Abstract
Aim
To establish the association between the obstruction site, whether it is unilateral or bilateral, age group, and sex.
Methods
A retrospective observational study of 1000 lacrimal ducts of 500 consecutive patients seen in the Emílio Amorim Radiological Clinic, who were suspected of having lacrimal duct obstructions, was performed.
Results
Of the studied patients, 121 were men and 379 were women. Their ages varied between 2 years and 93 years. 148 of the examinations were normal; in 298 the obstructions were unilateral and in 54 they were bilateral. The majority of the obstructions occurred at the valve of Krause. There was a significant difference in the correlation of the obstruction site with sex. The obstruction was total in 378 valves and partial in 28. Other findings included sinusitis, osteomas, bone fractures, fistulae, diverticulum, and lacrimal stones.
Conclusion
Obstruction of the lacrimal ducts is normally total, unilateral, and sited at the valve of Krause. The obstruction of this valve predominantly affects women, whereas obstruction of the valve of Hasner mainly affects men. There was no significant difference in the distribution of obstructions by age group.
Keywords: dacryocystography, lacrimal duct
Dacryocystography, one of the imaging methods that enable us to investigate the anatomy of the lacrimal duct, is mainly used in patients with epiphora. It precisely determines the site of a block or stenosis of the excretory duct and provides reliable details for the indication and choice of the type of surgery to be performed.
Epiphora consists in lacrimation of any aetiology. One case is when an excessive production of tears occurs resulting in inadequate evaporation and drainage. Another very common situation is epiphora caused by inefficient drainage of tears, secondary to a partial or total obstruction of the lacrimal system.1
We sought to establish the association between the obstruction site, unilateral or bilateral, age groups, and sex.
Material and method
An observational retrospective study of 1000 lacrimal ducts of 500 consecutive patients treated in the Emílio Amorim Radiological Clinic suspected of having obstruction of the lacrimal duct was performed using dacryocystography in the period from 2 January 2001 to 16 November 2004. Patients who repeated the examination in this period were excluded.
The sex, age, and dacryocystographic findings of all the patients were evaluated.
The data were submitted to statistical analysis using the non‐parametric χ2 test with 5% significance level (p value <0.05).
Anatomy of the lacrimal ducts
The tears enter the lacrimal duct through the upper and lower lacrimal puncta found in the inner corners of the upper and lower eyelids. The upper and lower lacrimal canaliculi have vertical and horizontal portions (fig 1).
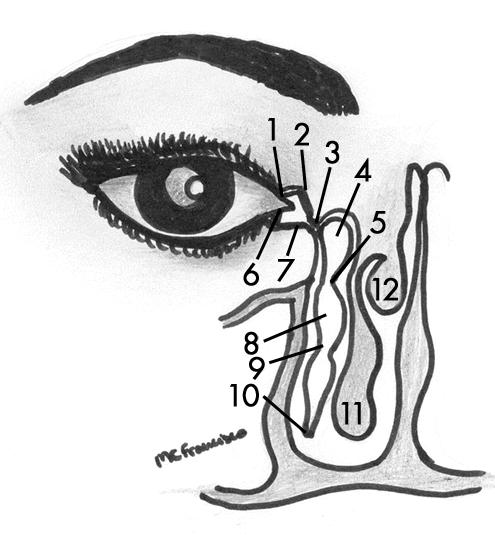
Figure 1 Diagram of the lacrimal ducts. 1, upper lacrimal punctum; 2, upper lacrimal canaliculus; 3, common lacrimal canaliculus; 4, lacrimal sac; 5, valve of Krause; 6, lower lacrimal punctum; 7, lower lacrimal canaliculus; 8, nasolacrimal duct; 9, valve of Taillefer; 10, valve of Hasner; 11, lower nasal cavity; 12, medial nasal cavity.
