Abstract
Aim
To determine the prevalence of refractive errors among schoolchildren in urban and rural areas of Dezful County, Iran.
Methods
In a cross‐sectional study, using random cluster sampling, 5721 Dezful schoolchildren were selected from 39 clusters. The participants in the study totalled 5544; 3673 elementary and middle school students and 1871 high school students. For the former group, cycloplegic refraction and for the latter, non‐cycloplegic refraction was tested. In all participants, uncorrected visual acuity and best corrected visual acuity were determined, and those with a visual acuity of 20/40 or worse, underwent a complete ophthalmic examination to determine the cause of visual impairment. A spherical equivalent of −0.5 diopter (D) or worse was defined as myopia, +2.0 D or more was defined as hyperopia, and a cylinder refraction greater than 0.75 D was considered astigmatism.
Results
The uncorrected visual acuity was 20/40 or worse in the better eye of 224 schoolchildren (3.8% of participants). This figure (percentage) was 14 (0.03%) based on their best corrected visual acuity and 96 (1.7%) with their presenting vision. According to results of cycloplegic refraction, 3.4% (95% confidence interval (CI), 2.5 to 4.4) of the primary and middle school students were myopic and 16.6% (95% CI, 13.6 to 19.7) were hyperopic. For high school students, these rates were 2.1% (95% CI, 0.7 to 3.5) and 33.0% (95% CI, 24.9 to 41.1), respectively, with non‐cycloplegic refraction. In the multivariate logistic regression for primary and middle school students, myopia was correlated with age (p = 0.030), and hyperopia was correlated with age (p<0.001) and area of residence (p = 0.007). In high school students, hyperopia again showed a correlation with their area of residence (p = 0.029).
Conclusion
The present study reveals the considerable prevalence rates of refractive errors among schoolchildren in Dezful County and the high rate of an unmet need for their correction. Although myopia is not very prevalent, the high rate of hyperopia in the studied population emphasises its need for attention.
Refractive errors are among the leading causes of visual impairment worldwide and are responsible for high rates of low vision and blindness in certain areas.1 Schoolchildren are considered a high risk group because uncorrected refractive errors can seriously affect their learning abilities,2 and their physical and mental development.3 Studies on the prevalence of refractive errors among children in different parts of the world show significant differences,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19 and population studies concerning refractive errors in children are very limited in the East Mediterranean region.14,15 In our country, Iran, the only published population study is the Tehran Eye Study,20 according to which the prevalence of myopia and hyperopia in children under 15 years of age is 7.2% and 76.2%, respectively, based on cycloplegic refraction.21 The study covers only the urban population, and in light of geographic and socioeconomic diversity, does not reflect the situation in the rest of the country. Such differences over the world show the inadequacy of the present data and studies on the prevalence of refractive errors in different areas, especially in age, gender and ethnicity groups have been recommended.22 For this purpose, the present study was designed and conducted in urban and rural areas of Dezful to determine the prevalence of refractive errors among schoolchildren in this southeastern county of our country, Iran.
Since only a limited number of epidemiologic studies focus on refractive errors and differences among age, gender and ethnic groups, a series of studies4,5,6,7,8,9,10,11 concerning refractive errors in school‐age children have been carried out, based on a single protocol,2 and their results have been published. The present study is in many aspects based on this protocol; its differences will be discussed.
Methods and materials
In this cross‐sectional study on schoolchildren in Dezful County in the 2004–2005 school year, cluster sampling was performed during February and March 2005.
Study population and sample
Dezful, with an area of 4762 square kilometres, is a county in Khuzestan Province in southwest Iran (fig 1). The population is approximately 380 000 (2004) and 44% inhabit rural areas. The study population, schoolchildren in the 2004–2005 school year, numbered 83 250. The distribution of this population in groups based on their grade level, gender and area of residence is shown in table 1. Sampling was performed with a random cluster approach, with 460 schools representing clusters. A total of 5726 students were enrolled after the random selection of 39 schools. The sample size for each grade level, according to the protocol for studying refractive errors in children by Negrel et al,2 was calculated for a prevalence rate of 22% for refractive errors with a 2% error rate and a 95% confidence interval (CI). The design effect and non‐response rate were assumed 1.25 and 10%, respectively. Therefore, the calculated sample size for each grade level was 475 students, with a total of 5700 (7 to 18 year olds) for all 12 grades.
