Abstract
Aim
To study the histological effects of trans‐scleral cyclophotocoagulation (TCP) and endoscopic cyclophotocoagulation (ECP) on the ciliary body and other structures collected at autopsy and to compare with untreated controls.
Materials and methods
TCP and ECP were performed on human eyes at autopsy. Detailed histological evaluations were perfomed using light microscopy and scanning electron microscopy on treated eyes and compared with untreated controls.
Results
Histological changes were observed with both light microscopy and scanning electron microscopy for all treated tissues. Tissue treated with TCP showed pronounced tissue disruption of the ciliary body muscle and stroma, ciliary processes, and both pigmented and non‐pigmented ciliary epithelium. ECP‐treated tissue exhibited pronounced contraction of the ciliary processes with disruption of the ciliary body epithelium, sparing of the ciliary body muscle and less architectural disorganisation. The sclera was not affected by either laser treatment.
Conclusions
ECP treatment caused less damage to the ciliary body compared with TCP when evaluated by light microscopy and scanning electron microscopy. Compared with TCP, ECP seems to be a more selective form of cyclophotocoagulation, resulting in less tissue disruption while achieving the goal of destroying ciliary body epithelium.
Cycloablation is a procedure typically performed for cases of glaucoma refractory to other medical and surgical treatments.1,2,3,4,5,6 Ablation of the ciliary body epithelium lowers the intraocular pressure (IOP) by decreasing the production of aqueous humor.1,2,6,7,8,9,10,11,12 Although many cycloablative techniques exist, two forms, trans‐scleral cyclophotocoagulation (TCP) and endoscopic cyclophotocoagulation (ECP), have found a role in modern clinical practice.
TCP is a non‐invasive laser technique in which the laser energy is transmitted through the sclera with minimal absorption or scatter. Typically, TCP is performed with a semiconductor diode laser that emits light in the near infrared spectrum (810 nm), which is strongly absorbed by melanin present in ciliary body epithelium. The G‐probe (IRIS Medical Instruments, Mountain View, California, USA) handpiece allows for fairly consistent probe placement in relation to the limbus and more consistent spacing circumferentially, compared with techniques in which the placement is measured manually. The anterior edge is placed at the limbus so that the laser energy is directed 1.2 mm posterior to the limbus and over the ciliary body. In non‐standard eyes, energy may not be directed over the ciliary body, increasing the probability of inadequate treatment, or, worse, treatment of adjacent tissues such as the iris or retina.
The quartz tip of the probe extends 0.7 mm beyond the contact surface, thus indenting the conjunctiva and sclera to allow better laser penetration (fig 1). Energy levels are titrated to maximise the effect while avoiding an audible “pop”, which indicates overtreatment and explosion of ciliary body tissue. Diode‐laser TCP has a large rate of complications and postoperative discomfort, and is usually reserved for eyes with limited visual potential or in eyes in which surgical intervention is not an option.2,7,8
Figure 1 G‐probe.
A newer device for cycloablation, ECP, has been developed (EndoOptiks, Little Silver, New Jersey, USA) with the aim of providing direct visualisation of treated tissue.13 The device's handpiece incorporates a diode laser that emits pulsed or continuous energy at a wavelength of 810 nm, a 175‐W xenon light source that provides illumination, a helium–neon lase‐ aiming beam and a fibreoptic video camera. All four elements are transmitted via fibreoptics to a 20‐gauge probe that can be inserted intraocularly through a self‐sealing, temporally clear corneal incision. With the ability to precisely ablate ciliary body epithelium, this instrument has theoretical advantages over the trans‐scleral approach in the management of glaucoma, particularly in eyes with good visual potential. The surgeon can use visual feedback to determine the exact placement of the laser energy and the extent of treatment, thus decreasing the risk of overtreatment and increasing the likelihood of adequate treatment. Histopathological studies of enucleation specimens after TCP have been performed in humans.14,15,16 This study examines and compares the histological changes in human autopsy eyes after TCP and ECP laser treatments with that of normal untreated controls.
