Abstract
Aim
To investigate the influence of tilt and decentration of scleral‐sutured intraocular lenses (IOLs) on ocular higher‐order wavefront aberrations.
Methods
In 45 eyes of 36 patients who had undergone scleral suture fixation of posterior chamber IOL, tilt and decentration of IOLs were determined by Scheimpflug videophotography, and higher‐order aberration for a 4‐mm pupil was measured using the Hartmann–Shack aberrometer. In another 100 eyes of 100 patients after standard cataract surgery with posterior chamber IOL implantation, ocular higher‐order aberration was measured.
Results
In eyes with scleral‐sutured IOL, the mean (SD) tilt angle and decentration were 4.43° (3.02°) and 0.279 (0.162) mm, respectively. Ocular coma‐like aberration in the sutured IOL group was 0.324 (0.170) µm, which was significantly greater than that of the standard cataract surgery group (0.169 (0.061) µm, p<0.001, Student's t test). No significant difference was found in ocular spherical‐like aberration between the sutured IOL group (0.142 (0.065) µm) and standard surgery group (0.126 (0.033) µm; p = 0.254). In the sutured IOL group, IOL tilt significantly correlated with ocular coma‐like aberration (Pearson's correlation coefficient r = 0.628, p<0.001), but no significant correlation was found between IOL tilt and ocular spherical‐like aberration (r = 0.222, p = 0.175). The IOL tilt did not correlate with corneal coma‐like (r = 0.289, p = 0.171) and spherical‐like (r = 0.150, p = 0.356) aberrations. The IOL decentration did not correlate with any higher‐order aberrations.
Conclusion
In eyes with scleral‐sutured posterior chamber IOL, tilting of the lens induces considerable amount of ocular coma‐like aberrations.
Proper positioning and on‐axis alignment of an intraocular lens (IOL) are critical in obtaining satisfactory quality of vision after cataract surgery. Patients with tilted or decentred IOLs may be unhappy with the results of otherwise successful cataract surgery. In fact, malposition of an IOL is one of the leading indications for removal, exchange or repositioning of a posterior chamber IOL.1,2,3,4,5
Malposition of the IOL comprises decentration and tilt. Although it has been known that decentration of the IOL can cause unwanted optical image or dysphotopsia,6,7,8,9,10 the influence of major IOL tilting on the optical quality of the eye has never been reported. With expanding indications of cataract surgery, more complicated cases will undergo cataract removal and IOL implantation procedures, which would increase the risk of IOL misalignment after surgery. Patients tend to have longer longevity after surgery, which might further increase the risk of postoperative events. The optical performance of IOLs in the presence of displacement has been an important issue even in modern cataract surgery.11,12,13,14,15 We conducted the current retrospective study to assess the influence of tilting and decentration of scleral‐sutured posterior chamber IOLs on ocular higher‐order aberrations.
Patients and methods
Patients
Forty five eyes of 36 patients (16 men and 20 women) who had undergone scleral suture fixation of a posterior chamber IOL were included. Their age ranged from 46 to 87 years (mean (standard deviation, SD)) 66.3 (14.2) years). The scleral‐sutured IOLs were hydrophobic acrylic foldable IOL (MA60AC, AcrySof, Alcon Laboratories, Fort Worth, Texas, USA) in 18 eyes and polymethylmethacrylate IOL in 19 eyes, but details were not available in the remaining 8 eyes. Another 100 eyes of 100 patients (41 men and 59 women) after standard cataract surgery with in‐the‐bag implantation of hydrophobic acrylic foldable IOL (MA60AC) served as age‐matched controls, ranging in age from 48 to 88 years (64.5 (13.5) years). The research protocol had institutional review board approval, and written informed consent was obtained from each patient. The study adhered to the tenets of the Declaration of Helsinki.
