Abstract
Background
Recently, the entity of retinal angiomatous proliferation (RAP) as a subtype of exudative age‐related macular degeneration was described, but no treatment options have been established as yet. The only two therapeutic modalities being discussed are surgical lysis of the feeding arteriole and draining venule, and the use of photodynamic therapy combined with intravitreal triamcinolone injection.
Aim
To examine focal laser treatment of early extrafoveal intraretinal neovascularisation of RAP.
Methods
Prospective case series. We included 13 consecutive patients with an extrafoveal RAP stage I lesion. All patients underwent a complete ophthalmic examination, including fluorescein angiography and optical coherence tomography (OCT) III before treatment and at 2 weeks, 1, 2 and 4 months afterwards. In cases with marked macular oedema (>350 μm retinal thickening in OCT III, r = 12), intravitreal injection of 4 mg triamcinolone was given before focal laser treatment to reduce the oedema.
Results
This case series indicates anatomical improvement or stabilisation in patients with an extrafoveal RAP lesion after treatment. Initial visual acuity ranged from 0.1 to 0.6 on the Snellen chart. By calculating logarithmic values, visual acuity was seen to be improved in five cases (2 to 5 log lines), deteriorated in four cases (−2 to 5 log lines) and stabilised in four cases (−1 to +1 log line change). Exudation on fluorescein angiography was stopped in 11 cases.
Conclusions
This preliminary case series suggests laser photocoagulation combined with prior intravitreal triamcinolone injection as a viable treatment option for RAP stage I. In cases with marked macular oedema, intravitreal triamcinolone injection improved visual acuity. For long‐term stabilisation, additional laser treatment is mandatory. These preliminary results warrant a more detailed prospective clinical trial.
The entity of retinal angiomatous proliferation (RAP) as a subtype of age‐related macular degeneration (ARMD) was first described by Yannuzzi et al.1 This new type of neovascular lesion in ARMD does not originate from the choroid, but begins with intraretinal new vessels, extends to the subretinal space and eventually communicates with new choroidal vessels. Yannuzzi et al distinguished three different stages that indicate deep intraretinal capillary proliferation within the retina (intraretinal neovascularisation) as stage I. This is typically characterised by multiple small intraretinal haemorrhages and intraretinal oedema surrounding the core of proliferating capillaries. It also includes hard exudates as well as retinal–retinal anastomosis.
Stage II is classified as the extending of intraretinal neovascularisation beyond the photoreceptor layer into the subretinal space, and is called subretinal neovascularisation. It may be combined with a pigment epithelium detachment (PED). Stage III includes choroidal neovascularisation as well as retinal choroidal anastomosis (RCA).
Since then, few studies have evaluated therapeutic options for this new subtype of ARMD, and as yet there is no effective treatment. Surgical ablation of RAP has been described in a small number of patients with RAP stage II associated with serous PED,2 and it has been shown that visual acuity improved and macular thickening resolved. Other reports showed benefit from combined photodynamic therapy (PDT) with intravitreal triamcinolone in single cases.3,4 With regard to the late stages of RAP such as choroidal neovascularisation, RCA and associated PED, the unique conviction in the literature is a high risk for pigment epithelium tears caused by PDT.5 The effects of triamcinolone injection are limited and temporary. Recently, combined surgical ablation and intravitreal triamcinolone for RAP stage III has been reported.6 This treatment was safe and anatomically effective, but recurrence after surgical ablation has been described by another author.7
A literature search showed no studies evaluating treatment options for RAP stage I.
The purpose of this study was to determine the effects of laser photocoagulation in combination with prior triamcinolone injection on RAP stage I.
Materials and methods
We prospectively included 13 consecutive patients with RAP stage I at least in one eye. They were identified in the Ludwig‐Maximilians‐University Munich, ARMD outpatient clinic between October 2004 and May 2005 and showed typical signs of ARMD, including soft Drusen, retinal pigment epithelium changes or atrophy.
Patients were both male and female (3 men and 10 women); their age ranged from 61 to 95 years (average age 75 years). None of their eyes had received any treatment before inclusion into our study.
To be eligible, patients were required to have an extrafoveal RAP lesion stage I (⩾ 500 μm from the fovea), classified by clinical slit‐lamp biomicroscopy by one experienced examiner (MU), fluorescein angiography and optical coherence tomography (OCT) III. Other neovascular maculopathies such as pathological myopia, angioid streaks, inflammatory chorioretinal diseases, tumours or trauma were not included. Also excluded were late stages of RAP such as RCA or serous PED.
