Abstract
Aim
To investigate the relationship between the size of macular holes and the possible benefit of internal limiting membrane (ILM) peeling.
Methods
84 consecutive cases of idiopathic macular hole followed up for at least 3 months were included in this retrospective study. Surgery comprised pars plana vitrectomy, peeling of any epiretinal membrane, 17% C2F6 (hexafluoroethane) gas filling and 10 days of positioning. 36 eyes had ILM peeling. The main outcome measure was the macular hole closure rate checked by optical coherence tomography.
Results
The overall postoperative closure rate was 90.5%. For macular holes ⩾400 μm in diameter, the rate was 100% with ILM peeling versus 73.3% without (p = 0.015). For smaller macular holes, the rates were 100% in both groups. Postoperative gain in visual acuity was not significantly different in eyes with ILM peeling and those without.
Conclusions
ILM peeling does not seem to be useful for macular hole <400 μm in diameter. Its likely benefit has to be investigated for larger macular hole sizes, for which the failure rate is higher.
Conventional surgery for idiopathic macular holes currently results in hole closure in about 85% of idiopathic cases.1,2 Presently, the most popular procedure proposed to increase this rate is internal limiting membrane (ILM) peeling, but the benefit of this procedure is still controversial. Recent studies have shown that the size of the hole is strongly predictive of postoperative success or failure in macular hole surgery.2,3 We postulated that there may be a relationship between hole size and the benefit, if any, of ILM peeling. The present retrospective study was designed to check this hypothesis.
Methods
Patients
The charts of all consecutive patients operated on for idiopathic macular hole during the year 2001 in the Department of Ophthalmology, Hôpital Lariboisière, Paris, France, were retrospectively reviewed; all patients followed up postoperatively for 3 months or more, with available preoperative and postoperative data, were included in this study. Ethics committee approval was not required for this retrospective study, as it was based on medical records.
Intervention procedures
Surgery consisted of pars plana vitrectomy, peeling of any epiretinal membrane, 17% C2F6 (hexafluoromethane) gas filling and 10 days of face‐down positioning. We chose to look at the 2001 data because, by chance, during that year, nearly half the eyes (36/84) in the series also had their ILM peeled off during surgery. For peeled eyes, indocyanine green ((ICG), 0.1 ml, 2.5 mg/ml, applied for 3 min) was used to visualise the ILM more clearly and to be sure it was peeled off all round the foveola (we later abandoned the use of this dye). In the other cases, no attempt was made to peel off the ILM and no ICG was used.
Data
For all patients, ophthalmological examination included preoperative and postoperative best‐corrected visual acuity, fundus biomicroscopy and optical coherence tomography (OCT) scanning. The stage and duration of the hole were also noted. Postoperative anatomical outcome was determined clinically and checked by OCT in all cases.
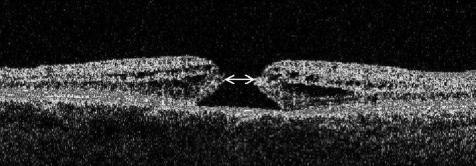
As regards to preoperative OCT, macular hole diameter was measured on 3 mm horizontal OCT scans, which allow a lateral resolution of 30 μm (OCT1, Zeiss Humphrey Instruments, Dublin, California, USA). Care was always taken to ensure that the scan passed through the middle of the hole. The OCT measurement used in this study was the “aperture diameter” of the macular hole, corresponding, on biomicroscopy, to the apparent size of the hole (fig 1).
Figure 1 Optical coherence tomography (OCT) scan of a macular hole. The OCT measurement used in this study was the aperture diameter of the macular hole, corresponding, on biomicroscopy, to the apparent size of the hole (arrow).
Statistical analysis
Results are expressed as means (standard deviation (SD)). Mann–Whitney's non‐parametric test was used to compare the statistical distribution of the parameters measured. Fisher's exact test was used for categorical variables.
Results
In all, 84 eyes of 81 patients (49 women and 32 men) were included. Patients' mean age was 67.31 (range 49–85, median 68) years. Table 1 gives the characteristics and OCT stages of macular holes.4 For the 84 eyes, the overall postoperative closure rate (ie, closure after one operation) was 90.5%. This rate was higher when the ILM was peeled off than when it was not (100% v 83.3, p = 0.009). For macular hole sizes ⩾400 μm in diameter, the closure rate was 100% with ILM peeling versus 73.3 without (p = 0.015). For smaller macular hole sizes, the rates were 100% in both groups (p>0.99). More details are shown in table 2.
Table 1 Characteristics of macular holes.
| Characteristics | Values |
|---|---|
| No of MHs | n = 84 |
| Stage* | |
| Stage 2 | 22 |
| Stage 3 | 33 |
| Stage 4 | 29 |
| Duration before surgery (months) | |
| Mean | 11.13 |
| Range | <1–72 |
| Median | 6 |
MHs, macular holes.
