Abstract
Background
Studies of distance stereoacuity in intermittent exotropia suggest that normal stereoacuity corresponds to good control of the deviation and that reduced or negative stereoacuity signifies poorer control.
Aim
To evaluate distance stereoacuity in intermittent exotropia using the Frisby Davis Distance stereo test (FD2).
Methods
Children with intermittent exotropia where the near angle was less than or equal to distance were eligible for recruitment. Standardised prospective data collection included FD2 distance stereoacuity. This was a longitudinal study in which outcomes are reported for baseline, last follow‐up (⩾6 months before any surgery) or preoperative and last postoperative visits for those undergoing surgery.
Results
110 children with intermittent exotropia had FD2 stereoacuity tested at baseline: 70 comprehended the test. Mean (standard deviation (SD)) age was 4.6 (1.7) years (range 2–10 years). 41/70 (59%) showed positive responses: mean (SD) stereoacuity 30 (12) s of arc. The mean follow‐up period before any surgery was 13 months (range 6–27 months). At follow‐up, mean (SD) stereoacuity was 24 (11) s of arc. Preoperative and postoperative stereoacuity were not significantly different from those not undergoing surgery.
Conclusion
This study was the first to report distance stereoacuity in intermittent exotropia using the FD2 stereo test: patients with intermittent exotropia can achieve normal levels of distance stereoacuity, but a considerable proportion, despite comprehending, showed a negative response. This suggests that using the FD2, distance stereoacuity in intermittent exotropia is either absent or normal rather than reduced. Possible reasons for this and its implications are discussed.
Stereopsis is generated by the fusion of horizontally disparate retinal images,1 and is considered the highest standard of binocular vision.2 Near stereoacuity assessment has long been an intrinsic part of assessing binocular vision: distance stereoacuity is measured less commonly, and features principally in the assessment of intermittent exotropia.
Intermittent exotropia is a common form of intermittent strabismus,3,4 in which assessment of severity is based on the ease with which binocular control is maintained. As stereoacuity provides a measure of the quality of binocular vision, it may provide a useful objective measure of control and therefore severity in intermittent exotropia.
Previous studies of distance stereoacuity in intermittent exotropia (using the Binocular Visual Acuity Test (BVAT) Mentor)5 suggest that normal stereoacuity corresponds to good control,6,7 reduced stereoacuity to poorer control6 and decreasing stereoacuity to increasing severity.6,7,8,9,10 However, the BVAT Mentor is difficult to use in small children and is no longer commercially available. This study aimed to evaluate distance stereoacuity in intermittent exotropia using the Frisby Davis Distance stereo test (FD2)11 to:
establish the characteristics of distance stereoacuity measured with the FD2,
identify change in stereoacuity over time,
compare preoperative responses to those in childen not undergoing surgery and
report postoperative stereoacuity.
Methods
The study was undertaken as part of a prospective multicentre pilot observational study conducted with approval from the UK North West Multi Centre Research and Ethics Committee, and in accordance with the tenets of the Declaration of Helsinki.
Patients eligible for inclusion were <11 years of age, with intermittent exotropia where the near angle was less than or equal to the distance on the alternating prism cover test. Coexisting ocular pathology (excluding refractive error) was excluded.
Data collected included Frisby and FD2 stereoacuity, alternating prism cover test and distance control using the Newcastle Control Score (NCS).12 Outcomes were assessed at baseline, last follow‐up (⩾6 months before any surgical intervention) or preoperatively and postoperatively.
FD2 stereoacuity was measured using the protocol provided with the test, establishing comprehension by performing the test at 1 m. Failure to respond at this distance was classified as “non‐comprehension”. Those able to comprehend were tested at 6 m, and the disparity progressively reduced until threshold could be determined by three correct responses. Those unable to respond at 6 m were classified as “negative”. Mean and median values were analysed and mean values were reported if the data were normally distributed. Comparison of means for statistical significance was made using the t test.