Examinations
In the scleral‐sutured IOL group, tilt and decentration of IOLs as well as higher‐order wavefront aberration were measured. In the standard cataract surgery group, higher‐order wavefront aberration of the eye was measured.
Tilt and decentration of IOLs were determined by an anterior eye segment analysis system (EAS‐1000; NIDEK, Gamagori, Aichi, Japan).16,17,18 The EAS‐1000 system consists of a Scheimpflug CCD video camera unit and an image analysis computer. The online computer included a special software package to quantitate the length of the decentration and the degree of the tilt.16,17,18 Two Scheimpflug images of the IOL after full mydriasis were taken at slit angles of 45° and 135° by the CCD camera. After geometric correction, the weakly exposed original images were then enhanced further using binarisation and curve‐fitting techniques. Next, by plotting the anterior surface of the IOL as well as the corneal surface on these images, the tilt angle of the IOL optic axis relative to the cornea vertex was quantified by the image analysis computer. The length of decentration was indicated by the distance of the IOL optic axis from the corneal vertex. The data of the two different Scheimpflug images were analysed in a three‐dimensional manner.
Corneal and ocular wavefront aberrations for a 4‐mm pupil were measured using the Hartmann–Shack wavefront aberrometer (Topcon, Tokyo, Japan).19,20,21 The light source of the wavefront sensor is an infrared super luminescent diode laser (λ = 840 nm; the spectral full‐width at half‐maximum = 14 nm; power at the cornea = 20 μW). Reflected light from the point image was led to a Hartmann–Shack wavefront sensor by a lens system. The Hartmann–Shack wavefront sensor consists of 169 small lenses (square shape, edge = 0.6 mm) aligned in a grid on a Hartmann plate and a cooled charge‐coupled device (pixel size = 9 μm). All of the Hartmann images were revised to the pupil‐centre images. The obtained data were expanded into the set of orthogonal Zernike polynomials. The root‐mean squares of third‐order Zernike components (Z3−3 to Z33) were used to represent coma‐like aberration and root‐mean squares of fourth‐order Zernike components (Z4−4 to Z44) were used to represent spherical‐like aberrations.22,23,24
Results
The average mean (SD) tilt angle and decentration of scleral‐sutured IOLs were 4.43° (3.02°) and 0.279 (0.162) mm, respectively. The amounts of ocular coma‐like and spherical‐like aberrations in the eyes with sutured IOL were 0.324 (0.170) and 0.142 (0.065) µm, respectively. The ocular coma‐like aberration in the sutured IOL group was significantly greater than that of the standard cataract surgery group (0.169 (0.061) µm, p<0.001, Student's t test). No significant difference was observed in the ocular spherical‐like aberration between the sutured IOL group and the standard cataract surgery group (0.126 (0.033) µm; p = 0.254).
The amounts of corneal coma‐like and spherical‐like aberrations in the eyes with sutured IOL were 0.192 (0.116) and 0.097 (0.096) µm, respectively. The amounts of corneal coma‐like and spherical‐like aberrations in the standard cataract surgery group were 0.153 (0.095) μm and 0.072 (0.054) µm, respectively. Corneal aberrations did not differ considerably between the sutured IOL and standard cataract surgery groups.
Among the sutured IOL group, there was no significant difference in the amount of tilt, decentration, and ocular and corneal aberrations between the hydrophobic acrylic foldable and polymethylmethacrylate IOL groups.
