Abstract
Aim
To compare the following two methods of paediatric secondary posterior chamber intraocular lens (PCIOL) determination with the Holladay formula: (1) estimation from the aphakic refraction alone (using assumed keratometry (K) of 44 diopters); and (2) calculation based on preoperative measured biometry.
Methods
(1) Retrospective medical record review in a referral eye hospital of children with aphakia aged ⩽12 years who underwent secondary PCIOL implantation with an Alcon MA60BM lens; (2) PCIOL determination for a plano refraction by the above two methods (estimation and calculation); and (3) prediction of pseudophakic refraction for the PCIOL actually implanted by the above two methods compared with the actual pseudophakic refraction.
Results
50 eyes of 30 children with aphakia were studied. The estimated (mean, 95% confidence interval (CI)) secondary PCIOL values (25.81, ±1.65 D) and the calculated secondary PCIOL values (26.35, ±1.50 D) were not significantly different (mean absolute value of the difference 1.86 D, 95% CI ±0.41 D) by the two‐tailed paired t test at α = 0.05 (p = 0.11). For each eye, the pseudophakic refractions predicted by the two methods for the PCIOL that was actually implanted differed, both from each other and from the actual pseudophakic refraction (repeated‐measures analysis of variance, p<0.001; Tukey test, p<0.01).
Conclusions
The method of PCIOL estimation from the aphakic refraction alone provides values similar to those obtained by a standard technique and can be useful if biometry is unavailable. Targeting a pseudophakic refraction in paediatric aphakia is prone to error.
Calculation of power of the secondary posterior chamber intraocular lens (PCIOL) by standard biometry is more prone to error in children than in adults, with actual postoperative paediatric pseudophakic refractions sometimes many diopters (D) different from preoperative targets.1,2 Standard biometry (ie, keratometry (K values) and ultrasonic axial length measurement) is currently the only practical way to measure the variables needed for PCIOL prediction formulas. In eyes with aphakia, however, power of the secondary PCIOL can be estimated from PCIOL prediction formulas in the absence of standard biometry in the following manner: axial length can be calculated from the aphakic refraction,3,4,5,6,7,8,9 and keratometry values can be assumed as an average value (because the effect of varying keratometry values on predicted pseudophakic refraction is small if an eye's aphakic refraction is known7). The purpose of this study is to compare and evaluate the following two methods of determination of paediatric secondary PCIOL using the Holladay formula10: (1) estimation with axial length estimated from the aphakic refraction (using a standard keratometry value) and (2) calculation based on measured preoperative biometry.
Methods
Institutional review board approved the study. Charts of children aged ⩽12 years with aphakia who underwent secondary PCIOL implantation of an Acrosott© MA60BM three‐piece acrylic PCIOL (Alcon, Fort Worth, Texas) and had a pseudophakic refraction within 6 months after surgery were reviewed. Data collected for each eye included aphakic refraction, ultrasonic axial length, average keratometry reading, patient's age at the time of refraction and biometry, PCIOL implanted and the first pseudophakic refraction. Technicians experienced in biometry measured ultrasonic axial length and keratometry values; these measurements were made under anaesthesia for young children and those with poor fixation. The Nidek Ultrasound 3300 or Coopervision Ultrascan 404 was used for axial length measurement using the machine's aphakic setting. The Haag–Streit keratometer was used for keratometry measurements. Retinoscopies were carried out by experienced paediatric ophthalmologists; chloral hydrate sedation was used on young uncooperative children (under five years of age) if necessary.