Figure 1 Geographic location of Dezful on the map of Iran.
Table 1 Distribution of the total population of Dezful schoolchildren in the 2004–2005 school year and the study participants in groups of grade level, gender and area of residence.
| Total population of Dezful schoolchildren | Participants | ||
|---|---|---|---|
| No (%) | No (%) | ||
| Grade level | 1 | 6495 (7.8) | 398 (7.2) |
| 2 | 6515 (7.8) | 411 (7.4) | |
| 3 | 6469 (7.7) | 410 (7.4) | |
| 4 | 7181 (8.6) | 484 (8.7) | |
| 5 | 7851 (9.5) | 570 (10.3) | |
| 6 | 8966 (10.7) | 454 (8.2) | |
| 7 | 8197 (9.8) | 425 (7.7) | |
| 8 | 8877 (10.7) | 521 (9.4) | |
| 9 | 8841 (10.6) | 877 (15.8) | |
| 10 | 6618 (8.0%) | 586 (10.6) | |
| 11 | 6061 (7.2) | 281 (5.7) | |
| 12 | 1179 (1.4%) | 127 (2.3) | |
| Gender | male | 43 441 (52.1) | 2440 (44.0) |
| female | 39 809 (47.9) | 3104 (56.0) | |
| Area of residence | urban | 55 840 (67) | 3730 (67.3) |
| rural | 27 410 (33) | 1814 (32.7) | |
| Total | 83 250 | 5544 | |
Examinations
For every student, the visual acuity was tested without correction, with correction and, if applicable, with their spectacles. Objective refraction was determined using a Topcon KR 8000 autorefractometer, (author, please state the country of origin) and ocular motility was evaluated with a cover test at 0.5 and 4.0 metres. For first to eighth graders, cycloplegic refraction was also checked half an hour after instilling a drop of cyclopentolate 1% three times with five minute intervals. All students with an uncorrected visual acuity (UCVA) worse than 20/20 in one eye underwent subjective refraction and best corrected visual acuity (BCVA) tests, and those with a BCVA worse than 20/32 were referred to an ophthalmologist for a complete ophthalmic examination to determine the cause of low vision. During the interview session, students' height and weight were measured, and data concerning their socioeconomic status and history of near work were recorded. Appropriate spectacles were provided by the study for those lacking them.
Definitions
To maintain comparability of our results with those of studies conducted in other parts of the world, the same definitions for refractive errors2 were used: a spherical equivalent of −0.50 D or worse for myopia, and +2.0 D or more for hyperopia. Students with myopia in one or both eyes were classified as myopic, and those with hyperopia in one or both eyes, provided that neither eye was myopic, were classified as hyperopic. Astigmatic students were those with a cylinder refraction of 0.75 D or more in at least one eye, which was recorded with a negative sign.
Students were divided into five groups based on their visual acuity: 20/32 or better in both eyes, 20/32 or better in one eye, 20/40 to 20/63 in the better eye, 20/80 to 20/160 in the better eye, and 20/200 or worse in the better eye. The cause of low vision was determined in those with a vision worse than 20/32, and was recorded as a refractive error when the BCVA could improve to 20/32 or better. When the BCVA was still worse than 20/32, a complete ophthalmic examination was performed and the cause of low vision was recorded in one of the following five categories: corneal opacities, cataract, retinal conditions, amblyopia, or other. In cases of amblyopia, it was necessary to rule out any organic cause, and find one of the following criteria: (1) Esotropia, exotropia, or vertical tropia in four meters, or esotropia or vertical tropia in 0.5 metre (strabismic amblyopia); (2) Anisometropia of 2.0 D or more; (3) Hyperopia of +6.0 D or more. In cases of an uncorrectable low vision with no organic disorder, the amblyopia was categorised as “undefined”.
Tropias were assessed with the cover test and observing the corneal reflex in 0.5 and 4.0 metres and classified in three groups of esotropia, exotropia, and vertical tropia. The degree of tropia was measured using the Hirschberg method of corneal light reflex.
Ethical issues
The study protocol was approved by the Ethical Committee of Tehran University of Medical Sciences. The local school board and school principles also approved the study. Written informed consent from a parent or guardian, in addition to the assent of each student was obtained before examination.