Materials and methods
Two human donor eyes were obtained from the San Diego Eye Bank. The eyes had brown irides and were harvested within 4 h of death from Caucasian individuals with no history of eye disease. The eyes were mounted on a suction device to provide stability before initiation of the laser treatments. This was followed by inflation of the eye with balanced salt solution introduced through the optic nerve with a 25‐gauge needle to bring the eye to a normative IOP. Inflation of the eye in this fashion allowed for proper external application of the TCP G probe. A single 8–0 vicryl suture was placed at 12 o'clock to provide a landmark to guide treatment and future dissection.
An Iris Oculight SLx diode laser photocoagulation system (Iris Medical Instruments) equipped with a G‐probe was used for the TCP laser treatment. Under light to medium pressure, the hand‐held diode laser was positioned on the conjunctival surface of the sclera 1.2 mm from the visible limbus (a distance determined by the spacing of the G‐probe footplate). On the basis of clinical experience, with the probe oriented perpendicular to the visual axis, trans‐scleral laser pulses of 2 W and 2.5 s duration were transmited to the area of the pars plicata and carried out for 120° counterclockwise from the 12 o'clock landmark. Energy was increased until an audible pop was heard, at which time energy was decreased until no audible pops were heard.
ECP was performed using the Endo Optiks System (Endo Optiks, Little Silver, New Jersey, USA). A 2.8 mm keratome was used to create a temporally clear corneal incision. A paracentesis was created and the anterior chamber was reformed with viscoelastic (Healon V, Advanced Medical Optics, Santa Anna, California, USA) to expand the ciliary sulcus and facilitate visualisation of the ciliary processes. After orientation and illumination of the ECP image on the monitor, the 20‐gauge probe was inserted through the incision and into the ciliary sulcus. At this time, the ciliary processes were viewed on the monitor and the treatment was started. The laser was set on continuous mode with energy settings of 0.25 W. A total of 120° of ciliary processes was treated, with whitening and shrinkage of the ciliary processes as the treatment end point. The treatment was initiated at the 12 o'clock position as identified by the vicryl suture and proceeded clockwise. The remaining 120° were left untreated as the normal control.
After the laser treatments, the eyes were processed in 4% paraformaldehyde and 2.5% glutaraldehyde at 4°C for 24 h. Each eye was subsequently sectioned into three 120° specimens representing the TCP‐treated, ECP‐treated and normal areas. The specimens from the paraformaldehyde‐fixed tissue were then washed with a 0.1 M phosphate‐buffered solution, dehydrated in increasing concentrations of propanol, cleared with xylene and in a paraffin tissue processor (Miles Tissue‐Tek VIP, model 2000, Spectron Corp, Burlington, WA, USA). After removing the tissue cassettes from the processor, they were placed into the holding tank of the embedding centre. Using heated forceps, each specimen was transferred to an embedding mould partially filled with paraffin wax and oriented appropriately. The moulds were then filled completely with paraffin wax and placed in a cooling plate. After cooling overnight, the paraffin wax blocks were removed gently from the moulds, 8 μm sections were prepared, dewaxed in xylene, hydrated in decreasing concentrations of ethanol, stained with haematoxylin and eosin/phloxine, and examined histologically using standard light microscopy. The specimens from the glutaraldehyde‐fixed eye were washed with 0.1 M phosphate‐buffered solution, soaked in 1% osmium tetroxide, dehydrated in increasing concentrations of ethanol and kept in acetone. They were then dried, to the critical point ion coated and examined using scanning electron microscopy.