Results
A total of 110 children were assessed with the FD2 at baseline; 70 were able to comprehend and respond at 6 m (mean (standard deviation (SD)) age 4.6 (1.7) years; range 2–10 years): 46 (66%) were female. This group was significantly older than those unable to comprehend (mean age 2.4 years; p<0.001).
Baseline responses
Positive responses were obtained in 41/70 (59%); mean (SD) stereoacuity 30 (12) s of arc; 29/70 (41%) were negative. Table 1 summarises the age, near stereo, distance angle and distance control. The mean (SD) age of the negative responders was not significantly different from the positive responders (4.3 (1.6) and 4.8 (1.7) years, respectively; p = 0.21). Distance control on NCS showed significantly poorer mean (SD) control for the negative responders than for the positive responders (1.8 (0.4) and 1.6 (0.5), respectively; p = 0.024).
Table 1 Baseline characteristics of positive and negative responders to Frisby Davis Distance stereo test at 6 m.
| Mean (SD) age (years) | Mean (SD) near stereo (Frisby) | Mean (SD) distance angle (APCT) | Mean (SD) distance control (NCS) | |
|---|---|---|---|---|
| Negative, n = 29/70 | 4.3 (1.6) | 164 (106) | 31 (9) | 1.8 (0.4) |
| Positive, n = 41/70 | 4.8 (1.7) | 120 (103) | 31 (9) | 1.6 (0.5) |
| Significance (p value) | 0.21 | 0.12 | 0.95 | 0.024 |
APCT, alternating prism cover test; NCS, Newcastle Control Score.
Change over follow‐up period
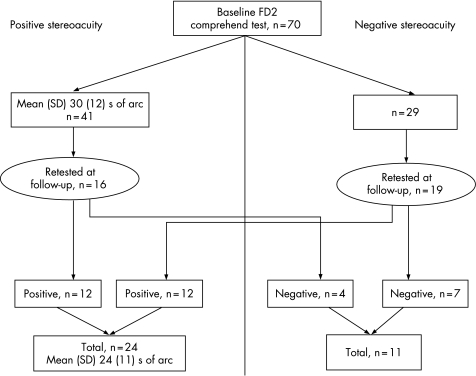
At ⩾6 months follow‐up (mean 13 months; range 6–27 months) before any surgical intervention, FD2 stereoacuity was reassessed in 35/70 patients. Figure 1 shows the changes from baseline to follow‐up. In all, 24/35 (69%) were positive at follow‐up, with a mean (SD) stereoacuity of 24 (11) s of arc; 12/35 (34%) were positive at both baseline and follow‐up; 16/41 who were positive at baseline were retested at follow‐up, and 4/16 (25%) became negative; 19/26 who were negative at baseline were retested at follow‐up, and 12/19 (63%) became positive (p = 0.077).
Figure 1 Frisby Davis Distance Stereo Test stereoacuity values at baseline and ⩾6 months follow‐up.
Preoperative and non‐surgical responses
FD2 was comprehended by 15 patients preoperatively; 11/15 were positive: mean (SD) stereoacuity 28 (13) s of arc compared with 26 (11) s of arc in those not undergoing surgery (n = 39; p = 0.56). The proportion of negative responses was also comparable: 4/15 (27%) preoperatively and 18/57 (32%) in the non‐surgical cohort (p = 0.71; table 2).
Table 2 Frisby Davis Distance stereo test stereoacuity in patients before operation and in those not undergoing surgery.
| Positive: mean (SD) seconds of arc | Negative | |
|---|---|---|
| Preoperative, n = 15 | 28 (13), n = 11, 73% | n = 4, 27% |
| No surgery, n = 57 | 26 (11), n = 39, 68% | n = 18, 32% |
| Statistical significance (p value; t test) | 0.56 | 0.71 |
Postoperative results
Seven patients performed FD2 preoperatively and postoperatively. The mean (range) postoperative follow‐up was 12 (7–24) months; 2/7 (29%) patients tested negative both preoperatively and postoperatively; 5/7 tested positive preoperatively and postoperatively: mean (SD) 24 (11) and 24 (6.5) s of arc, respectively (p = 1). Postoperative results were comparable with those found for all patients with ⩾6 months of follow‐up in the non‐surgical group; 26 (11) s of arc (n = 39; table 3).
