Abstract
Aims
To measure the productivity and factors associated with high productivity of trichiasis surgeons.
Methods
A standardised, pretested questionnaire was posted to all trichiasis surgeons trained in Tanzania at the address listed at the time of training, and then followed up by post and telephone with those who did not return the form. Questions asked related to place of work, number of surgeries carried out, supplies and equipment available, and outreach activities. A random selection of high‐productivity and low‐productivity surgeons was invited to a focus group meeting to discuss factors that affected productivity.
Results
28 of the trained surgeons had died, retired or could not be located. Forms were retrieved from 95 others. Productivity (averaged over the past 4 years) was low overall, but highly variable. The mean number of surgeries per year was 22.3 (SD 48.1) and the median was 7. The most important factor associated with higher productivity was conducting outreach activities. Conducting outreach was associated with having a complete set of instruments and consumables and with being able to identify a supervisor.
Conclusions
Redesigning the provision of trichiasis surgery (in particular, supervision, support and community programmes/outreach) is necessary to ensure that the investment from training is used adequately.
Trachoma is still an important cause of blindness worldwide, although it is distributed in pockets rather than being a universal problem. In particular, trachoma continues to contribute to blindness in parts of Tanzania and other sub‐Saharan African countries. The current World Health Organization strategy for reducing trachoma, called the SAFE strategy, includes provision of surgery for trachomatous trichiasis, antibiotic distribution for villages where active trachoma is endemic and changes in basic hygiene practices such as washing the face and environmental cleanliness.1
In Tanzania, 7107 trichiasis operations were conducted between 1999 and 2003. In 2004, it was estimated that there were still 54 000 people with trichiasis in need of surgical correction, and the Ministry of Health (MoH) set a target of providing 43 000 more surgeries by the year 2008 (National Trachoma Control Programme Strategic Plan 2004–8, MoH, United Republic of Tanzania).
Several surgical procedures have been suggested for correcting trachomatous trichiasis; most are relatively simple and are performed by non‐ophthalmologist health workers including nurses, clinical officers and various cadres of health assistants. The World Health Organization currently recommends the bilamellar tarsal plate rotation (BTRP) as the most effective procedure.2 Recognising the need for non‐ophthalmologist health workers to be trained, Helen Keller International designed a 10‐day training course and set up a centre dedicated to training such workers to perform BTRP in Kongwa, Tanzania, in 1995. The course consisted of 3 days theory and 7 days practical fieldwork (described in a field manual, Community‐based Trichiasis Surgery3). Selection of health workers to attend the course was generally made by MoH through regional eye coordinators.
This study was undertaken to measure the productivity of surgeons and to identify factors associated with high or low productivity. The goal was to provide information to assist in planning human resources, including (1) the development of selection criteria for training and placement, and (2) planning for support and supervision after training.
Methods
A standard questionnaire was designed to obtain information on the following: year of training; current position (title); current employer (private or government and primary, secondary or tertiary); days per week spent on eye care (as opposed to general medicine); number of trichiasis surgeries performed in each of the years 2001, 2002 and 2003; whether the worker went outside his station to perform surgery (outreach); whether the surgical set was complete and a list of eight essential consumables was available at the time the questionnaire was completed; and whether the health worker could identify his supervisor. The questionnaire was translated into Kiswahili and pretested.
A list of names and last‐known addresses of all the health workers trained from 1995 to 2004 was compiled from records at the Kongwa training centre. The questionnaire was mailed with a cover letter and a return stamped envelope to all 123 Tanzanians who completed training. A second mail was sent to those who did not respond within 2 months. Finally, phone calls to the health workers or their supposed supervisors were made to trace non‐respondents.
Frequencies of responses were entered in SPSS. We calculated the productivity per year for each surgeon by dividing the number of trichiasis surgeries carried out by the number of years the surgeon had been in practice, using data from 2001 to 2004. Means and standard deviations (SDs) in productivity were calculated, and non‐parametric tests (Mann–Whitney U test) were used to calculate p values for differences in productivity between groups.