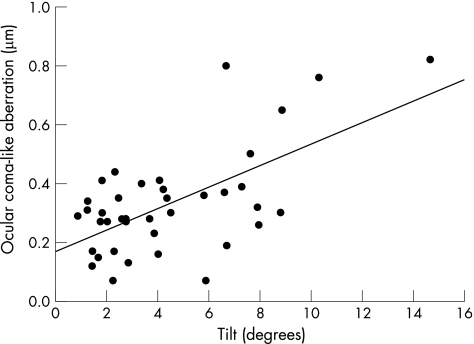
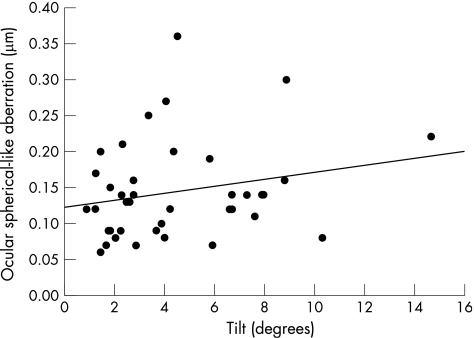
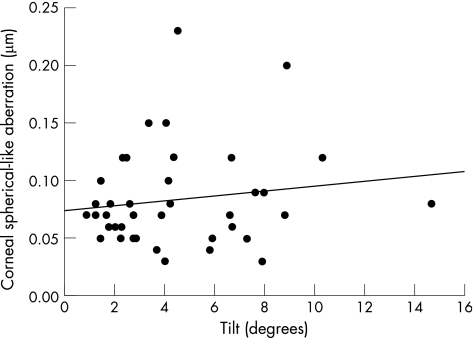
In the sutured IOL group, there was a significant positive correlation between the IOL tilt and ocular coma‐like aberration (Pearson's correlation coefficient r = 0.628, p<0.001; fig 1), but no significant correlation was found between the IOL tilt and ocular spherical‐like aberration (r = 0.222, p = 0.175; fig 2). The IOL tilt did not correlate with corneal coma‐like (r = 0.289, p = 0.171; fig 3) and spherical‐like (r = 0.150, p = 0.356; fig 4) aberrations.
Figure 1 A significant positive correlation was found between the intraocular lens tilt and ocular coma‐like aberration (Pearson's correlation coefficient r = 0.628, p<0.001).
Figure 2 No significant correlation was found between the intraocular lens tilt and ocular spherical‐like aberration (Pearson's correlation coefficient r = 0.222, p = 0.175).
Figure 3 No significant correlation was found between the intraocular lens tilt and corneal coma‐like aberration (Pearson's correlation coefficient r = 0.289, p = 0.171).
Figure 4 No significant correlation was found between the intraocular lens tilt and corneal spherical‐like aberration (Pearson's correlation coefficient r = 0.150, p = 0.356).
The IOL decentration did not correlate with ocular coma‐like (r = 0.123, p = 0.457), ocular spherical‐like (r = −0.067, p = 0.685), corneal coma‐like (r = 0.121, p = 0.456) and corneal spherical‐like (r = −0.187, p = 0.249) aberrations.
Discussion
There have been several studies on the tilt and decentration of IOLs.9,25,26,27,28,29,30,31 In general, modern cataract surgery yields smaller amount of tilt and decentration than the previous surgical procedures. On the other hand, a significant amount of tilt and decentration can sometimes be induced after trans‐scleral suture fixation of IOLs in the absence of capsular support.32,33 Hayashi et al34 reported mean (SD) tilt angle of 6.35° (3.09°) and decentration length of 0.62 (0.31) mm in eyes with scleral suture‐fixed IOLs, which were significantly greater than the values obtained in eyes with in‐the‐bag IOLs, tilt angle of 3.18° (1.66°) and decentration length of 0.29 (0.21) mm. Durak et al35 reported that mean (SD) tilt and decentration of trans‐sclerally sutured posterior chamber IOLs were 6.09° (3.80°) and 0.67 (0.43) mm, respectively. In the current study, we obtained a mean (SD) tilt angle of 4.43° (3.02°) and decentration length of 0.28 (0.16) mm in eyes with sutured IOL, which are favourably compared with the previous data.