Results
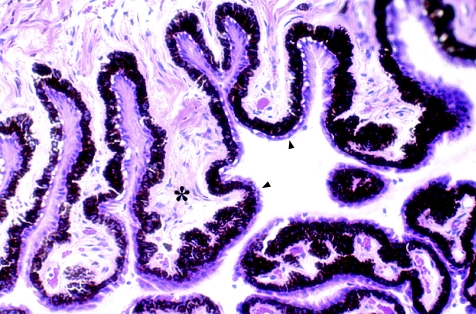
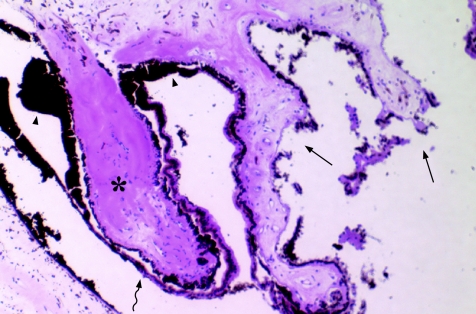
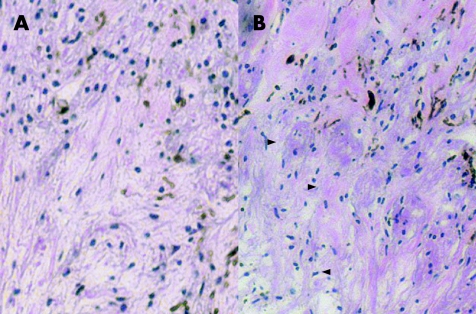
Compared with normal non‐treated human eye tissue (fig 2) in which there were no visible structural changes, histological examination of TCP‐treated human eye tissue, stained with haematoxylin–eosin by light microscopy, showed considerable damage similar in morphological appearance to those described previously.14,15,16 The laser‐treated areas showed destruction of pigmented and non‐pigmented ciliary epithelium and capillaries in the ciliary processes, with pigment clumping, coagulative changes and destruction of the processes' stroma (fig 3). Loss of the architectural organisation seemed to extend into the ciliary muscle layer in some areas, but not in others (fig 4A,B).
Figure 2 Light microscopy of normal ciliary processes showing their lacy contour with normal‐appearing stroma (asterisk), pigmented and non‐pigmented ciliary epithelium (arrowheads).
Figure 3 Light microscopy of trans‐scleral cyclophotocoagulation‐treated tissue showing separation of the non‐pigmented and pigmented ciliary epithelium (wavy arrow), pigment clumping (arrowheads), coagulative necrosis of the underlying ciliary stroma (asterisk) and architectural destruction of the treated tissue (straight arrows).
Figure 4 Light microscopy of a normal‐appearing ciliary muscle (A) and some loss of architectural organisation (arrowheads) of trans‐scleral cyclophotocoagulation‐treated tissue (B).
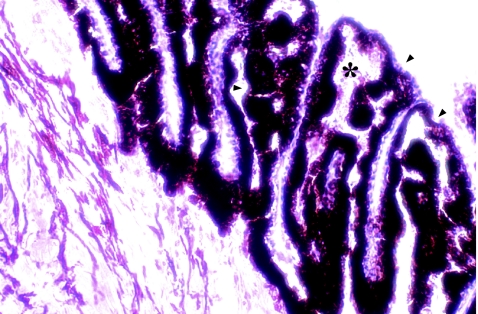
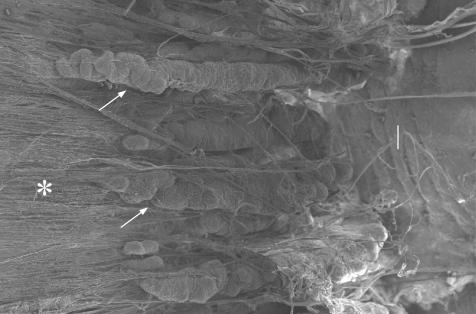
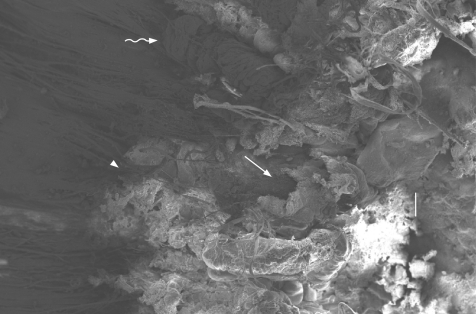
By contrast, ECP‐treated human tissue showed loss of the lacy appearance of the stroma of the ciliary processes with destruction of the non‐pigmented epithelium and clumping of the pigmented epithelium, with minimum to no coagulative changes of the tissue beyond the ciliary processes (fig 5). Scanning electron microscopy showed normal long and velvety appearance of the ciliary processes in the normal untreated tissue (fig 6) and extensive shrinkage of the ciliary processes and effacement of the ciliary epithelium after ECP treatment (fig 7). TCP‐treated tissue had extensive architectural disruption extending into the pars plana and iris stroma (fig 8).
Figure 5 Light microscopy of endoscopic cyclophotocoagulation‐treated tissue showing loss of the lacy appearance of the ciliary processes (asterisk) with destruction of the non‐pigmented epithelium and clumping of the pigmented epithelium (arrowheads).