The axial length of each eye was estimated from its aphakic refraction (spherical equivalent) using a method described previously7,9 as follows:
R (aphakic refraction) = spherical equivalent value from patient chart
K (average keratometry) = 44 D (arbitrarily assumed)
VTX (vertex distance) = 0.010 m (arbitrarily assumed)
nc (corneal index of refraction) = 1.376
na (aqueous index of refraction) = 1.336
TC (thickness of the cornea in metres)11 = 0.0006
RcA (anterior corneal radius in metres) = 0.3375/K
RcP (posterior corneal radius in metres) = RcA−0.0009
PFAC (diopters in front of the anterior cornea) = 1/((1/R)−VTX)
PBAC (diopters behind the anterior cornea) = PFAC+((nc−1)/RcA)
PFPC (diopters in front of the posterior cornea) = nc/((nc/PBAC)−TC)
PBPC (diopters behind the posterior cornea) = PFPC+((na−nc)/RcP)
AL (axial length in millimetres) = (na/PBPC)+TC
The estimated axial length was used in the Holladay formula with an arbitrary keratometry value of 44 D and the recommended Alcon MA60BM PCIOL surgeon factor of 1.73 to predict power of the secondary PCIOL for emmetropia, thus simulating a situation in which biometry was unavailable. In addition, the Holladay formula was used in a standard manner to calculate power of the secondary PCIOL for emmetropia for each eye (using ultrasonic axial length value, preoperative biometric average keratometry readings and the Alcon MA60BM PCIOL surgeon factor of 1.73). For each eye, the two secondary PCIOL values (estimated and calculated values) were compared.
The two methods for PCIOL prediction (estimation and calculation) were then used to predict the expected pseudophakic refraction for in‐the‐bag placement of the PCIOL actually implanted. All PCIOLs were actually placed in the sulcus; therefore, to compare sulcus placements, +0.52 D was subtracted from each expected pseudophakic refraction to obtain the predicted pseudophakic refraction for the sulcus placement12 before comparison with the actual pseudophakic refraction.
Calculations using the Holladay formula were made using software on the Humphrey A/B Scan System Model 837. Microsoft Excel V.2003 was used for statistical analysis of the data (the two‐tailed paired t test at α = 0.05, Pearson's correlation coefficient, averages, differences and 95% CI). For repeated‐measures analysis of variance and the Tukey test, an online statistical package was used (http://faculty.vassar.edu/lowry/corr3.html, accessed 15 July 2006).
Results
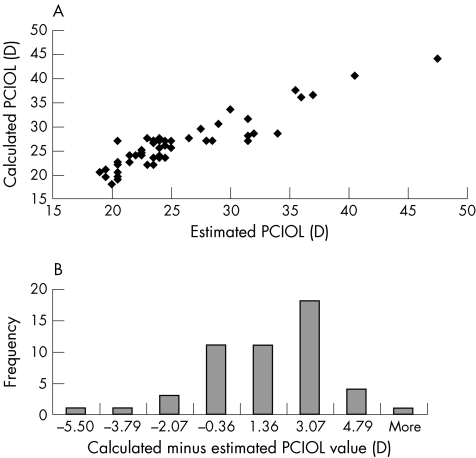
We identified 50 eyes of 30 patients. For each eye, preoperative biometry and aphakic refraction were carried out within 3 months of PCIOL insertion; all PCIOLs were placed in the ciliary sulcus. No patient had evidence for aphakic glaucoma during the study period. The mean (range, standard deviation (SD)) age of the patients was 7.89 years (6 months to 12 years, 2.81 years). The mean (range, SD) aphakic refraction was 14.68 (11–25, 3.07) D. The (mean, 95% CI) estimated secondary PCIOL values (25.81 D, ±1.65 D) and the calculated secondary PCIOL values (26.35 D, ±1.50 D) were positively correlated (Pearson's correlation coefficient 0.92) and had a mean difference (in absolute values) of 1.86 D (95% CI ±0.41 D). The two‐tailed paired t test showed no significant difference (p = 0.11) between the two predicted PCIOL values at α = 0.05 (t = 1.64), whereas the critical two‐tailed t value was 2.01 for α = 0.05. The maximum difference was 6.5 D, the minimum difference was 0 D and the SD of the differences was 1.49 (fig 1).
Figure 1 (A) Calculated and estimated posterior chamber intraocular lens (PCIOL) values were positively correlated. (B) A histogram of the differences between the calculated and estimated PCIOL values shows that calculated values tended to be larger. Although the paired t test suggested that the two values did not differ significantly as groups, individual values differed by as much as 6.5 D (“More”). It is not clear which PCIOL value was more accurate because neither PCIOL was actually implanted in a given eye.
