Abstract
Aim
To identify whether the risk of an intraoperative complication of phakoemulsification cataract surgery increases with age.
Methods
1441 consecutive patients undergoing phakoemulsification cataract surgery were assessed preoperatively, and data on the occurrence of intraoperative complications were collected prospectively. Data were entered into a computerised database, and logistic regression was used to examine evidence of an association between age and the risk of an intraoperative complication. In addition, the rates of intraoperative complications were compared between patients ⩾88 years and those <88 years, and between patients ⩾96 years and those <96 years.
Results
No significant association was found between age and the risk of an intraoperative complication. The authors found little evidence that patients ⩾88 years were at a greater risk of an intraoperative complication than those <88 years, or that those ⩾96 years are at increased risk; however, numbers were small.
Conclusions
These results suggest that age alone is not a major risk factor for any intraoperative complications occurring during phakoemulsification cataract surgery. This has implications not just for tailoring the risk of complications occurring to individual patients but also for meaningful comparisons between national complication rates and those of individual surgeons, and better selection of cases suitable for instruction.
In an effort to improve the safety of cataract surgery, numerous groups have attempted to establish whether certain factors evident at preoperative assessment might be useful predictors of an intraoperative complication. Among the eyes shown to be at risk of a visually relevant complication at the time of surgery are those with a white or dense cataract,1,2,3 vitrectomised eyes,4,5 those with pseudoexfoliation,6 those with posterior polar cataracts7,8 and those with shallow anterior chambers.9 In addition, Berler10 found that those ⩾88 years were at increased risk of complications compared with those <88 years, in a study of 802 consecutive cataract operations. Syam et al11 conducted a retrospective study of perioperative complications of cataract surgery in those ⩾96 years, which suggested a higher incidence of complications in this age group, although numbers were small (34 eyes of 21 patients). We undertook a study examining the hypothesis that age is a risk factor for cataract surgery complications.
Methods
The approval of the ethics review board of our hospital was sought and obtained.
We conducted a Medline review of the literature pertaining to complications during phakoemulsification cataract surgery, particularly with a view to identifying those studies looking at age as a risk factor. We found one study that claimed intraoperative complications, such as posterior capsular tears, vitreous loss and loss of nucleus, in 10% of patients aged ⩾88 years compared with only 3% in patients <88 years.10
We used our literature search to draw up a data sheet, which was attached to the case notes at the preoperative ward round. Once the operation had been completed, data regarding date of surgery, right eye or left eye, grade of surgeon and whether any complication had occurred were recorded on the sheet. In the event of any complication occurring, its nature was specified as follows: incomplete capsulorrhexis, posterior capsule rupture, vitreous loss, zonule dehiscence, lost nucleus, anterior capsule tear, unplanned extracapsular cataract extraction, corneal burn or wound leak, others (“specify”). We used a preoperative data collection sheet and maintained patient/surgeon anonymity throughout, with the aim of minimising reporting bias.
When all the required data had been entered, the data sheet was detached and placed in a designated receptacle in the operating theatre after each operation. The data were entered into a computerised database (Microsoft Access 2000).
To examine whether age was a risk factor for complications, logistic regression was used. In addition to this, as previous papers had suggested that patients ⩾88 years and ⩾96 years might be useful cut‐offs, we compared the overall complication rates between those more than and less than these ages. For descriptive purposes, we report overall complication rates (table 1), with 95% confidence intervals in five age groups (<50, 50–60, 60–70, 70–80 and >90 years).
Table 1 Overall complication rates per age group.
| Age group (years) | Complication at surgery | |||
|---|---|---|---|---|
| Yes | No | Total | Percentage (95% CI) | |
| ⩽50 | 1 | 28 | 29 | 3.45 (0.087 to 17.77) |
| 50–60 | 5 | 74 | 79 | 6.33 (2.09 to 14.15) |
| 60–70 | 18 | 269 | 287 | 6.27 (3.76 to 9.73) |
| 70–80 | 37 | 510 | 547 | 6.76 (4.81 to 9.20) |
| 80–90 | 28 | 417 | 445 | 6.29 (4.22 to 8.97) |
| >90 | 3 | 51 | 54 | 5.56 (1.16 to 15.39) |
| Total | 92 | 1349 | 1441 | 6.38 (5.18 to 7.77) |
CI, confidence interval
We collected data only from successive phakoemulsification operations. Planned extracapsular cataract extractions were not included in the study. All operations included placement of an injectable hydrophilic or hydrophobic acrylic intraocular lens or a foldable silicone intraocular lens in the bag, except where a complication necessitated placement of a lens in the posterior sulcus or anterior chamber. A mixture of types of anaesthesia was used depending on the preference of the surgeon and attending anaesthetist. These included topical, sub‐Tenon's and peribulbar anaesthesia, as well as occasional general anaesthesia.