Figure 6 Scanning electron microscopy of normal ciliary processes (arrows) with adjacent pars plana (asterisk) and iris stroma (I).
Figure 7 Scanning electron microscopy of endoscopic cyclophotocoagulation‐treated ciliary processes showing shrinking of the processes (arrows) with blunting of their tips (arrowheads) and disruption of the normal architecture of the overlying epithelium. The adjacent pars plana (asterisk) and iris stroma (I) are unaffected.
Figure 8 Scanning electron microscopy of trans‐scleral cyclophotocoagulation (TCP)‐treated ciliary processes showing extensive architectural destruction (straight arrow) extending into the pars plana (arrowhead) and iris stroma (I). Normal ciliary processes are visible adjacent to the treated area (wavy arrow).
Discussion
TCP is a non‐invasive procedure used to ablate the ciliary body epithelium, thus reducing the rate of the aqueous production. It is indicated for patients with refractory glaucoma who have failed trabeculectomy or tube shunt procedures, patients with limited vision and increased IOP, and patients with blind painful eyes.15 However, results are difficult to predict, as the surgeon must estimate the position of the ciliary processes without direct visualisation.16 Variations in the anatomy and pigmentation of the ciliary body may further influence the success, and may explain why the response to treatment varies from one individual to another.17 Another important issue regarding treatment is the optimum power settings and duration of laser treatment. It is now thought that audible “pops” indicate overtreatment, and their presence can be used to titrate laser parameters, and that the maximum energy level delivered should be just below the threshold required to produce such “pops”.18 TCP has been associated with complications such as intense intraocular inflammation, postoperative pain, intraocular haemorrhage, choroidal detachment, hypotony and phthisis.2,7,8 For this reason, it is usually performed cautiously, with surgeons erring on the side of undertreatment to avoid postoperative hypotony. This approach leads to a large failure rate in IOP control and the need for retreatment.3
ECP provides the surgeon with the ability to treat ciliary processes under direct visualisation and offers the potential to decrease the complication rate, potentially improving the efficacy of the procedure. This is especially advantageous in eyes with atypical ciliary body anatomy, such as in patients with paediatric glaucoma.19 Barkana et al22 used ECP in a child with persistently increased IOP after three treatments with TCP and achieved better results in controlling the IOP using ECP. Using the direct visualisation system of the ECP, the authors found many scars in the pars plana, away from the ciliary processes, representing misplaced TCP laser burns. In addition, properly placed external burns over the ciliary processes did not fully destroy the tissue beneath them.20
ECP has been used to effectively reduce IOP in primary open‐angle glaucoma, congenital glaucoma, aphakic and pseudophakic glaucoma, uveitic glaucoma, pseudoexfoliative glaucoma, pigmentary glaucoma, neovascular glaucoma and traumatic glaucoma.6,12,19,23 In patients with penetrating keratoplasties, ECP may be preferred over TCP as it seems to be associated with a lower incidence of corneal graft rejection and failure.6,22
This study examines and compares the histological outcomes in human eyes from autopsy after TCP and ECP laser treatments. We found clear differences in the tissue treated by the two lasers. These differences were noted both with light microscopy and scanning electron microscopy. The histological findings showed marked disruption of the ciliary epithelium and coagulative changes of the underlying ciliary stroma after TCP treatment. TCP treatment was characterised by extreme architectural disruption of treated tissue, with disintegration of the tissue in some cases. The energy level used in this study did not produce any audible “pops”, and thus intentional overtreatment and explosion of the ciliary body tissue was avoided. This may explain the subtle loss of architectural organisation of the ciliary muscle that we observed compared with the extensive destruction of the ciliary muscle reported by McKelvie et al.14
ECP produced most of its structural changes at the level of the ciliary epithelium and ciliary process stroma with less effect on the ciliary body muscle and on the less superficial structures. The ciliary processes treated with ECP remained organised despite complete treatment and did not exhibit areas of disintegration as witnessed with TCP. This finding could be explained by the more specific targeting of the ciliary epithelium with ECP and the use of lower‐energy settings because of direct exposure and termination of the treatment based on the visible shrinkage and whitening of the target tissue. This minimised the possibility of overtreatment. The scanning electron microscopy observations correlated with the histological findings in all treatment groups.