In the present study, we found that major tilting of an IOL caused a substantial amount of ocular coma‐like aberration. There was a significant positive correlation between IOL tilt and ocular coma‐like aberration. Ocular spherical‐like aberration, and corneal coma‐like and spherical aberrations did not correlate with the amount of IOL tilt. Similarly, IOL decentration showed no correlation with any ocular or corneal higher‐order aberrations. Recently, there has been a case report of a significant amount of ocular coma‐like aberration caused by major tilting of an IOL, 28.87°, which was successfully treated by IOL repositioning surgery.36 Taketani et al30 reported that IOL tilt of even a small amount, 3.43° (4.55°), significantly correlated with ocular coma‐like aberration.30
As shown in the results, the ocular coma‐like aberration in the sutured IOL group (0.324 (0.170) µm) was significantly greater than that of the standard cataract surgery group (0.169 (0.061) µm). On the other hand, there was no significant difference in the ocular spherical‐like aberration between the sutured IOL group (0.142 (0.065) µm) and the standard cataract surgery group (0.126 (0.033) µm). In eyes after standard cataract surgery with foldable acrylic IOL implantation, the mean (SD) ocular coma‐like and spherical‐like aberrations for 4.0‐mm aperture diameter were reported to be 0.194 (0.081) and 0.144 (0.07) μm, respectively.30 In pseudophakic eyes with acrylic IOLs, ocular coma‐like aberration for a 4‐mm pupil was 0.125–0.15 μm and ocular spherical‐like aberration for a 4‐mm pupil was 0.075–0.082 μm.37 Similar values have been reported for 4‐mm to 5‐mm aperture diameter in eyes after standard cataract surgery with implantation of spherical IOLs,38,39 indicating that coma‐like aberration was remarkably increased in eyes after scleral suture fixation of the IOL.
It would be interesting to know the influence of IOL tilt and coma‐like aberration on visual quality of patients after scleral suture fixation of IOLs. These patients, however, had undergone complicated surgical procedures, which included primary or secondary scleral suture fixation of the IOL, and many of them have other ocular pathologies that affect visual functions. Thus, such evaluation is difficult in this study population. There have been several simulation studies on the visual impairment caused by IOL misalignment.11,12,13 These studies, however, did not consider higher‐order aberrations of human corneas, and therefore exact simulation of situations in living human eyes was rather difficult. In a case report, retinal image simulation of a Landolt ring was conducted using the wavefront aberration profile.36 It was found that major tilt of the IOL resulted in remarkably skewed and blurred Landolt images, which were significantly improved by IOL repositioning surgery.36 Compared with that report, the amount of IOL tilt in the current study was small, but still induced coma‐like aberration may have induced skewed distortion of the object image. The present study alone cannot determine the extent of these changes in human eyes. Future studies are needed to elucidate these points.
Another weakness of this retrospective study is that various types of IOLs were used in the sutured IOL group. This was because of the retrospective nature of the current study. Moreover, surgical details including the type of IOL were not available in several patients, because they had been operated on at different surgical sites. There is a possibility that the differences in IOL design and material resulted in different amount and pattern of ocular wavefront aberrations. Bellucci et al39 have reported, however, that ocular coma‐like aberrations did not differ significantly among various types of IOLs, whereas ocular spherical‐like aberrations were largely affected by the style of IOLs. Thus, we believe that there was little, if any, influence of the type of IOLs on the results of the current study.
Scleral suture fixation of a posterior chamber IOL is one of the surgical procedures used to implant an IOL in eyes with inadequate capsular support.40,41 Other options to correct aphakic eyes in the absence of capsular support include anterior chamber IOL, iris‐sutured posterior chamber IOL and contact lens correction of aphakia. Until now, these alternatives have been compared in terms of safety, efficiency and feasibility. The data obtained in the current study suggest that the influence of these procedures on optical quality of the eye should also be evaluated, making these comparisons more comprehensive and elaborate.