*Optical coherence tomography staging: stage 2, full‐thickness MH with vitreous attached to the edge of the hole through the pseudo‐operculum; stage 3, vitreous detached from the macula but attached to the optic disc; stage 4, complete posterior vitreous detachment.4
Table 2 Postoperative closure rates for the idiopathic macular holes.
| ILM peeled off | ILM not peeled off | p Value | |
|---|---|---|---|
| All diameters (n = 84) | 100% (36/36) | 83.3% (40/48) | 0.009 |
| MH⩾400 μm (n = 51) | 100% (21/21) | 73.3% (22/30) | 0.015 |
| MH<400 μm (n = 33) | 100% (15/15) | 100% (18/18) | >0.99 |
ILM, internal limiting membrane; MH, macular hole.
No statistical difference was observed between failed holes and others for the duration of the macular hole (mean 12.8 (SD 9.6) v 11.0 (14.2) months, p = 0.281). In the whole series, there was no significant difference between the postoperative gain in visual acuity of the eyes whose ILM was peeled off and the others (−0.287 (0.493) and −0.234 (0.504) logMAR (logarithm of the minimum angle of resolution) units, p = 0.856, respectively). The result was the same when only successful cases of peeling (−0.287 (0.493)) and non‐peeling (−0.361 (0.398)) logMAR (logarithm of the minimum angle of resolution) units were considered (p = 0.203).
Discussion
ILM peeling is the most recent change in the procedure for macular hole surgery proposed to improve the rate of macular hole closure,5,6,7,8 and has become popular even though its benefit has not been clearly shown. In this series, we showed that analysis of the crude statistics for the technique of macular hole surgery, with or without ILM peeling, must take into account the size of the hole. In our series, the closure rate for idiopathic macular holes was 100% for cases in which the ILM was peeled off versus 83.3% for cases in which it was not (p = 0.009). However, in actual fact, this benefit concerned only larger holes for which the closure rate rose significantly, from 73.3% to 100%, when the ILM was peeled off. For holes <400 μm, the rate was already 100% with the conventional technique, and therefore could not be increased by ILM peeling (table 2).
Although in a few cases small macular holes may also fail to close, that macular hole diameter has a major role in the closure rate was recently shown by several authors.2,3 In a retrospective series of 40 cases studied with OCT, Ip et al3 found a closure rate of 92% for idiopathic macular holes <400 μm in diameter versus 56% for larger holes. In an analysis of the closure rate for macular holes operated on in our department in 2000, we too found that the rate for macular hole sizes <400 μm was significantly higher than the rate for larger holes. We then tested this finding on an independent series of macular holes operated on in our department in 2001, and the results confirmed our previous findings.9 Consequently, macular hole diameter can be considered to be strongly predictive of the postoperative success or failure of macular hole closure. We therefore wonder whether there is any justification for ILM peeling when macular hole diameter is <400 μm, as the closure rate for conventional operation of these holes is already extremely high. The results of this study suggest that peeling results in no clear benefit in terms of closure rates for holes <400 μm. This question is even more relevant if we consider that not only has the benefit of ILM peeling not yet been proved, but that there is also controversy about its harmlessness, especially when it is carried out using a dye such as ICG. Indeed, it has been suggested that ILM peeling results in minor but demonstrable damage to the adjacent retina.10,11 This damage is sometimes seen as a dissociated optic nerve fibre layer appearance of the fundus,12,13,14,15 and results in moderate functional impairment in most eyes.16,17 Moreover, there is still controversy about the safety of ICG, the most popular dye used to stain the ILM.18,19,20,21 Consequently, ILM peeling would be justified only if it could be proved to be beneficial. In the absence of such proof, it seems more suitable to reserve peeling for macular hole subgroups for which the potential benefit might outweigh the risks. Our results suggest that macular holes with a diameter of ⩾400 μm may be included in these subgroups, but that smaller macular hole sizes should probably be excluded. Prospective studies with randomisation might better answer this question, but our retrospective data strongly support this hypothesis.
Our study was not designed to assess the value of ILM peeling in macular hole surgery in general, which can be shown only by a randomised prospective study. Our results only highlight the relationship between macular hole size and the possible benefit of ILM peeling. We recognise that other prognostic factors such as initial visual acuity and the duration or stage of the hole may also be considered. However, the size of the hole measured by OCT seems the most suitable parameter to consider, as it is an objective and reproducible measurement and has already been clearly shown to be an important factor predictive of postoperative closure. We also admit that our conclusions might be biased because of the retrospective design of our study. Nevertheless, they may be useful for designing future randomised studies. Indeed, when hundreds of macular holes may be necessary to show a clear rise of 10% in the closure rate (from 85% for conventional surgery to 95% with ILM peeling), for a subgroup with a lower closure rate (here, 73% for macular hole diameter ⩾400 μm) the benefit would be easier to prove if ILM peeling really raised the closure rate to 95%. If no such benefit were found, the overall benefit of ILM peeling would be highly improbable.
In summary, we showed that there might be a relationship between macular hole size and the benefit of ILM peeling. For macular hole diameters <400 μm, with a high success rate, no difference was found, whether the ILM was peeled off or not. ILM peeling may therefore be useful only for larger macular holes, for which the failure rate is higher.