Trichiasis surgeons were divided into low and high productivity groups (<10 surgeries/year and >30 surgeries/year). Five were selected from each group by using a random number table; these were invited to attend a meeting in Dar‐es‐Salaam to discuss their experience with trachoma surgery training and practice. Eight attended the meeting, where they participated in discussions of several issues including factors leading to low productivity, surgeon competence to perform surgery, adequacy of training, availability of patients needing operation, availability of surgical instruments and supplies, priority granted to trichiasis surgery by the local health management teams, surgeons willingness to perform surgery and patients willingness to undergo surgery.
Results
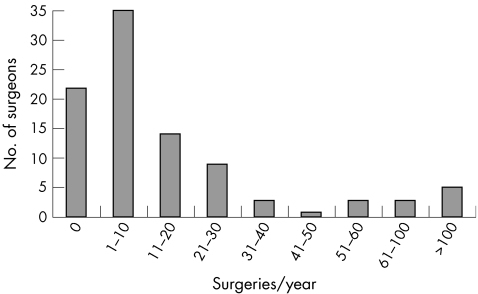
Records at the training centre showed that 123 Tanzanians were trained between 1995 and 2004; 95 of these returned questionnaires. Of the 28 non‐respondents, 8 had died or transferred out of eye work completely and 20 could not be traced. Thus, we had 95 active surgeons for analysis. Figure 1 shows the productivity of the respondents. Table 1 shows some characteristics describing the trichiasis surgeons.
Figure 1 Number of surgeries per year performed by trachomatous trichiasis surgeons.
Table 1 Descriptive characteristics of active trichiasis surgeons.
| Variable | n (%) |
|---|---|
| <40 years old | 23 (26) |
| ⩾40 years old | 65 (74) |
| Male | 55 (58) |
| Female | 40 (42) |
| Works in mission hospital | 11 (12) |
| Works in district hospital | 40 (42) |
| Works in regional hospital | 18 (19) |
| Works in dispensary or clinic | 26 (27) |
| Ophthalmic nurse | 49 (52) |
| Ophthalmic assistant | 18 (19) |
| Assistant medical officer in ophthalmology | 4 (4) |
| Other non‐ophthalmic trained* | 24 (25) |
| Access to surgical consumables incomplete | 78 (82) |
| Access to surgical consumables complete | 17 (18) |
| TT surgical sets incomplete† | 24 (45) |
| TT surgical set complete | 29 (55) |
| Days/week working in eye care‡ | |
| 0 | 1 (1) |
| 1 | 13 (14) |
| 2 | 13 (14) |
| 3 | 13 (14) |
| 4 | 1 (1) |
| 5 | 46 (48) |
TT, trachomatous trichiasis.
*Includes general clinical officers, nurses or health assistants.
†Owing to printing error, this question was omitted from 42 questionnaires.
‡11 respondents did not answer the question.
The mean age of the surgeons was 45 years. The mean number of trichiasis surgeries per year among active surgeons was 22.3 (SD 48.1) and the median was 7. Table 2 shows the productivity according to various factors. Having the service near the population by stationing trichiasis surgeons in rural dispensaries or health centres did not predict productivity; however, conducting outreach was an important predictor of productivity.
Table 2 Factors associated with productivity.