Although the current study was conducted in eyes with scleral suture fixation of IOLs, the findings obtained may have clinical implications in regular cataract surgery. The advent and widespread use of continuous curvilinear capsulorhexis greatly contributed to long‐term centration of IOLs. However, perfect centration of IOLs is rare for many reasons including in–out‐of‐the‐bag placement, incongruence between bag diameter and overall IOL diameter, a large capsulorhexis, asymmetrical capsule coverage, IOL placement in the sulcus, capsule fibrosis, capsule phimosis and radial bag tears.13,42 Even if the IOL is perfectly centred, the other optical components of a human eye are rarely, if ever, centred on the visual axis or on any common axis. A new class of IOLs designed to offset corneal spherical aberration has been recently introduced,43,44,45,46 making the relative alignments of IOLs and other optical components of the eye more important. Further studies in these fields are warranted.
Abbreviations
IOL - intraocular lens
Footnotes
Funding: This study was supported in part by grants‐in‐aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology, Japan.
Competing interests: None.
References
- 1.Obstbaum S A, To K. Posterior chamber intraocular lens dislocations and malpositions. Aust N Z J Ophthalmol 198917265–271. [DOI] [PubMed] [Google Scholar]
- 2.Lyle W A, Jin J C. An analysis of intraocular lens exchange. Ophthalmic Surg 199223453–458. [PubMed] [Google Scholar]
- 3.Auffarth G U, Wilcox M, Sims J C.et al Analysis of 100 explanted one‐piece and three‐piece silicone intraocular lenses. Ophthalmology 19951021144–1150. [DOI] [PubMed] [Google Scholar]
- 4.Carlson A N, Stewart W C, Tso P C. Intraocular lens complications requiring removal or exchange. Surv Ophthalmol 199842417–440. [DOI] [PubMed] [Google Scholar]
- 5.Mamalis N, Davis B, Nilson C D.et al Complications of foldable intraocular lenses requiring explantation or secondary intervention ‐ 2003 survey update. J Cataract Refract Surg 2004302209–2218. [DOI] [PubMed] [Google Scholar]
- 6.Brems R N, Apple D J, Pfeffer B R.et al Posterior chamber intraocular lenses in a series of 75 autopsy eyes. Part III: correlation of positioning holes and optic edges with the pupillary aperture and visual axis. J Cataract Refract Surg 198612367–371. [DOI] [PubMed] [Google Scholar]
- 7.Kumar S, Miller D. Effect of intraocular lens decentration on retinal image contrast. J Cataract Refract Surg 199016712–714. [DOI] [PubMed] [Google Scholar]
- 8.McDonnell P J, Spalton D J, Falcon M G. Decentration of the posterior chamber lens implant: the effect of optic size on the incidence of visual aberrations. Eye 19904132–137. [DOI] [PubMed] [Google Scholar]
- 9.Kozaki J, Tanihara H, Yasuda A.et al Tilt and decentration of the implanted posterior chamber intraocular lens. J Cataract Refract Surg 199117592–595. [DOI] [PubMed] [Google Scholar]
- 10.Subramaniam S, Tuft S J. Early decentration of plate‐haptic silicone intraocular lenses. J Cataract Refract Surg 200127330–332. [DOI] [PubMed] [Google Scholar]
- 11.Korynta J, Bok J, Cendelin J.et al Computer modeling of visual impairment caused by intraocular lens misalignment. J Cataract Refract Surg 199925100–105. [DOI] [PubMed] [Google Scholar]
- 12.Negishi K, Ohnuma K, Ikeda T.et al Visual simulation of retinal images through a decentered monofocal and a refractive multifocal intraocular lens. Jpn J Ophthalmol 200549281–286. [DOI] [PubMed] [Google Scholar]
