Maxillary artery embolisation with polyvinyl alcohol (PVA) is a procedure used for the treatment of intractable epistaxis. We report a rare but devastating complication of this otherwise safe and successful procedure.
Case report
A 46‐year‐old man presented to the accident and emergency department with a 1‐day history of left epistaxis. He had had mild infrequent episodes in the past. He had cauterisation of the Little's area, but as the bleeding persisted, nasal packing was performed and blood tests were done. The platelet count was 310×109/l; other tests were normal. The epistaxis persisted the next day and a new bismuth idoform paraffin paste nasal pack was inserted. He underwent a nasal endoscopy the next day and an arterial bleed in the area of the left sphenopalatine artery was observed. Electrocautery to this area was performed and a post‐nasal pack was applied.
Despite these measures, the epistaxis continued for a further couple of days. The patient underwent carotid angiography via the left femoral artery under local anaesthesia. The catheter was advanced through the left common carotid artery, left external carotid and left internal maxillary artery. Selective endovascular embolisation of the left internal maxillary artery with 45–150 μm polyvinyl alcohol (PVA) particles was carried out. By the end of the procedure, the patient experienced left‐sided loss of vision. His blood pressure was 167/100 mm Hg, pulse 52 beats/min and SaO2 99%.
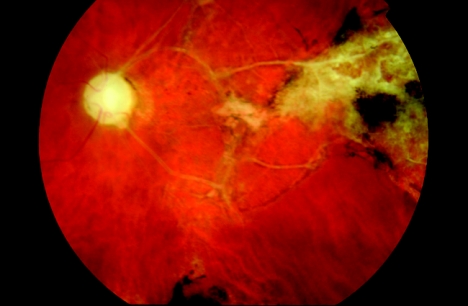
The patient was examined by an ophthalmologist and was found to have no perception of light, afferent pupillary defect and classic signs of a central retinal artery occlusion in the left eye. A more recent photograph of his left fundus shows optic atrophy and retinal fibrosis. The draining veins of the affected temporal retina are occluded completely (fig 1). This is a unique fundus appearance not noted in vascular occlusions with more common calcific, fibrinoplatelet or cholesterol emboli.
Figure 1 Photograph of the left fundus showing retinal fibrosis.
Comment
The aetiology of retinal arteriolar occlusion is diverse. The most common causes were cholesterol and fibrinoplatelet (from a carotid source) followed by calcific emboli (from a cardiac source) in one case series of 70 patients.1 Risk factors can be multifactorial and a comprehensive physical examination and systemic work‐up is essential.2 The treatment is directed to the cause. However, acute treatment of the condition to aid visual recovery is still disappointing.
The case described is an unusual, iatrogenic event. To our knowledge only one case of central and posterior ciliary artery occlusion after PVA embolisation has been reported3 (PubMed search for articles in English). Although reporting is not a reflection of true incidence, such an occurrence is still rare as it is only the external carotid system that is involved in embolisation, whereas the ophthalmic circulation is derived from the internal carotid system. This perceived notion of safety has been further supported by the advocation of embolisation treatment as the primary treatment of intractable epistaxis, citing low complication rates in a large case series.4,5
The mechanism of PVA particles affecting the ocular circulation distant from their site of injection is manifold. Post‐nasal bleeding is usually arterial and the vasculature is derived from both external (sphenopalatine and greater palatine branches of the internal maxillary artery) and internal carotid systems (anterior and posterior branches of the ophthalmic artery). The presence of these normal or any abnormal anastamoses (such as the artery of foramen rotundum, to the carotid siphon) provides anatomical access of embolic agents to the ophthalmic circulation.6
PVA particles are available in sizes ranging from 45 to 2000 μm. The smaller the particle size, the greater the ability to travel downstream and cause tissue destruction. Smaller particles occlude arterioles including retinal arterioles, as in our patient. Over‐forceful injection can result in a reflux into the internal carotid system.4
The clinical appearance of retinal arterial occlusion owing to fibrotic agents like PVA is unique and distinct. This is due to the fact that polyvinyl alcohol particles are capable of inducing an intense fibrotic response (with a minimal amount of inflammatory cells) in tissues.7 This can be of significance in pinpointing the aetiology where other risk factors may coexist. ENT and ophthalmic surgeons need to be aware of this rare but devastating complication occurring after PVA embolisation for epistaxis.
References
- 1.Arruga J, Sanders M D. Ophthalmologic findings in 70 patients with evidence of retinal embolism. Ophthalmology 1982891336–1347. [DOI] [PubMed] [Google Scholar]
- 2.Graham E M. The investigation of patients with retinal vascular occlusion. Eye 19904464–468. [DOI] [PubMed] [Google Scholar]
- 3.Mames R N, Snady‐McCoy L, Guy J. Central retinal and posterior ciliary artery occlusion after particle embolization of the external carotid artery system. Ophthalmology 199198527–531. [DOI] [PubMed] [Google Scholar]
- 4.Vitek J. Idiopathic intractable epistaxis: endovascular therapy. Radiology 1991181113–116. [DOI] [PubMed] [Google Scholar]
- 5.Elahi M M, Parnes L S, Fox A J.et al Therapeutic embolization in the treatment of intractable epistaxis. Arch Otolaryngol Head Neck Surg 199512165–69. [DOI] [PubMed] [Google Scholar]
- 6.Koh E, Frazzini V I, Kagetsu N J. Epistaxis: vascular anatomy, origins, and endovascular treatment. Am J Roentgenol 2000174845–851. [DOI] [PubMed] [Google Scholar]
- 7.Smith A R, Garrison J L, Greene W B.et al The clinical, histologic, and ultrastructural presentation of polyvinyl sponge (Ivalon) breast prostheses removed for massive fluid accumulation. Plast Reconstr Surg 19991031970–1974. [DOI] [PubMed] [Google Scholar]