Scleral and muscle injury was not a consistent finding in this study, a finding in line with several studies involving TCP treatment at comparable energy levels.23,24 However, thermal damage to the sclera has been reported in studies that used lower energy and pulse duration parameters than those used in this study.25,26,27 Although every effort was made in this study to standardise procedures, it must be recognised that results based on autopsy donor tissue could differ from those encountered in practice. Factors such as energy diffusion can vary between living and dead tissue. Inherent differences in the design of laser delivery systems and the surgeon's skills may also influence the findings. This study is an acute in vitro experiment, and the observations are limited to the detection of certain morphological effects, such as disruption of the pigmented tissues, which become apparent immediately after irradiation with laser light. Other subacute effects, such as coagulative necrosis affecting muscle cells and other tissues along the laser beam's path, may not be detectable acutely in dead tissue and remain hidden until we have the opportunity to observe the inflammatory and other tissue responses occurring in vivo.
Our study confirms findings from other studies about the nature of the changes induced by TCP. We also show that the structural changes induced with ECP are much less extensive than those with TCP. Properly performed ECP does seem to selectively target the ciliary epithelium without markedly altering other structures in the eye. On the basis of this information, surgeons can use these procedures to achieve the clinical goals of laser cyclophotocoagulation.
Acknowledgements
We thank the following individuals for their assistance with the research: Gloria Limetti from the Department of Otolaryngology, Eye and Ear Institute, Pittsburgh, Pennsylvania, and Marc W Rubin from the Center for Biologic Imaging, Pittsburgh, Pennsylvania, USA.
Abbreviations
ECP - endoscopic cyclophotocoagulation
IOP - intraocular pressure
TCP - trans‐scleral cyclophotocoagulation
Footnotes
Funding: Core Grant for Vision Research—EY080908, supported in part by an unrestricted grant from Research to Prevent Blindness and The Eye and Ear Foundation (Pittsburgh, PA).
Competing interests: RJN has received honoraria for speakerships for EndoOptiks.
Published Online First 20 September 2006
The authors do not have a financial/proprietary interest in any of the devices, equipment, instruments or drugs discussed in this article.
The results of this study have been presented at the American Glaucoma Society (AGS) meeting in Charlestown, South Carolina, USA, March 2006.
References
- 1.Kosoko O, Gaassterland D E, Pollack I P.et al Long term outcome of initial ciliary ablation with contact diode laser transscleral cyclophotocoagulation for severe glaucoma. Ophthalmology 19961031294–1302. [DOI] [PubMed] [Google Scholar]
- 2.Bloom P, Tsai J, Sharma K.et al “Cyclodiode” transscleral diode laser cyclophotocoagulation in the treatment of advanced refractory glaucoma. Ophthalmology 19971041508–1520. [DOI] [PubMed] [Google Scholar]
- 3.Threlkeld A B, Johnson M H. Contact transscleral diode cyclophotocoagulation for refractory glaucoma. J Glaucoma 199983–7. [PubMed] [Google Scholar]
- 4.Schlote T, Derse M, Zierhut M. Transscleral diode laser cyclophotocoagulation for treatment of refractory glaucoma secondary to inflammatory eye diseases. Br J Ophthalmol 200084999–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lai J, Tham C, Chan J.et al Diode laser transscleral cyclophtocogaulation as primary surgical treatment for medically uncontrolled chronic angle closure glaucoma. J Glaucoma 200514114–119. [DOI] [PubMed] [Google Scholar]
- 6.Chen J, Cohn R A, Lin S C.et al Endoscopic photocoagulation of the ciliary body for treatment of refractory glaucomas. Am J Ophthalmol 1997124787–796. [DOI] [PubMed] [Google Scholar]