The union of the upper and lower lacrimal canaliculi occurs in 90% of patients, forming a common lacrimal canaliculus or sinus of Maier. In the other 10% of individuals, the canaliculi independently meet in the lacrimal sac. The sinus of Maier enters the lacrimal sac by a mucous fold called the valve of Rosenmüller.2 Some authors question the existence of this valve, saying it is nothing more than an angle formed by the junction of the common lacrimal canaliculus with the lateral wall of the lacrimal sac.3
At its distal end, the valve of Krause is found. Below this, the lacrimal duct continues as a nasolacrimal duct to the lower nasal meatus, with part of its course through the nasolacrimal bone. Halfway through its intra‐osseo portion, there is the valve of Taillefer and at its runs into the valve of Hasner.2
Background
Imaging studies of the lacrimal duct were first performed by Ewing in 1909 utilising bismuth subnitrate solutions to demonstrate lacrimal abscesses.4
Bollack, in 1924, studied the normal and pathological anatomies of lacrimal ducts using radiology.5
Jones revolutionised the method characterising the lacrimal duct using a fine nylon tube and acquiring an image during the injection of a liposoluble contrast.6
Imaging study of the lacrimal duct
Demonstration of the anatomy of the lacrimal duct can nowadays be achieved by utilising conventional radiography, linear or computed tomography, and magnetic resonance.
In this study, linear tomography was employed as it allows diagnosis of changes in the lacrimal duct by any aetiology and it provides good quality imaging at a lower cost and lower dose of radiation when compared to computed tomography.
Examination technique
Each patient was submitted to head radiographs. After placing the patient in the dorsal decubitus position, local anaesthesia was administered (oxybuprocaine (proxymetacaine) chloride).
A Scalpe number 25 catheter was connected to a disposable syringe containing contrast medium. Its end was introduced through both lacrimal puncta.
The head of the patient was fixed. The contrast medium was administered simultaneously to acquiring linear tomographic images, varying the gap between slices.
Results
The radiological findings were grouped according to the sex of the patient, the site of the obstruction, and whether the obstruction was unilateral or bilateral.
One thousand lacrimal ducts of 500 consecutive patients were evaluated. This group of patients included 121 men (24.2%) and 379 women (75.8%) with ages varying from 2 years to 93 years, an arithmetic mean of 61.35 years and a median of 67 years.
Fifteen of the patients had already undergone some type of ophthalmological surgery. Four presented with nasal polyposis and another four with facial bone fractures.
Obstruction of at least one of the lacrimal ducts was found in 351 patients. Of these, data were obtained for 283 patients as described below.
Epiphora was reported as the motive for the examination in 277 (97.9%) of the studied cases. Seventy two (25.4%) patients reported repetitive infections; however, only six (2.1%) had this as the main complaint.
Of the 281 patients who made some type of clinical treatment, six confirmed a total cure of the symptoms, 146 reported partial improvement, and 129 no improvement of the symptoms. Of the 275 individuals who did not have a total improvement of the symptoms with clinical management, 153 opted for surgical treatment, of whom 13 had bilateral operations.
Of the 500 patients examined at the centre, 148 (29.6%) had normal examinations, 298 (59.6%) presented with unilateral obstructions, and 54 (10.8%) bilateral obstructions. There was no correlation (p = 0.181) between bilateral obstruction and sex.
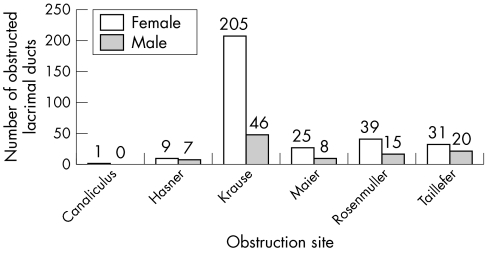
The majority (251) of the obstructions were at the valve of Krause, which proved to be statistically significant (p = 0.009). There was a predominance of this site of obstruction in women (p = 0.013). Obstruction of the valve of Hasner was predominantly found in men (fig 2).
Figure 2 Correlation between sex and the obstruction site. 1% significance level.
Total obstruction was identified in 378 valves (292 in women and 86 in men) and partial in 28 valves (18 in women and 10 in men). In respect to this, no statistical significance was confirmed (p = 0.119).
Obstruction was total in all patients with bilateral alterations and it was partial in 28 (9.4%) of the 298 cases of unilateral obstruction. This difference was significant (p = 0.000).