- 13.Altmann G E, Nichamin L D, Lane S S.et al Optical performance of 3 intraocular lens designs in the presence of decentration. J Cataract Refract Surg 200531574–585. [DOI] [PubMed] [Google Scholar]
- 14.Mutlu F M, Erdurman C, Sobaci G.et al Comparison of tilt and decentration of 1‐piece and 3‐piece hydrophobic acrylic intraocular lenses. J Cataract Refract Surg 200531343–347. [DOI] [PubMed] [Google Scholar]
- 15.Hayashi K, Hayashi H. Comparison of the stability of 1‐piece and 3‐piece acrylic intraocular lenses in the lens capsule. J Cataract Refract Surg 200531337–342. [DOI] [PubMed] [Google Scholar]
- 16.Sasaki K, Sakamoto Y, Shibata T.et al Measurement of postoperative intraocular lens tilting and decentration using Scheimpflug images. J Cataract Refract Surg 198915454–457. [DOI] [PubMed] [Google Scholar]
- 17.Sasaki K, Sakamoto Y, Shibata T.et al The multi‐purpose camera: a new anterior eye segment analysis system. Ophthalmic Res 199022(Suppl 1)3–8. [DOI] [PubMed] [Google Scholar]
- 18.Hayashi K, Harada M, Hayashi H.et al Decentration and tilt of polymethyl methacrylate, silicone, and acrylic soft intraocular lenses. Ophthalmology 1997104793–798. [DOI] [PubMed] [Google Scholar]
- 19.Kuroda T, Fujikado T, Maeda N.et al Wavefront analysis of higher‐order aberrations in patients with cataract. J Cataract Refract Surg 200228438–444. [DOI] [PubMed] [Google Scholar]
- 20.Fujikado T, Kuroda T, Maeda N.et al Light scattering and optical aberrations as objective parameters to predict visual deterioration in eyes with cataracts. J Cataract Refract Surg 2004301198–1208. [DOI] [PubMed] [Google Scholar]
- 21.Tanabe T, Miyata K, Samejima T.et al Influence of wavefront aberration and corneal subepithelial haze on low‐contrast visual acuity after photorefractive keratectomy. Am J Ophthalmol 2004138620–624. [DOI] [PubMed] [Google Scholar]
- 22.Howland H C, Howland B. A subjective method for the measurement of monochromatic aberrations of the eye. J Opt Soc Am 1977671508–1518. [DOI] [PubMed] [Google Scholar]
- 23.Applegate R A, Howland H C, Sharp R P.et al Corneal aberrations and visual performance after radial keratotomy. J Refract Surg 199814397–407. [DOI] [PubMed] [Google Scholar]
- 24.Oshika T, Klyce S D, Applegate R A.et al Changes in corneal wavefront aberrations with aging. Invest Ophthalmol Vis Sci 1999401351–1355. [PubMed] [Google Scholar]
- 25.Auran J D, Koester C J, Donn A. In vivo measurement of posterior chamber intraocular lens decentration and tilt. Arch Ophthalmol 199010875–79. [DOI] [PubMed] [Google Scholar]
- 26.Hayashi K, Hayashi H, Nakao F.et al Intraocular lens tilt and decentration after implantation in eyes with glaucoma. J Cataract Refract Surg 1999251515–1520. [DOI] [PubMed] [Google Scholar]
- 27.Hayashi K, Hayashi H, Nakao F.et al Anterior capsule contraction and intraocular lens decentration and tilt after hydrogel lens implantation. Br J Ophthalmol 2001851294–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim J S, Shyn K H. Biometry of 3 types of intraocular lenses using Scheimpflug photography. J Cataract Refract Surg 200127533–536. [DOI] [PubMed] [Google Scholar]
- 29.Nejima R, Miyata K, Honbou M.et al A prospective, randomised comparison of single and three piece acrylic foldable intraocular lenses. Br J Ophthalmol 200488746–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taketani F, Matuura T, Yukawa E.et al Influence of intraocular lens tilt and decentration on wavefront aberrations. J Cataract Refract Surg 2004302158–2162. [DOI] [PubMed] [Google Scholar]