To negate the effect of a higher rate of complications by inexperienced surgeons, we only included data from operations performed by consultants, fellows and specialist registrars.
Results
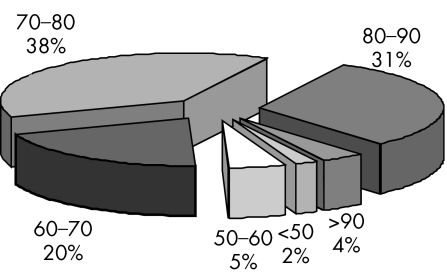
We analysed data on 1441 patients with cataract who had surgery between 15 November 2002 and 9 June 2003. Surgery was performed on 533 men (mean age 73.7 years) and 908 women (mean age 75.9 years). The overall complication rate (6.38% locally compared with 7.5% nationally12) compared favourably with the results of the National Cataract Survey, which adopted less comprehensive criteria. Numbers of patients were spread fairly evenly across the 60–90 age range (fig 1). We found no evidence for an association between the risk of a complication and whether or not the surgeon was still in training, and we therefore did not adjust for this (odds ratio (OR) 1.1, 95% confidence interval (CI) 0.67 to 1.81).
Figure 1 Age groups (years) represented as a percentage of the total number of patients (n = 1441).
We found little evidence of any association between age and the odds of a complication (OR 1.003, 95% CI 0.98 to 1.02). Complication rates in patients ⩾88 years (4.5%) were similar to those ⩽88 years (6.3%); p = 0.54. Complication rates were higher in patients ⩾96 (11.1%) years than in patients <96 (6.3%) years, but this was not significant; p = 0.45. It should be noted, however, that the power to detect a difference here was low, as there were only nine patients in our study ⩾96 years. Further analysis of specific complication rates showed that none of the individual complications examined, including visually relevant complications (posterior capsular rupture, vitreous loss, dropped nucleus), occurred with greater frequency in any particular age group.
Conclusions
We found little evidence to support the hypothesis that age alone is a risk factor for the intraoperative complications of phakoemulsification cataract surgery. This contrasts with the results of the only other comparable study published on the subject, which suggested that people >88 years were at increased risk of complications.10 Syam et al11 found complication rates in 34 eyes (of 21 patients) ⩾96 years: anterior capsular tear, 8.8%; zonular dialysis with vitreous loss, 2.9%; posterior capsule rupture with vitreous loss, 2.9%; iris incarceration, 5.9%. Our study included nine patients aged ⩾96 years, one of whom had a posterior capsule rupture.
These results provide evidence that no patient should be denied the benefits of cataract surgery on the basis of age. Elderly people often seem most resistant to the idea of surgery (possibly because of a greater fear of complications occurring); these results allow us to provide patients with greater accuracy of reslts and, more specifically, reassure elderly patients that they are not at increased risk of complications simply because of their age. The evidence that the very old stand to benefit from cataract surgery is clear: Evans et al13 established that a substantial proportion of visual impairment in a sample of older people in Britain could be attributed to remediable causes, including cataract (cataract being responsible for visual loss of 6/18 or worse in 35.9% of patients aged 75 years in a population of 976); Brannan et al14 established that cataract surgery is an effective intervention to reduce the risk of falls in elderly patients with cataract‐related visual impairment. Interestingly, however, Westcott et al15 found that age is a significant determinant of visual outcome, with the odds of a patient with no comorbidity achieving an acuity of ⩾6/12 being 4.6 times higher in the 60–69‐year age group than in those >80 years (in addition, Berler10 found that, in patients <88 years, 90.5% of eyes with complicated surgery achieved an acuity ⩾6/12 compared with only 40% in complicated cases where the patient was >88 years).
With increasing pressures on departments to compare performance internally and externally, our results suggest that the age of a population undergoing cataract surgery should have little bearing on intraoperative complication rates, allowing a more focused appraisal of performance both locally and nationally. In addition, this study suggests that patient's age should not determine suitability for training purposes, although clearly dense cataracts occur with greater frequency with age, and this, together with other risk factors, might influence whether a case would be appropriate for a trainee surgeon.