Table 3 Preoperative and postoperative and non‐surgical Frisby Davis Distance stereo test values.
| Negative | Positive: mean (SD) seconds of arc | |
|---|---|---|
| Preoperative | n = 2/7, 29% | n = 5/7, 71%; 24 (11) s |
| Postoperative | n = 2/7,* 29% | n = 5/7,* 71%; 24 (6.5) s |
| Non‐surgical | n = 18/57, 32% | n = 39/57, 68%; 26 (11) s |
*Same patients as in the preoperative group.
Discussion
Distance stereoacuity provides a useful means of assessing distance sensory visual function in conditions such as intermittent exotropia where binocular cooperation is compromised. This study is the first to report distance stereoacuity in intermittent exotropia using the FD2 test, and shows that although some children can achieve normal levels,13 a marked proportion showed a negative response. Although age can influence outcomes in young children,14,15 we found no marked differences in age between positive and negative responders. The incidence of negative responses in a study of visually normal children of comparable age was markedly lower (7%),13 indicating that negative responses on distance stereoacuity testing in children with intermittent exotropia are not due to immaturity. Our findings suggest that using the FD2, distance stereoacuity in intermittent exotropia is either absent or normal. This is in contrast with two previous studies, which showed reduced levels of distance stereopsis in patients with intermittent exotropia using the BVAT Mentor.6,16 One explanation for the reported difference between our results and those of Stathacopoulos et al6 and O'Neal et al16 is that they allocated a nominal value of 400 s of arc to patients with no distance stereoacuity: in the study by O'Neal et al, this applied to 16/20 patients (BVAT random dot E test) who had no measurable distance stereoacuity preoperatively and to 9 patients postoperatively. We believe that the allocation of a nominal value to an absence of distance stereoacuity in this way could obscure the true situation.
It may be that finding absent rather than reduced stereoacuity reflects a difference between the FD2, BVAT and AO Vectograph tests: the maximum disparity measurable on the FD2 at 6 m is 50 s of arc compared with 240 and 480 s of arc on the BVAT and AO Vectograph, respectively. It is possible that if the subjects in our study had been tested at greater disparities, the negative responses would decrease and the mean stereoacuity would increase. However, when data from these studies are extrapolated, we can see trends that support our suggestion: Stathacopoulos et al6 found negative responses in 25% of subjects (n = 11/44) on BVAT circles and 55% (n = 24/44) on the BVAT random dot; Yildirim et al17 reported 50% negative responses on BVAT circles and Walsh et al18 found 22% (n = 8/36) of negative reponses using the AO Vectograph.18
Monocular cues can be a problem with FD2 testing in older patients,19 but have not been found to affect the younger age group tested in our study. However, some errors may have been associated with monocular cues, but, if present, would make the negative responses an even more relevant finding.
Negative or reduced stereoacuity may correlate to other measures of severity such as angle of deviation and control. Our use of the NCS to quantify control showed some correlation with distance stereoacuity, consistent with Stathacopoulos et al,6 but as in the study by Walsh et al,18 we found no correlation with angle of deviation. The change in test performance over time can be difficult to measure in young children owing to changes in general development and attention; our finding of a decrease in the proportion of negative responses was not statistically significant and may reflect a practice effect. Further studies are needed to better identify changes attributable to maturity and those related to sensory capability.
It has been suggested that reduced distance stereoacuity may provide an objective indication for surgery.6,10,16,17 The patients in this study were not randomised, but it is interesting to note that there was no difference in distance stereoacuity, or the proportion of negatives in surgical and non‐surgical cohorts.
Our findings suggest that absent rather than reduced distance stereoacuity may be a feature of intermittent exotropia, but the usefulness of this as an objective measure of severity remains unclear. Immeasurable or negative stereoacuity may be a feature of a subgroup of patients with more significantly impaired binocular co‐operation, reflected in clinically significant reductions in BVA18 and loss of central fusion.17 Further work to establish whether or not distance stereoacuity correlates to other clinical measures of severity, such as angle of deviation and control, will help us understand its role in the management of intermittent exotropia.