According to these criteria, 13 eyes of 13 patients were included. All patients underwent a complete ophthalmic examination, including fluorescein angiography and OCT III at 2 weeks, 1, 2 and 4 months afterwards. Angiography was carried out with a Heidelberg Retina Angiograph II (Heidelberg Engineering, Heidelberg, Germany) at 30 s, 1, 3 and 5.5 min after injection of 10 ml 10% fluorescein (Alcon, Texas, USA) into the cubital vein. In the case of marked macular oedema (>350 μm retinal thickening in OCT III, 12 of 13 cases), an intravitreal triamcinolone injection (4 mg) was given. The decision for laser treatment was based on the clinical findings and fluorescein angiography by one retinal specialist (MU). Photocoagulation was also carried out by one retinal specialist (MU) by means of a Humphrey Visulas 532 nm laser (Zeiss, Jena, Germany) and the “Area Centralis” lens (Volk, Mentor, Ohio) after a mean interval of 4 weeks. The number of spots applied varied from 9 to 36 (mean = 19 spots). The power was from 150 to 300 mW (mean = 266 mW), with a spot size of 200 μm. The exposure time varied from 200 to 300 ms.
Follow‐up visits were performed at 2 weeks after laser treatment and at 1, 2 and 4 months after the treatment. All follow‐up visits included best‐corrected visual acuity (BCVA) with a Snellen chart at 6 months, full clinical examination with slit‐lamp biomicroscopy, fluorescein angiography, optical coherence tomography and fundus photography. All examinations were also carried out on the fellow eye.
The main outcome measure was a change in visual acuity . Improvement was defined as a change in visual acuity from 2 to 5 log lines, stabilisation by change in visual acuity from −1 to +1 log line, and deterioration was classified as a loss of −2 to −5 log lines.
Additionally, angiographic exudation was analysed.
Results
In one case, laser photocoagulation had to be repeated to achieve complete cessation of exudation and stabilisation of visual acuity. Another case showed persistent exudation and leakage, with extension into the subfoveal area. In this case, PDT was successfully carried out.
One patient underwent intravitreal triamcinolone injection and PDT on the fellow eye for advanced RAP.
Another case showed rapid deterioration in the fellow eye, which progressed from RAP stage I to III during the period of review.
During the period of review, only one study eye progressed to RAP stage III. The other eyes with deterioration in visual acuity, nevertheless, showed stabilised angiographic findings.
There were no complications related to intravitreal injection or laser treatment.
Visual acuity
This study showed visual improvement in six patients. In four patients, visual acuity remained unchanged and three patients showed deterioration. At baseline, BCVA ranged from logarithm of minimum angle of resolution (log MAR) 1 to log MAR 0.2 (decimal equivalent 0.1–0.6 Snellen scale). At the 1‐month and 4‐month visits the BCVA ranged from log MAR 1.3 to log MAR 0.2, whereas the average BCVA changed from log MAR 0.65 to log MAR 0.6 at the 1‐month visit and to log MAR 0.54 at the 4‐month visit (fig 1).
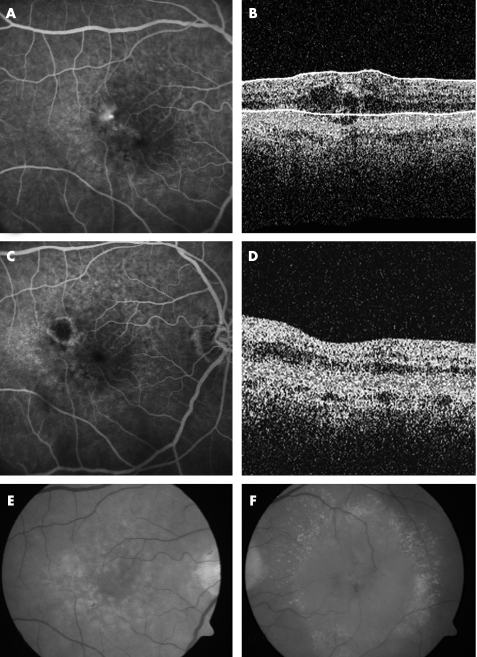
Figure 1 (A–D) Case 2: A 76‐year‐old woman with retinal angiomatous proliferation (RAP) stage I with extrafoveal leakage in the right eye. Visual acuity was 0.3 (logarithm of minimum angle of resolution (logMAR) 0.5). (A, B) Angiography as well as optical coherence tomography (OCT) findings showed extrafoveal leakage in combination with intraretinal oedema. Clinically, we found superficial intraretinal haemorrhages and hard exudates. (C, D) Findings 4 months after intravitreal injection of triamcinolone and consecutive laser treatment. The visual acuity changed from 0.3 to 1.0 (log MAR 0). There was no exudation in fluorescein angiography and no intraretinal oedema on OCT. (E) Fundus photography of treated RAP stage I lesion after 4 months. (F) Fellow eye with RAP stage III.