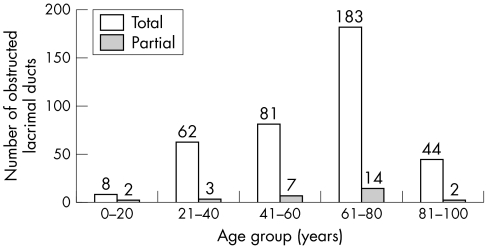
Patients were distributed according to their ages in 20 year age groups (1–20; 21–40; etc.). Subsequently, these groups were analysed in respect of the type of obstruction, but no significant difference was identified (p = 0.429) (fig 3).
Figure 3 Correlation between age group and the type of obstruction. Insignificant.
Some examples of lacrimal duct obstruction are shown in figs 4 and 5.

Figure 4 Total obstruction at the left valve of Rosenmüller (arrow).

Figure 5 Total obstruction at the right valve of Taillefer (arrow) and at the left valve of Hasner (arrowhead).
Other radiological findings of the 500 patients studied were sinusitis in seven, four old bone fractures, two osteomas, four fistulae, four diverticulum of the lacrimal sac, two lacrimal stones, and four nasal polyposis (fig 6).
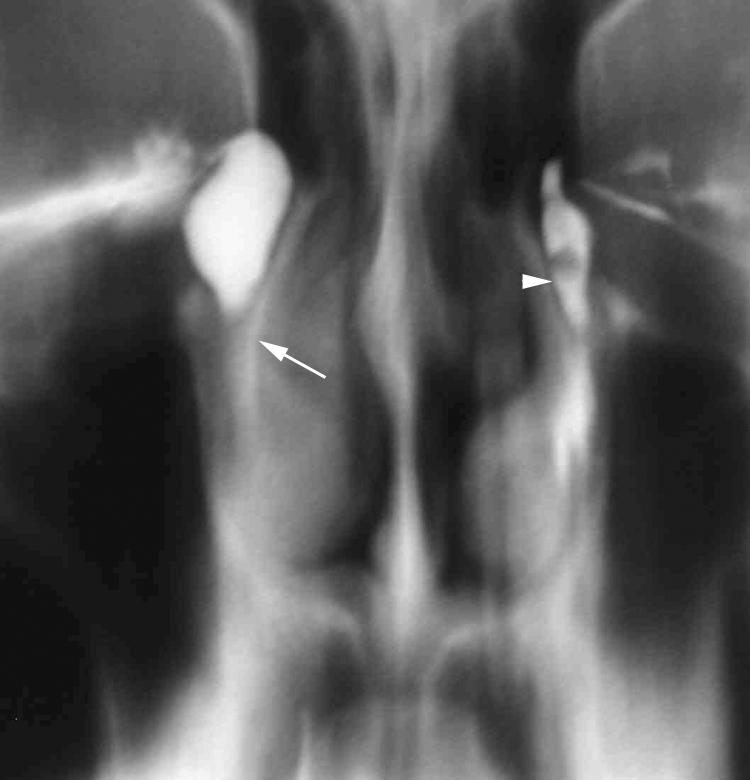
Figure 6 Stone (arrowhead) in the left lacrimal duct and obstruction of the right valve of Krause (arrow).
Discussion
Epiphora is the most common indication for dacryocystography.1 Among the causes of epiphora, the most important are infection, trauma, facial bone fractures, lacrimal duct tumors, irradiation, a scaring process either related to surgery or not, foreign bodies, lacrimal stones, intranasal processes, and congenital obstructions. In many cases the true cause is not established.7
Epiphora in nursing babies normally has a congenital aetiology and can result from incomplete canalisation of the lacrimal duct at the end of the embryonic period or a block caused by residues or thick meconium.8 This disease should be differentiated from pseudo‐obstruction of the lacrimal ducts, which also occurs in this age group.9
Schellini et al described pseudo‐obstruction of the lacrimal ducts in 22 children. They reported that in the majority of cases, lacrimation is sporadic, it is predominantly seen in girls (68.2%), and has as the main finding of concomitant nasal turbinate hypertrophy (77.3%).9
Soares and França concluded that dacryocystography should be the first imaging examination to be performed in newborn babies with suspicion of lacrimal duct obstruction. They studied 64 children and found 53.9% of true obstructions and 46.1% of pervious ducts, demonstrating that the clinical manifestations were related to other factors. They affirmed that the classic congenital obstruction most commonly occurs at the valve of Hasner (66.6%).10
Schellini et al evaluated 100 patients by dacryocystography utilising liposoluble contrast. They obtained a radiograph only after the injection of the contrast medium stating that the radiation dose was lower. They reported that the assessment of the examination was inconclusive in 19 patients because of the unsatisfactory quality of the technique. Approximately 75% of the patients were female and the most common obstruction site was at the point of transition between the lacrimal sac and the nasolacrimal duct.1
In a similar proportion of women, the valve of Krause was also identified as the main obstruction site in this group of patients. Even though water soluble contrast was used and the acquisition of the images was by using linear tomography, no examinations were inconclusive in our study.
