branch arteriole occlusion. Surgical removal of peripapillary lesions is invasive and can often lead to defects in the retinal pigment epithelium.2 Photodynamic therapy has recently been reported to be safe and successful in the treatment of peripapillary choroidal neovascularisation from age related macular degeneration and presumed ocular histoplasmosis syndrome.4 The advantage of photodynamic therapy is the reduced risk of collateral damage to surrounding tissue, compared to surgical excision and thermal laser photocoagulation. As it has been used in the treatment of circumscribed choroidal haemangioma, photodynamic therapy does not appear to have an adverse affect on the optic nerve.5 However, photodynamic therapy can cause a release of angiogenic factors. Triamcinolone acetonide has antiangiogenic and antipermeability effects and combination therapy with photodynamic therapy and juxtascleral triamcinolone acetonide has been shown to be beneficial in treating subfoveal choroidal neovascular membranes related to age related macular degeneration.6
Peripapillary choroidal neovascularisation can cause visual loss in patients with papilloedema from pseudotumour cerebri. Although a longer follow up may be necessary, we report the successful treatment of a peripapillary choroidal neovascular membrane related to papilloedema with combination photodynamic therapy and juxtascleral triamcinolone acetonide.
References
- 1.Morse P H, Leveille A S, Antel J P.et al Bilateral juxtapapillary subretinal neovascularization associated with pseudotumor cerebri. Am J Ophthalmol 198191312–317. [DOI] [PubMed] [Google Scholar]
- 2.Castellarin A A, Sugino I K, Nasir M.et al Clinicopathological correlation of an excised choroidal neovascular membrane in pseudotumour cerebri. Br J Ophthalmol 199781994–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morse P H, Leveille A S, Antel J P.et al Bilateral juxtapapillary subretinal neovascularization associated with pseudotumor cerebri. Am J Ophthalmol 198191312–317. [DOI] [PubMed] [Google Scholar]
- 4.Rosenblatt B J, Shah G K, Blinder K. Photodynamic therapy with verteporfin for peripapillary choroidal neovascularization. Retina 20052533–37. [DOI] [PubMed] [Google Scholar]
- 5.Robertson D M. Photodynamic therapy for choroidal hemangioma associated with serous retinal detachment. Arch Ophthalmol 20021201155–1161. [DOI] [PubMed] [Google Scholar]
- 6.Van de M A, Sandhu S S, Kak R.et al Effect of posterior juxtascleral triamcinolone acetonide on choroidal neovascular growth after photodynamic therapy with verteporfin. Ophthalmology 20051121896–1903. [DOI] [PubMed] [Google Scholar]