- 31.Baumeister M, Neidhardt B, Strobel J.et al Tilt and decentration of three‐piece foldable high‐refractive silicone and hydrophobic acrylic intraocular lenses with 6‐mm optics in an intraindividual comparison. Am J Ophthalmol 20051401051–1058. [DOI] [PubMed] [Google Scholar]
- 32.Solomon K, Gussler J R, Gussler C.et al Incidence and management of complications of transsclerally sutured posterior chamber lenses. J Cataract Refract Surg 199319488–493. [DOI] [PubMed] [Google Scholar]
- 33.Gabric N, Henc‐Petrinovic L, Dekaris I. Complications following two methods of posterior chamber intraocular lens suturing. Doc Ophthalmol. 1996–97 92107–116. [DOI] [PubMed] [Google Scholar]
- 34.Hayashi K, Hayashi H, Nakao F.et al Intraocular lens tilt and decentration, anterior chamber depth, and refractive error after trans‐scleral suture fixation surgery. Ophthalmology 1999106878–882. [DOI] [PubMed] [Google Scholar]
- 35.Durak A, Oner H F, Kocak N.et al Tilt and decentration after primary and secondary transsclerally sutured posterior chamber intraocular lens implantation. J Cataract Refract Surg 200127227–232. [DOI] [PubMed] [Google Scholar]
- 36.Oshika T, Kawana K, Hiraoka T.et al Ocular higher‐order wavefront aberration caused by major tilting of intraocular lens. Am J Ophthalmol 2005140744–746. [DOI] [PubMed] [Google Scholar]
- 37.Choi J, Kim T I, Tchah H. Comparison of wavefront aberration after cataract surgery with acrylic intraocular lens implantation. J Cataract Refract Surg 200531324–329. [DOI] [PubMed] [Google Scholar]
- 38.Vilarrodona L, Barrett G D, Johnson B. High‐order aberrations in pseudophakia with different intraocular lenses. J Cataract Refract Surg 200430571–575. [DOI] [PubMed] [Google Scholar]
- 39.Bellucci R, Morselli S, Piers P. Comparison of wavefront aberrations and optical quality of eyes implanted with five different intraocular lenses. J Refract Surg 200420297–306. [DOI] [PubMed] [Google Scholar]
- 40.Stark W J, Gottsch J D, Goodman D F.et al Posterior chamber intraocular lens implantation in the absence of capsular support. Arch Ophthalmol 19891071078–1083. [DOI] [PubMed] [Google Scholar]
- 41.Wagoner M D, Cox T A, Ariyasu R G.et al Intraocular lens implantation in the absence of capsular support: a report by the American Academy of Ophthalmology. Ophthalmology 2003110840–859. [DOI] [PubMed] [Google Scholar]
- 42.Walkow T, Anders N, Pham D T.et al Causes of severe decentration and subluxation of intraocular lenses. Graefe's Arch Clin Exp Ophthalmol 19982369–12. [DOI] [PubMed] [Google Scholar]
- 43.Packer M, Fine I H, Hoffman R S.et al Prospective randomized trial of an anterior surface modified prolate intraocular lens. J Refract Surg 200218692–696. [DOI] [PubMed] [Google Scholar]
- 44.Mester U, Dillinger P, Anterist N. Impact of a modified optic design on visual function: clinical comparative study. J Cataract Refract Surg 200329652–660. [DOI] [PubMed] [Google Scholar]
- 45.Bellucci R, Scialdone A, Buratto L.et al Visual acuity and contrast sensitivity comparison between Tecnis and AcrySof SA60AT intraocular lenses: a multicenter randomized study. J Cataract Refract Surg 200531712–717. [DOI] [PubMed] [Google Scholar]
- 46.Marcos S, Barbero S, Jimenez‐Alfaro I. Optical quality and depth‐of‐field of eyes implanted with spherical and aspheric intraocular lenses. J Refract Surg 200521223–235. [DOI] [PubMed] [Google Scholar]