| Variable | n | Mean (SD) | Median | p Value |
|---|---|---|---|---|
| <40 years old | 23 | 23.5 (39.7) | 7 | 0.99 |
| ⩾40 years old | 65 | 22.75 (53.1) | 7 | |
| Male | 55 | 26 (58) | 8 | 0.58 |
| Female | 40 | 17 (29.5) | 5 | |
| Work at mission hospital | 11 | 19.8 (27.8) | 6 | 0.37 |
| Work at government facility | 84 | 22.6 (50.3) | 7 | |
| Work at hospital | 69 | 25.7 (53.9) | 8 | 0.16 |
| Work at dispensary or clinic | 26 | 13.2 (25.6) | 6 | |
| Ophthalmic trained | 71 | 24.6 (53.3) | 8 | 0.61 |
| Non‐ophthalmic trained | 24 | 15.6 (27.5) | 7 | |
| Access to consumables incomplete | 78 | 18.5 (31.1) | 6 | 0.21 |
| Access to consumables complete | 17 | 39.7 (92.5) | 16 | |
| Works ⩽3 days/week in eye care | 40 | 19.3 (28.9) | 9 | 0.53 |
| Works >4 days/week in eye care | 47 | 25 (61.1) | 7 | |
| TT surgical set incomplete* | 24 | 4.6 (5.9) | 2 | 0.057 |
| TT surgical set complete | 29 | 28.3 (42.1) | 11 | |
| Knows supervisor | 69 | 22 (33.42) | 8 | 0.058 |
| Does not know supervisor | 26 | 23.2 (75.25) | 2 | |
| Conducts outreach activities | 40 | 39.7 (68.1) | 17 | <0.001 |
| Does not conduct outreach activities | 55 | 9.7 (17.1) | 2 |
TT, trachomatous trichiasis.
*Owing to a printing error, this question was omitted from 42 questionnaires.
Table 3 shows the association of various factors with which surgeons conducted outreach activities. Trachomatous trichiasis surgeons who had a complete instrument set and who knew their supervisors were more likely to conduct outreach activities, with odds ratios of 3.69 (95% confidence interval (CI) 1.14 to 12.0) and 3.14 (95% CI 1.12 to 8.81), respectively.
Table 3 Factors associated with conducting outreach activities.
| Conducts outreach | OR (95% CI) | p Value | ||
|---|---|---|---|---|
| Yes | No | |||
| Male | 22 | 33 | 0.81 (0.36 to 1.86) | 0.67 |
| Female | 18 | 22 | ||
| ⩽45 years | 16 | 30 | 0.58 (0.25 to 1.36) | 0.28 |
| >45 years | 21 | 23 | ||
| Work at private facility | 3 | 8 | 0.48 (0.12 to 1.92) | 0.34 |
| Work at government facility | 37 | 47 | ||
| Work at hospital level | 29 | 40 | 0.99 (0.4 to 2.46) | 1 |
| Work at dispensary or clinic | 11 | 15 | ||
| Work ⩽3 days/week in eye care | 17 | 23 | 1 (0.43 to 2.34) | 1 |
| Work >3 days/week in eye care | 20 | 27 | ||
| TT surgical set complete* | 16 | 13 | 3.69 (1.14 to 12) | 0.049 |
| TT surgical set incomplete | 6 | 18 | ||
| Access to consumables complete | 11 | 6 | 3.1 (1.04 to 9.27) | 0.056 |
| Access to consumables incomplete | 29 | 49 | ||
| Knows supervisor | 34 | 35 | 3.14 (1.12 to 8.81) | 0.034 |
| Does not know supervisor | 6 | 20 | ||
TT, trachomatous trichiasis.
*Owing to a printing error, this question was omitted from 42 questionnaires.
The focus group discussions showed a clear consensus on some issues as follows:
Surgeons agreed that there are many patients who need surgery, but they do not have access to services because the surgeons do not have support to conduct outreach activities.
Surgeons agreed that local health management teams do not consider trichiasis surgery a priority and thus do not allocate financial support for it.
Surgeons believed that they are competent to identify and operate on patients with trichiasis.
Surgeons agreed that lack of instruments and supplies are problems in some areas, and contribute to low productivity.
Surgeons agreed that the duration of the training should be longer and include more practical work, and that refresher training is desirable.
There was disagreement on whether patients are willing to undergo surgery; a number of reasons were cited as to why they are not, including fear, traditional beliefs and worry about fees.
The issue of surgeons' willingness to perform surgery was coloured by a perceived lack of financial support for outreach and incentives to work and lack of regular supervision; however, there was no suggestion that they do not like the work.