Acknowledgements
We thank Professor John Frisby and Dr Helen Davis, developers of the FD2, for their help and advice.
Footnotes
This study was supported by the Newcastle Healthcare Charity.
Competing interests: None.
References
- 1.Bishop P. Binocular vision. In: HW Moses RA, ed. Adler's Physiology of the Eye. St Louis: CV Mosby, 1987619–689.
- 2.Westheimer G. Seeing depth with two eyes: stereopsis. Proc R Soc London 1994257205–214. [DOI] [PubMed] [Google Scholar]
- 3.Graham P. Epidemiology of strabismus. Br J Ophthalmol 197458224–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Govidan M, Mohney B G, Diehl N N.et al Incidence and types of childhood exotropia: a population‐based study. Ophthalmology 2005112104–108. [DOI] [PubMed] [Google Scholar]
- 5.Zanoni D, Rosenbaum A. A new method for evaluating distance stereoacuity. J Pediatr Ophthalmol Strabismus 199128255–260. [DOI] [PubMed] [Google Scholar]
- 6.Stathacopoulos R, Rasenbaum A L, Zanoni D.et al Distance stereoacuity: assessing control in intermittent exotropia. Ophthalomology 1993100495–500. [DOI] [PubMed] [Google Scholar]
- 7.Rosenbaum A. Exodeviations. Current concepts in paediatric ophthalmology and strabismus. Ann Arbor, MI: University of Michigan, 1993
- 8.Rosenbaum A. John Pratt‐Johnson lecture: evaluation and management of intemittent exotropia. Am Orthopt J 19964694 [Google Scholar]
- 9.Von Noorden G, Campos E C. Binocular Vision and Ocular Motility: Theory and Management of Strabismus. 6th Ed, Chapter 17. St Louis: Mosby‐Year Book, 367
- 10.Rosenbaum A, Stathacopoulos R. Subjective and objective criteria for recommending surgery in Intermittent exotropia. Am Orthopt J 19924246 [Google Scholar]
- 11.Davis H, Frisby J, Walters B.The Frisby Davis Distance Stereotest (FD2). Florence, Italy: European Strabismological Association, 2001
- 12.Haggerty H, Richardson S, Hrisos S.et al A new method of grading the severity of intermittent distance exotropia. Br J Ophthalmol 200488233–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adams W E, Hrisos S, Richardson S.et al Frisby‐Davis (FD2) distance stereoacuity values in visually normal children. Br J Ophthalmol 2005891438–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simons K. Stereoacuity norms in young children. Arch Ophthal 198199439–445. [DOI] [PubMed] [Google Scholar]
- 15.Oduntan A, Al‐Ghamdi M, Al‐Dosari H. Randot stereoacuity norms in a population of Saudi Arabian children. Clin Exp Optom 199881193–197. [DOI] [PubMed] [Google Scholar]
- 16.O'Neal T, Rosenbaum A, Stathacopoulos R. Distance stereo acuity improvement in intermittent exotropic patients following strabismus surgery. J Pediatr Ophthalmol Strabismus 199532353–357. [DOI] [PubMed] [Google Scholar]
- 17.Yildirim C, Mutlu F M, Chen Y.et al Assessment of central and peripheral fusion and near and distance tereoacuity in sntermittent exotropic patients before and after strabismus surgery. Am J Ophthalmol 1999128222–230. [DOI] [PubMed] [Google Scholar]
- 18.Walsh L, Laroche G, Tremblay F. The use of binocular visual acuity in the assessment iof ntermittent exotropia. J AAPOS 20004154–157. [PubMed] [Google Scholar]
- 19.Holmes J, Fawcett S. Testing distance stereoacuity with the Frisby‐Davis 2 (FD2) test. Am J Ophthalmol 2005139193–195. [DOI] [PubMed] [Google Scholar]