Recent work by Osborne et al16 has successfully validated two scoring systems for predicting the likelihood of a complication.17,18 The evidence‐based scoring system developed by Muhtaseb et al17 apportions a level of risk to those >88 years—revision in the light of our findings may improve the accuracy of this particular method. Indeed, all such scoring systems would clearly benefit from further research into the weight accorded to certain individual risk factors.
We hope that the findings of this study will contribute to the body of research aimed at delivering patients with more informed consent, and surgeons with both the means to compare outcomes more accurately and train juniors more effectively.
Footnotes
Competing interests: None declared.
References
- 1.Chakrabarti A, Singh S. Phacoemulsification in eyes with white cataract. J Cataract Refract Surg 2000261041–1047. [DOI] [PubMed] [Google Scholar]
- 2.Brazitikos P D, Tsinopoulos I T, Papadopoulos N T.et al Ultrasonographic classification and phacoemulsification of white senile cataracts. Ophthalmology 19991062178–2183. [DOI] [PubMed] [Google Scholar]
- 3.Singh R, Vasavada A R, Janaswamy G. Phacoemulsification of brunescent and black cataracts. J Cataract Refract Surg 2001271762–1769. [DOI] [PubMed] [Google Scholar]
- 4.Pinter S M, Sugar A. Phacoemulsification in eyes with past pars plana vitrectomy: case‐control study. J Cataract Refract Surg 199925556–561. [DOI] [PubMed] [Google Scholar]
- 5.Diaz Lacalle V, Orbegozo Garate F J, Martinez Alday N.et al Phacoemulsification cataract surgery in vitrectomized eyes. J Cataract Refract Surg 199824806–809. [DOI] [PubMed] [Google Scholar]
- 6.Drolsum L, Haaskjold E, Sandvig K. Phacoemulsification in eyes with pseudoexfoliation. J Cataract Refract Surg 199824787–792. [DOI] [PubMed] [Google Scholar]
- 7.Vasavada A, Singh R. Phakoemulsification in eyes with posterior polar cataract. J Cataract Refract Surg 199925238–245. [DOI] [PubMed] [Google Scholar]
- 8.Osher R H, Yu B C, Koch D D. Posterior polar cataracts: a predisposition to intraoperative posterior capsular rupture. J Cataract Refract Surg 199016157–162. [DOI] [PubMed] [Google Scholar]
- 9.Kuchle M, Viestenz A, Martus P.et al Anterior chamber depth and complications during cataract surgery in eyes with pseudoexfoliation syndrome. Am J Ophthalmol 2000129281–285. [DOI] [PubMed] [Google Scholar]
- 10.Berler D K. Intraoperative complications during cataract surgery in the very old. Trans Am Ophthalmol Soc. 2000;98: 127–30; discussion 130–2, [PMC free article] [PubMed]
- 11.Syam P P, Eleftheriadis H, Casswell A G.et al Clinical outcome following cataract surgery in very elderly patients. Eye 20041859–62. [DOI] [PubMed] [Google Scholar]
- 12.Desai P, Minassian D C, Reidy A. National cataract surgery survey 1997–8: a report of the results of the clinical outcomes. Br J Ophthalmol 1999831336–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Evans J R, Fletcher A E, Wormald R P. Causes of visual impairment in people aged 75 years and older in Britain: an add‐on study to the MRC Trial of Assessment and Management of Older People in the Community. Br J Ophthalmol 200488365–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brannan S, Dewar C, Sen J.et al A prospective study of the rate of falls before and after cataract surgery. Br J Ophthalmol 200387560–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Westcott M C, Tuft S J, Minassian D C. Effect of age on visual outcome following cataract extraction. Br J Ophthalmol 2000841380–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Osborne S A, Adams W E, Bunce C V.et al Validation of two scoring systems for the prediction of posterior capsule rupture during phacoemulsification surgery. Br J Ophthalmol 200690333–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muhtaseb M, Kalhoro A, Ionides A. A system for preoperative stratification of cataract patients according to risk of intraoperative complications: a prospective analysis of 1441 cases. Br J Ophthalmol 2004881242–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Habib M S, Bunce C V, Fraser S G. The role of case mix in the relation of volume and outcome in phacoemulsification. Br J Ophthalmol 2005891143–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]