- 7.Kramp K, Vick H, Guthoff R. Transscleral diode laser contact cyclophotocoagulation in the treatment of different glaucomas, also as primary surgery. Graefes Arch Clin Exp Ophthalmol 2002204698–703. [DOI] [PubMed] [Google Scholar]
- 8.Chang S H, Chen Y C, Li C Y.et al Contact diode laser transscleral cyclophotocoagulation for refractory glaucoma: comparison of treatment protocols. Can J Ophthalmol 200434511–516. [DOI] [PubMed] [Google Scholar]
- 9.Nourredin B N, Zein W, Haddad C.et al Diode laser transscleral cyclophotocoagulation for refractory glaucoma: a 1 year follow‐up of patients treated using an aggressive protocol. Eye 20051–7. [DOI] [PubMed]
- 10.Patel A, Thompson J T, Michels R G.et al Endolaser treatment of the ciliary body for uncontrolled glaucoma. Ophthalmology 198693825–830. [DOI] [PubMed] [Google Scholar]
- 11.Zarbin M A, Michels R G, de Bustros S.et al Endolaser treatment of the ciliary body for severe glaucoma. Ophthalmology 1988951639–1828. [DOI] [PubMed] [Google Scholar]
- 12.Uram M. Ophthalmic laser microendoscope ciliary process ablation in the management of neovascular glaucoma. Ophthalmology 1992991823–1828. [DOI] [PubMed] [Google Scholar]
- 13.Lin S. Endoscopic cyclophotocoagulation. Br J Ophthalmol 2002861434–1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McKelvie P A, Walland M J. Pathology of cyclodiode laser: a series of nine enucleated eyes. Br J Ophthalmol 200286381–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schuman J S, Noecker R J, Puliafito C A.et al Energy levels and probe placement in contact transscleral semiconductor diode laser cyclophotocoagulation in human cadaver eyes. Arch Ophthalmol 19911091534–1538. [DOI] [PubMed] [Google Scholar]
- 16.Feldman R M, El Harazi S M, LoRusso F J.et al Histopathologic findings following contact transscleral semiconductor diode laser cyclophotocoagulation in a human eye. J Glaucoma 19976139–140. [PubMed] [Google Scholar]
- 17.Pastor S A, Singh K, Lee D A.et al Cyclophotocoagulation. A report by the American Academy of Ophthalmology. Ophthalmology 20011082130–2138. [DOI] [PubMed] [Google Scholar]
- 18.Uram M. Technology assessment of cyclophotocoagulation. Ophthalmology 2003110874. [DOI] [PubMed] [Google Scholar]
- 19.Neely D E, Plager D A. Endocyclophotocoagulation for management of difficult pediatric glaucomas. J AAPOS 20015221–229. [DOI] [PubMed] [Google Scholar]
- 20.Rebolleda G, Munoz F J, Murube J. Audible pops during cyclodiode procedures. J Glaucoma 19998177–183. [PubMed] [Google Scholar]
- 21.Plager D A, Neely D E. Intermediate‐term results of endoscopic diode laser cyclophotocoagulation for pediatric glaucoma. J AAPOS 19993131–137. [DOI] [PubMed] [Google Scholar]
- 22.Barkana Y, Morad Y, Bennun J. Endoscopic photocoagulation of the ciliary body after repeated failure of transscleral diode laser cyclophotocoagulation. Am J Ophthalmol 2002133405–407. [DOI] [PubMed] [Google Scholar]
- 23.Gayton J L, Van De Karr M, Sanders V. Combined cataract and glaucoma surgery: trabeculectomy versus endoscopic laser cycloablation. J Cataract Refract Surg 1999251214–1219. [DOI] [PubMed] [Google Scholar]
- 24.Lin S C, Chen J, Hwang D G.et al Endoscopic cyclophotocoagulation for the treatment in glaucoma in keratoplasty patients. Invest Ophthalmol Vis Sci 1998392157B14 [Google Scholar]
- 25.Hennis H L, Assia E, Stewart W C.et al Transscleral cyclophotocoagulation using a semiconductor diode laser in cadaver eyes. Ophthalmic Surg 199122274–278. [PubMed] [Google Scholar]
- 26.Coleman A L, Jampel H D, Javitt J C.et al Transscleral cyclophotocoagulation of human autopsy and monkey eyes. Ophthalmic Surg 199122638–643. [PubMed] [Google Scholar]
- 27.Palmer D J, Cohen J, Torczynski E.et al Transscleral diode laser cyclophotocoagulation on autopsy eyes with abnormally thinned sclera. Ophthalmic Surg Lasers 199728495–500. [PubMed] [Google Scholar]