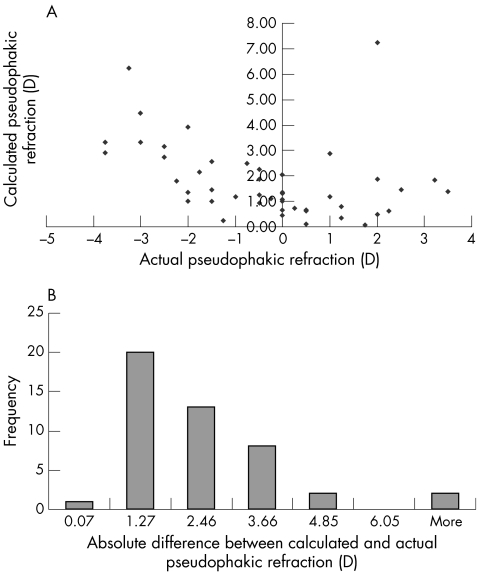
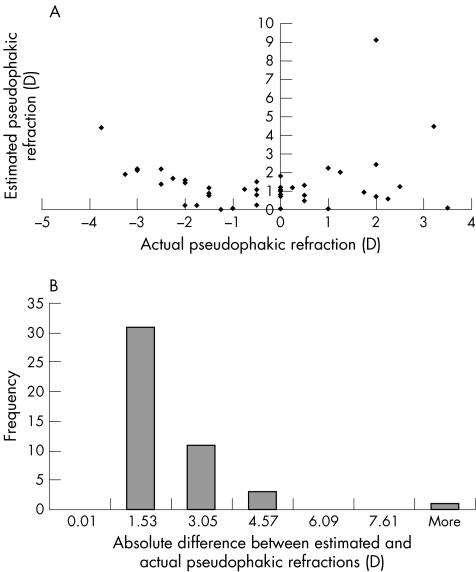
Postoperative pseudophakic refractions were analysed in 46 eyes; four of the 50 eyes were excluded because postoperative pseudophakic refraction was not documented in the medical record. A comparison of the expected pseudophakic refraction predicted by each of the two methods for sulcus placement of the PCIOL actually implanted with the actual pseudophakic refraction showed that the three values were not the same (repeated‐measures analysis of variance, F = 20.76, p<0.001). In addition, the Tukey test showed that no two of these three groups were the same (p<0.01). Although expected pseudophakic refractions predicted by each of the two methods differed from actual pseudophakic refractions, the expected values predicted by the estimation method as a group seemed closer to the actual pseudophakic refractions (average absolute value of the difference 1.48 D) than those predicted by the calculation method (average absolute value of the difference 1.80 D; figs 2, 3).
Figure 2 (A) Actual pseudophakic refractions plotted against calculated pseudophakic refractions; the two values were not similar by the Tukey test. (B) The absolute values of the differences between the actual pseudophakic refraction and the calculated pseudophakic refraction. As a group, there tended to be more difference from the actual pseudophakic refraction for the calculated values than for the estimated values (fig 3). “More” refers to the values 6.22 and 7.24 D.
Figure 3 (A) Actual pseudophakic refractions plotted against estimated pseudophakic refractions; the two values were not similar by the Tukey test. (B) The absolute values of the differences between the actual pseudophakic refraction and the estimated pseudophakic refraction. As a group there tended to be less difference from the actual pseudophakic refraction than was the case for calculated values (fig 2). “More” refers to the value 9.13 D.
Discussion
In this series of 50 eyes of children with aphakia, we overall found no marked difference between predicted values for secondary PCIOL power (for a plano refraction) when calculated from a standard biometry‐based method and when estimated from the aphakic refraction alone with an arbitrary keratometry value. Differences between the two values ranged up to 6.5 D; however, as none of the eyes were actually implanted with either predicted PCIOL, a judgement cannot be made as to which value was more appropriate.
Both techniques are prone to measurement error in eyes of children with aphakia, largely because of inaccuracies in axial length determination. In the estimation technique, axial lengths were estimated from refractions that usually could not be subjectively refined, and were based on an assumed vertex distance. In addition, the assumption of assumed keratometry in this technique, although not a major factor for most patients, would be expected to introduce error when actual keratometry is very flat or steep.7,8 The calculation technique for power determination in paediatric secondary PCIOL implantation is also prone to measurement error. Paediatric outpatient axial length measurements are obviously limited by the maturity of the child. When carried out under anaesthesia, axial length measurements are prone to error because they are made without the guidance of a fixating patient (the immersion ultrasound technique would have improved axial length measurement accuracy, but this was not the practice at the King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia). The lack of a lens spike in patients with aphakia makes verification of the visual axis even more difficult. Further complicating ultrasonic axial length measurements in children are biomechanics that differ those in adults, such as increased corneal elasticity (and thus increased potential for corneal compression), differing ocular tissue viscosity (potentially resulting in an actual speed of sound different from what is assumed by the ultrasound unit)1,2 and ocular dimensions that do not correspond to the adult dimensions assumed by theoretical PCIOL formulas.