Liposoluble contrast media are eliminated slower than water soluble contrast media; however, they tend to cause obstructions, particularly when ducts are altered. Thus, these liposoluble contrast media cause a false appearance of polycystic sacs as the oil does not mix well with the lacrimal secretion.11 This contrast medium should not be used when there is a suspicion of tumours, trauma and fistulae, as, it overflows and can remain in the subcutaneous tissue for several years and induce the formation of granulomas.12
We chose water soluble non‐ionic iodine contrast medium as it is homogeneous, has a low viscosity, a good miscibility with the body fluids, and a pH adjusted between 6.0 and 7.4, similar to tears and is thus non‐irritative. There were no post examination complications in this study.
Some studies affirm that in a normal duct, the contrast totally disappears within 10 minutes.13
Tumours involving the lacrimal duct are rare. Stefanyszyn et al studied 115 patients with tumours of the lacrimal ducts. The most common symptom was epiphora (53%). The tumours were divided into epithelial (82 cases) and non‐epithelial (33 cases). They found a rate of malignancy of approximately 55% for tumors originating in the lacrimal sac.14
Song et al studied 502 patients by means of dacryocystography and found only three lacrimal calculi—two radiotransparent and one radiopaque. The aetiology of the calculus remains unclear, but it is believed that it is associated to impaction of mucus, blood clots, and cellular debris. It presents as a continuous or intermittent lacrimal duct obstruction and a mucopurulent discharge.15
With a similar sample size, our study identified two radiotransparent lacrimal calculi.
Takano and Mendonça studied 24 patients, 75% of whom were women. Three examinations (12.5%) were normal. Of the 21 abnormal examinations, in two (9.5%) bilateral obstructions were found and in 19 (90.5%) the alteration was unilateral. The most common obstruction site was the valve of Krause; an alteration found in 47.8% of the obstructed lacrimal ducts.11
Agarwal assessed 30 patients with dacryocystitis using dacryocystography with conventional radiography. The author concluded that the main obstruction site was at the junction between the lacrimal sac and the nasolacrimal duct and, secondly, in the nasolacrimal duct.16
In our study, we agreed that the most common obstruction site was at the valve of Krause (61.2%); however, the second most common site was above the lacrimal sac, more precisely at the valve of Rosenmüller (13.3%).
The lacrimal sac possesses a slight external inclination and the nasolacrimal duct presents with a small internal inclination. Thus, at the junction there is an angle which favours constriction.17 Added to the fact that the lumen of the nasolacrimal duct is slightly irregular and tortuous, this favours stasis and consequently stenosis.18
The analysis of 63 lacrimal duct performed in São Paulo, Brazil, shows that there is a tendency that the number of individuals who had lacrimal duct blocks increases with age.19
In this study the patients were classified depending on age in 20 year age groups; however, no significant association between age and obstruction site was found.
Dacryocystography allows the identification of the obstruction site and, in some cases, the cause of the obstruction of tear flow, which is fundamental to define the type of clinical or surgical conduct. With an experienced physician, the examination is only slightly uncomfortable. Recently, it has been recommended to perform a bilateral study to enable a comparison with the contralateral duct, specifically to detect asymptomatic alterations.20 Using this tactic, Takano and Mendonça identified changes in 8.3% of the asymptomatic contralateral ducts.11
In our experience, dacryocystography by linear tomography is harmless, easy to perform, and has a low cost, providing a high resolution to demonstrate changes in any aetiology of the lacrimal duct.