Discussion
The two most striking findings are the overall low productivity (half performed <7 surgeries per year) and the large variability in productivity. This may be compared with the MoH target of 15–20 surgeries per month.4 Only 1 surgeon averaged as many as 15 surgeries per month; 9 (9%) reported that they had not performed any surgeries since completion of training. The large variability suggests that specific factors might be responsible for productivity.
Looking at productivity according to specific factors, the most important was whether the surgeon conducted outreach activities in the past year. As with cataract surgical services, it seems that, at this time, programmes in Africa must be prepared either to go out into the community to reach patients or to develop community‐based efforts to allow patients to reach services if we expect to reach VISION 2020 targets.5 Placing trichiasis surgeons at the lowest level (health centres and dispensaries) does not guarantee patients' access to the service.
Dovlo6 has described some of the factors that lead to wastage of human resources in healthcare in Africa. “Indirect” wastage is common and manifests as low productivity owing to misapplied skills, poor support and poor supervision. We have noted a tendency for health workers and their supervisors to regard all training as beneficial and desirable without consideration of whether they will be in a position to use the training or receive support. This was illustrated by the focus group consensus that refresher training would be desirable even though current training is not being used. Training may be wasted because of lack of management systems to provide adequate supervision and supplies after training, as suggested in this data, or inappropriate choice of candidates for training. Selection based on seniority or personal relationships rather than proved or tested capability is likely to result in wasted resources. Increased training of health workers without careful planning to ensure they will be used will result in further wastage of human resources.
Our findings showed another example of the indirect wastage Dovlo describes, which is poor supervision. A trichiasis surgeon's ability to name a supervisor was associated with productivity. In another study in Tanzania, 22% of patients with trichiasis who required surgery failed to get it because the surgeon was away from his station when the patient went to the health facility (companion paper 103374 under revision). Proper supervision would help ensure that posts are covered.
The focus group discussion consensus that lack of support after training, in terms of instrument, supplies, supervision and support for outreach activities is an obstacle to productivity supports the quantitative data we collected.
There are limitations to this study. We have only examined productivity, and have no information on the quality of surgery. In addition, poor outcomes noted in Tanzania7 are likely to reduce acceptance of surgery. Our inability to show statistically significant associations with more factors and productivity may be due to the complexity of issues contributing to productivity. The findings of such low productivity and such great variability, however, ought to encourage more research into this problem. Human and financial resources are scarce in Africa; we will only achieve VISION 2020 targets if we use them wisely.
Acknowledgements
We thank the trichiasis surgeons who contributed information and Helen Keller International, the International Trachoma Initiative and the Tanzania Ministry of Health for cooperation with this study.
Abbreviations
BTRP - bilamellar tarsal plate rotation
MoH - Ministry of Health
Footnotes
Competing interests: None declared.
References
- 1.West S K. Blinding trachoma: prevention with the safe strategy. Am J Trop Med Hyg 200369(Suppl)18–23. [DOI] [PubMed] [Google Scholar]
- 2.Reacher M, Foster A, Huber J. Trichiasis surgery for trachoma. The bilamellar tarsal rotation procedure. WHO/PBL/93.29. 1998
- 3.Helen Keller International Community‐based trichiasis surgery. New York: HKI, 1999
- 4.Ministry of Health Guidelines for bilamellar tarsal rotation procedure (BTRP) training and service delivery. United Republic of Tanzania: MoH, 20046
- 5.Lewallen S, Roberts H, Hall A.et al Increasing cataract surgery to meet Vision 2020 targets; experience from two rural programmes in east Africa. Br J Ophthalmol 2005891237–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dovlo D. Wastage in the health workforce: some perspectives from African countries. Hum Resour Health 200536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.West E S, Mkocha H, Munoz B.et al Risk factors for postsurgical trichiasis recurrence in a trachoma‐endemic area. Invest Ophthalmol Vis Sci 200646447–453. [DOI] [PubMed] [Google Scholar]