This retrospective study cannot determine which of the two methods for paediatric secondary PCIOL prediction is more accurate for multiple reasons that include lack of target refraction documentation preoperatively and variation in patient follow‐up visits. However, an attempt was made to evaluate which method was more accurate in the following manner: the two methods were used to estimate the expected pseudophakic refraction for sulcus placement of the PCIOL actually implanted and then compared with each other as well as with the actual pseudophakic refraction. These comparisons showed that the three values differed. Interestingly, in this sample, predicted pseudophakic refractions by the estimation method (with an average absolute difference of 1.48 D from the actual pseudophakic refraction) as a group tended to be closer to the actual pseudophakic refraction than values predicted by the standard biometry‐based method (with an average difference of 1.80 D from the actual pseudophakic refraction; figs 2, 3).
In summary, prediction of pseudophakic refraction in children before secondary PCIOL implantation is prone to error. Estimation of paediatric secondary PCIOL power for a plano refraction from the aphakic refraction provides values similar to those obtained by a standard biometry‐based technique. This estimation method can be useful, especially in settings where biometry is unavailable.
Abbreviations
PCIOL - posterior chamber intraocular lens
Footnotes
Competing interests: None.
The Human Ethics Committee and Institutional Review Board of the King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia, approved this study.
References
- 1.Mezer E, Rootman D S, Abdolell M.et al Early postoperative refractive outcomes of pediatric intraocular lens implantation. J Cataract Refract Surg 200430603–610. [DOI] [PubMed] [Google Scholar]
- 2.Andreo L K, Wilson M E, Sauders R A. Predictive value of regression and theoretical IOL formulas in pediatric intraocular lens implantation. J Pediatr Ophthalmol Strabismus 199734240–243. [DOI] [PubMed] [Google Scholar]
- 3.Weinstein G W, Baum G, Binkhorst R D.et al A comparison of ultrasonographic and optical methods for determining the axial length of the aphakic eye. Am J Ophthalmol 1966621194–1201. [DOI] [PubMed] [Google Scholar]
- 4.Binkhorst R D. The accuracy of ultrasonic measurement of the axial length of the eye. Ophthalmic Surg 198112363–365. [PubMed] [Google Scholar]
- 5.Olsen T. Calculating axial length in the aphakic and the pseudophakic eye. J Cataract Refract Surg 198814413–416. [DOI] [PubMed] [Google Scholar]
- 6.Krag S, Olsen T. Secondary IOL power calculation: a comparison of an optical and a biometric method. Acta Ophthalmol 199169625–629. [PubMed] [Google Scholar]
- 7.McClatchey S K, Parks M M. Theoretic refractive changes after lens implantation in childhood. Ophthalmology 10071041744–1751. [DOI] [PubMed] [Google Scholar]
- 8.Hug T. Use of the aphakic refraction in intraocular lens (IOL) power calculations for secondary IOLs in pediatric patients. J Pediatr Ophthalmol Strabismus 200441209–211. [DOI] [PubMed] [Google Scholar]
- 9.Khan A O. Retinoscopic (refractive) estimation of axial length in paediatric aphakia: a comparison with ultrasonic measurement. Br J Ophthalmol 200690987–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holladay J R, Prager T C, Chandler T Y.et al A three‐part system for refining intraocular lens power calculations. J Cataract Refract Surg 19881417–24. [DOI] [PubMed] [Google Scholar]
- 11.Simon J W, O'Malley M R, Gandham S B.et al Central corneal thickness and glaucoma in aphakic and pseudophakic children. J AAPOS 2005926–29. [DOI] [PubMed] [Google Scholar]
- 12.Osher R H. Adjusting intraocular lens power for sulcus fixation. J Cataract Refract Surg 2004302031. [DOI] [PubMed] [Google Scholar]