Conclusions
Obstruction of the lacrimal ducts occurs more frequently unilaterally, at the valve of Krause, and totally blocks the duct. The obstruction of this valve was more common in women and the valve of Hasner in men. There was no statistical significance in the distribution of obstructions in respect of age group.
Footnotes
Work performed in the Emílio Amorim Radiology Clinic and in the Radiology Department of the Federal University in Rio de Janeiro, Brazil.
References
- 1.Schellini S A, Hercules L A, Padovani C R.et al Dacryocystography in adult lacrimal system evaluation. Arq Bras Oftalmol 20056889–92. [DOI] [PubMed] [Google Scholar]
- 2.Schatz C S. Dacryocystography. In: Bergeron RT, Osborn AG, Som PM. In: Head and neck imaging. 1st ed. St Louis: CV Mosby, 1984, v. 1. p. 669–680.
- 3.Linberg J V, Moore C A. Symptoms of canalicular obstruction. Ophthalmology 1988951077–1079. [DOI] [PubMed] [Google Scholar]
- 4.Ewing A E. Roentgen ray demonstrations of the lacrimal abcess cavity. Am J Ophthalmol 1909241–4. [Google Scholar]
- 5.Bollack J. Sur l'Exploration radiographique des voles lacrymales par l'Injection D'Hulle iodée. Ann Oculist 1924161321–335. [Google Scholar]
- 6.Jones L T. Tear‐sac foreign bodies. Am J Ophthalmol 196560111–113. [DOI] [PubMed] [Google Scholar]
- 7.Linberg J V, McCormick S A. Primary acquired nasolacrimal duct obstruction. A clinicopathologic report and biopsy technique. Ophthalmology 1986931055–1063. [DOI] [PubMed] [Google Scholar]
- 8.Schellini S A, Viveiros M M H, Jaqueta E.et al Congenital nasolacrimal obstruction: successful treatment factors. Arq Bras Oftalmol 200568241–244. [DOI] [PubMed] [Google Scholar]
- 9.Schellini S A, Silva M R B M, Schellini R C. Pseudonasolacrimal obstruction in infancy. Arq Bras Oftalmol 199457348–351. [Google Scholar]
- 10.Soares E J C, França V P. Importância da dacriocistografia no tratamento da obstrução lacrimal do recém‐nascido. Arq Bras Oftalmol 198750225–236. [Google Scholar]
- 11.Takano B A, Mendonça‐Júnior A A. Dacriocistografia: aspectos radiológicos nas alterações das vias lacrimais análise de 24 casos. Radiol Bras 19962923–29. [Google Scholar]
- 12.Munk P L, Burhenne L W, Buffam F V.et al Dacryocystography: comparison of water‐soluble and oil‐based contrast agents. Radiology 1989173827–830. [DOI] [PubMed] [Google Scholar]
- 13.Patrão A L S. Dacriocistografia. Rev Bras Oftalmol 1983XLII68–72. [Google Scholar]
- 14.Stefanyszyn M A, Hidayat A A, Pe'er J J.et al Lacrimal sac tumors. Ophthalmic Plast Reconstr Surg 199410169–184. [DOI] [PubMed] [Google Scholar]
- 15.Song H Y, Lee D H, Ahn H.et al Lacrimal system obstruction treated with lacrimal polyurethane stents: outcome of removal of occluded stents. Radiology 1998208689–694. [DOI] [PubMed] [Google Scholar]
- 16.Agarwal M L. Dacryocystography in chronic dacryocystitis. Am J Ophthalmol 196152245–251. [DOI] [PubMed] [Google Scholar]
- 17.Wolff E.The anatomy of the eye and orbit. London: Lewis, 1954
- 18.Schaeffer J P.The nose, paranasal sinuses, nasolacrimal passage ways and olfactory organs in man. Philadelphia: Blakiston's, 1920
- 19.Bison S, Scarpi M J, Soccol O.et al Etiologia da obstrução canalicular. Arq Bras Oftalmol 200164401–403. [Google Scholar]
- 20.Robert Y. Bilateral injection of contrast medium for dacryocystography. Am J Ophthalmol 198395117–118. [DOI] [PubMed] [Google Scholar]