Abbreviations
ICG - indocyanine green
ILM - internal limiting membrane
OCT - optical coherence tomography
Footnotes
Competing interests: None.
References
- 1.Paques M, Chastang C, Mathis A.et al Effect of autologous platelet concentrate in surgery for idiopathic macular hole: results of a multicenter, double‐masked, randomized trial. Platelets in Macular Hole Surgery Group. Ophthalmology 1999106932–938. [DOI] [PubMed] [Google Scholar]
- 2.Ullrich S, Haritoglou C, Gass C.et al Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol 200286390–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ip M S, Baker B J, Duker J S.et al Anatomical outcomes of surgery for idiopathic macular hole as determined by optical coherence tomography. Arch Ophthalmol 200212029–35. [DOI] [PubMed] [Google Scholar]
- 4.Haouchine B, Massin P, Gaudric A. Foveal pseudocyst as the first step in macular hole formation: a prospective study by optical coherence tomography. Ophthalmology 200110815–22. [DOI] [PubMed] [Google Scholar]
- 5.Brooks H L J. Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology 20001071939–1948. [DOI] [PubMed] [Google Scholar]
- 6.Eckardt C, Eckardt U, Groos S.et al Removal of the internal limiting membrane in macular holes. Clinical and morphological findings. Ophthalmologe 199794545–551. [DOI] [PubMed] [Google Scholar]
- 7.Mester V, Kuhn F. Internal limiting membrane removal in the management of full‐thickness macular holes. Am J Ophthalmol 2000129769–777. [DOI] [PubMed] [Google Scholar]
- 8.Ando F, Sasano K, Ohba N.et al Anatomic and visual outcomes after indocyanine green‐assisted peeling of the retinal internal limiting membrane in idiopathic macular hole surgery. Am J Ophthalmol 2004137609–614. [DOI] [PubMed] [Google Scholar]
- 9.Tadayoni R, Almeida C, Haouchine B.et al Macular hole size as a predictor of postoperative failure. Presented at the AAO Annual Meeting, 24 October 2004, New Orleans, USA
- 10.Wolf S, Schnurbusch U, Wiedemann P.et al Peeling of the basal membrane in the human retina: ultrastructural effects. Ophthalmology 2004111238–243. [DOI] [PubMed] [Google Scholar]
- 11.Nakamura T, Murata T, Hisatomi T.et al Ultrastructure of the vitreoretinal interface following the removal of the internal limiting membrane using indocyanine green. Curr Eye Res 200327395–399. [DOI] [PubMed] [Google Scholar]
- 12.Tadayoni R, Paques M, Massin P.et al Dissociated optic nerve fiber layer appearance of the fundus after idiopathic epiretinal membrane removal. Ophthalmology 20011082279–2283. [DOI] [PubMed] [Google Scholar]
- 13.Miura M, Elsner A E, Osako M.et al Dissociated optic nerve fiber layer appearance after internal limiting membrane peeling for idiopathic macular hole. Retina 200323561–563. [DOI] [PubMed] [Google Scholar]
- 14.Ito Y, Terasaki H, Takahashi A.et al Dissociated optic nerve fiber layer appearance after internal limiting membrane peeling for idiopathic macular holes. Ophthalmology 20051121415–1420. [DOI] [PubMed] [Google Scholar]
- 15.Mitamura Y, Ohtsuka K. Relationship of dissociated optic nerve fiber layer appearance to internal limiting membrane peeling. Ophthalmology 20051121766–1770. [DOI] [PubMed] [Google Scholar]
- 16.Terasaki H, Miyake Y, Nomura R.et al Focal macular ERGs in eyes after removal of macular ILM during macular hole surgery. Invest Ophthalmol Vis Sci 200142229–234. [PubMed] [Google Scholar]
- 17.Haritoglou C, Gass C A, Schaumberger M.et al Macular changes after peeling of the internal limiting membrane in macular hole surgery. Am J Ophthalmol 2001132363–368. [DOI] [PubMed] [Google Scholar]
- 18.Tadayoni R, Paques M, Girmens J F.et al Persistence of fundus fluorescence after use of indocyanine green for macular surgery. Ophthalmology 2003110604–608. [DOI] [PubMed] [Google Scholar]
- 19.Gass C A, Haritoglou C, Schaumberger M.et al Functional outcome of macular hole surgery with and without indocyanine green‐assisted peeling of the internal limiting membrane. Graefes Arch Clin Exp Ophthalmol 2003241716–720. [DOI] [PubMed] [Google Scholar]
- 20.Haritoglou C, Gandorfer A, Gass C A.et al Indocyanine green‐assisted peeling of the internal limiting membrane in macular hole surgery affects visual outcome: a clinicopathologic correlation. Am J Ophthalmol 2002134836–841. [DOI] [PubMed] [Google Scholar]
- 21.Horio N, Horiguchi M. Effect on visual outcome after macular hole surgery when staining the internal limiting membrane with indocyanine green dye. Arch Ophthalmol 2004122992–996. [DOI] [PubMed] [Google Scholar]