The BCVA improved in six patients (46%) by 2–8 log lines (average gain in this group was 3.8 log lines, decimal equivalent 0.2–1.0 Snellen chart). The BCVA stabilised in four patients (31%) (no log line change in visual acuity, decimal equivalent 0.2–0.6 Snellen chart). In three patients (23%) the BCVA decreased by 2–5 log lines ( average loss in this group was 3.6 log lines, decimal equivalent 0.05–0.1 Snellen chart (table 1).
Table 1 Visual acuity (logarithm of minimum angle of resolution units) of patients with retinal angiomatous proliferation stage I who underwent combined triamcinolone injection and laser photocoagulation.
| Patient number | Age | Baseline VA (log MAR) | VA 2 weeks (log MAR) | VA 1 month (log MAR) | VA 2 months (log MAR) | Final VA 4 months (log MAR) | Total VA change in loglines | Complication |
|---|---|---|---|---|---|---|---|---|
| 1 | 82 | 1 | 1 | 1 | 0.4 | 0.7 | 3 | RAP stage I of fellow eye |
| 2 | 76 | 0.5 | 0 | 0 | 0 | 0 | 5 | |
| 3 | 74 | 0.7 | 0.7 | 0.7 | 0.7 | 0.7 | 0 | |
| 4 | 80 | 1 | 0.9 | 1.3 | 1.3 | 1.3 | −3 | |
| 5 | 76 | 0.7 | 1 | 1 | 1 | 1 | −3 | |
| 6 | 61 | 1 | 0.3 | 0.4 | 0.2 | 0.2 | 8 | |
| 7 | 66 | 0.7 | 0.4 | 0.4 | 0.4 | 0.4 | 3 | |
| 8 | 63 | 0.5 | 0.7 | 1 | 0.8 | 1 | −5 | PDT 1 |
| 9 | 72 | 0.8 | 1 | 0.6 | 2 | |||
| 10 | 71 | 0.2 | 0.2 | 0.2 | 0.3 | 0.2 | 0 | |
| 11 | 78 | 0.5 | 0.4 | 0.3 | 0.2 | 0.3 | 2 | |
| 12 | 87 | 0.3 | 0.4 | 0.3 | 0.4 | 0.2 | 1 | IVTA 2 |
| 13 | 95 | 0.6 | 0.5 | 0.7 | 0.5 | −1 | ||
| Mean | 0.65 | 0.57 | 0.6 | 0.57 | 0.54 |
The table also includes the age of the patients and complications, as well as eventual further additional treatment.
IVTA, intravitreal triamcinolone; MAR, minimum angle of resolution; PDT, photodynamic therapy; RAP, retinal angiomatous proliferation; VA, visual acuity.
Fluorescein angiography findings
Exudation on fluorescein angiography was completely stopped in 11 of 13 (85%) eyes at the 4‐month visit. Even in the group with deterioration of visual acuity, we observed stable angiographic findings.
In one eye with unchanged BCVA, angiographic extension of neovascularisation to the subfoveal area was noted. In this case, additional PDT was successful and the visual acuity stabilised.
Another patient showed recurrent exudation at the edge of the laser scar with intraretinal oedema at the 4‐month visit. Additional intravitreal triamcinolone injection and photocoagulation were scheduled in this case.
Fellow eyes
The study eyes with treated RAP stage I lesion had better function in 8 (62%) eyes compared with their fellow eyes. The fellow eyes had either RAP lesions (stage II or III) or a fibrovascular scar (table 2).
Table 2 Fellow eyes of patients under study and clinical stage of age‐related macular degeneration.
| Clinical stage of ARMD | Number of eyes |
|---|---|
| ARMD with mild Drusen | 5 |
| RAP stage II or III | 3 |
| FVS | 2 |
| CRA | 3 |
ARMD, age‐related macular degeneration; CRA, chorioretinal atrophy; FVS, fibrovascular scar; RAP, retinal angiomatous proliferation.
Discussion
This study presents a novel treatment option in retinal angiomatous proliferation stage I. As the neovascular origin of the lesion is in the deep intraretinal vascular plexus, photocoagulation of extrafoveal lesions was carried out to prevent progression to RAP stage II or III.1 This led to stabilisation or improvement of visual acuity and stable angiographic findings in most of the eyes.
Thermal laser photocoagulation has been considered unfavourable with poor visual outcome previously because it does not spare retinal pigment epithelium.2 Especially in eyes with associated PED, studies suggest little benefit.8,9,10
Only one case reported laser treatment for RAP with cilioretinal artery anastomosis.11 However, since the specific classification of RAP into different stages, there have been no further trials that evaluated conventional laser photocoagulation as a treatment option for extrafoveal stage I RAP lesions. However, the therapeutic gold standard for small extrafoveal classic choroidal neovascularisation is thermal photocoagulation.12
According to the results of this preliminary study, early detection and treatment of RAP stage I are recommended, and a high level of visual acuity and quality of life can be sustained.
Early detection is of most importance. These patients rarely had distortion, and as the RAP tends to form in an extrafoveal part of the macular area, only a mild decrease in visual acuity was reported. Presentation in the clinic is usually because of a RAP stage II or III lesion in the fellow eye. Yannuzzi et al1 observed RAP lesions to be bilateral. They begin with small intraretinal, extrafoveal new vessels. Therefore it is mandatory to examine the fellow eye for early changes.
We do acknowledge that our study presents only a small number of patients and has a limited period of review. Nevertheless, it was shown that extrafoveal RAP stage I can benefit from combined treatment with intravitreal triamcinolone and thermal laser photocoagulation. This justifies a more detailed and prospective clinical trial. The treatment of RAP stage I may prevent the progression to RAP stage II and III for some time.
Abbreviations
ARMD - age‐related macular degeneration
BCVA - best‐corrected visual acuity
CRA - chorioretinal atrophy
FVS - fibrovascular scar
IVTA - intravitreal triamcinolone
MAR - minimum angle of resolution
OCT - optical coherence tomography
PDT - photodynamic therapy
PED - pigment epithelium detachment
RAP - retinal angiomatous proliferation
RCA - retinal choroidal anastomosis
Footnotes
Competing interests: None declared.
Presented in part at the Société Francaise d̀ Ophthalmologie meeting, May 2005, Paris, France and the joint meeting of 103rd DOG Congress/15th SOE Congress, September 2005, Berlin, Germany.
References
- 1.Yannuzzi L A, Negrao S, Iida T.et al Retinal angiomatous proliferation in age‐related macular degeneration. Retina 200121416–434. [DOI] [PubMed] [Google Scholar]
- 2.Borrillo J L, Sivalingam A, Martidis A.et al Surgical ablation of retinal angiomatous proliferation. Arch Ophthalmol 2003121558–561. [DOI] [PubMed] [Google Scholar]
- 3.Bottoni F, Romano M, Massacesi A.et al Remodeling of the vascular channels in retinal angiomatous proliferations treated with triamcinolone acetonide and photodynamic therapy. Graefe's Arch Clin Exp Ophthalmol. 2006. Epub ahead of print [DOI] [PubMed]
- 4.Hunter M A, Dunbar M T, Rosenfeld P J. Retinal angiomatous proliferation: clinical characteristics and treatment options. Optometry 200475577–588. [DOI] [PubMed] [Google Scholar]
- 5.Pece A, Introini U, Botttoni F.et al Acute retinal pigment epithelium tear after photodynamic therapy. Retina 200121661–665. [DOI] [PubMed] [Google Scholar]
- 6.Boscia F, Furino C, Prascina F.et al Combined surgical ablation and intravitreal triamcinolone acetonide for retinal angiomatous proliferation. Eur J Ophthalmol 200515513–516. [DOI] [PubMed] [Google Scholar]
- 7.Sakimoto S, Gomi F, Sakaguchi H.et al Recurrent retinal angiomatous proliferation after surgical ablation. Am J Ophthalmol 2005139917–918. [DOI] [PubMed] [Google Scholar]
- 8.Hartnett M E, Weiter J J, Staurenghi G.et al Deep retinal vascular anomalous complexes in advanced age‐related macular degeneration. Ophthalmology 19961032042–2053. [DOI] [PubMed] [Google Scholar]
- 9.Slakter J S, Yannuzzi L A, Schneider U.et al Retinal choroidal anastomoses and occult choroidal neovascularisation in age‐related macular degeneration. Ophthalmology 2000107742–753. [DOI] [PubMed] [Google Scholar]
- 10.Kuhn D, Meunier I, Soubrane G.et al Imaging of chorioretinal anastomoses in vascularized retinal pigment epithelium detachments. Arch Ophthalmol 19951131392–1398. [DOI] [PubMed] [Google Scholar]
- 11.Ghazi N G, Conway B P. Retinal angiomatous proliferation with a cilioretinal artery anastomosis: an unusual presentation. Graefe's Arch Clin Exp Ophthalmol 2005243493–496. [DOI] [PubMed] [Google Scholar]
- 12.Ulbig M W, Mc Hugh D A, Hamilton A M P. Photocoagulation of choroidal neovascular membranes with a diode laser. Br J Ophthalmol 199377218–221. [DOI] [PMC free article] [PubMed] [Google Scholar]