Analysis
The prevalence rates of refractive errors were calculated in the studied population. The design effect was used in computing the error rate and the 95% CI. For ratios, the 95% CIs were calculated using normal distribution. In cases of low proportion that did not follow the normal distribution, binominal distribution was used. All figures were directly standardised according to the grade level and gender distribution rates of Dezful County schoolchildren. Distribution of refractive errors were computed through separate analyses for first to eighth graders and high school students, using objective cycloplegic and objective non‐cycloplegic refractions, respectively. Multivariate logistic regression was applied to assess the association between refractive errors and other factors, using a backward hierarchical elimination approach to create the model.
Results
During the period of this study, February and March 2005, 5726 students were sampled and 5544 participated, accounting for a 96.8% response rate. Table 1 presents the demographic information of the participants in terms of grade level, gender and area of residence (rural or urban), in comparison to those of the total schoolchildren population of Dezful County in the 2004/2005 school year. The distribution rates of grade level and area of residence did not differ greatly, but the gender distribution rates were slightly different between participants and the schoolchildren population. There were 3673 primary and middle school participants, among which 183 students or their parents did not consent to cycloplegia. The remaining 1861 participants were high school students for whom objective non‐cycloplegic refraction was tested.
Visual acuity
Data on participants' visual acuity is presented in table 2. The UCVA was 20/40 or worse in the better eye of 224 (3.8%) students. This figure was 14 (0.3%) according to the BCVA, while the presenting vision was 20/40 or worse in 96 (1.7%) students. Out of 224 schoolchildren with a UCVA of 20/40 or worse in the better eye, 46 (20.5%) did not use spectacles although 32 (69.6%) of them could reach a visual acuity of 20/32 or better with appropriate correction. Visual acuity showed a statistically significant difference between genders (p<0.001); girls were more likely to have a visual acuity of 20/40 or worse (OR = 1.8; 95% CI, 1.1 to 2.9).
Table 2 Distribution of uncorrected, spectacle corrected, presenting, and best corrected visual acuity in each visual acuity group in terms of number, percentage and 95% confidence interval*.
| Visual acuity groups | Uncorrected visual acuity | Spectacle corrected visual acuity | Presenting visual acuity | Best corrected visual acuity |
|---|---|---|---|---|
| 20/32 or better in both eyes | 5141 (92.7%) | 261 (76.6%) | 5238 (95.0%) | 5473 (98.5%) |
| (91.3–94.2) | (71.5–81.8) | (94.0–95.9) | (98.1–99.0) | |
| 20/32 or better in one eye | 170 (3.4%) | 48 (14.7%) | 165 (3.3%) | 57 (1.1%) |
| (2.6–4.1) | (9.9–19.4) | (2.5–4.1) | (0.8–0.15) | |
| 20/40 to 20/63 in the better eye | 124 (2.1%) | 23 (6.6%) | 74 (1.3%) | 6 (0.1%) |
| (1.6–2.7) | (4.1–9.0) | (0.9–1.7) | (0.03–0.23)† | |
| 20/80 to 20/160 in the better eye | 75 (1.2%) | 7 (2.1%) | 16 (0.3%) | 5 (0.1%) |
| (0.6–1.8) | (0.6–3.6) | (0.1–0.5) | (0.05–0.36)† | |
| 20/200 or worse in the better eye | 25 (0.5%) | – | 6 (0.1%) | 3 (0.1%) |
| (0.2–0.8) | (0.05–0.38) | (0.03–0.35)† | ||
| Total sample | 5535 | 339 | 5544 | 5544 |
*Standardised for age and grade level
†The 95% confidence interval was calculated using binominal distribution
The design effect was 0.8 to 4.4
Factors responsible for a UCVA of 20/40 or worse in each or both eyes are summarised in table 3.
Table 3 Causes of low vision in Dezful schoolchildren, defined as a visual acuity of 20/40 or worse.
| Cause | Number (%) of eyes with a visual acuity of 20/40 or worse | Number (%) of children with a visual acuity of 20/40 or worse in one or both eyes† | Prevalence rate of a visual acuity of 20/40 or worse in one or both eyes in the population† | |
|---|---|---|---|---|
| Right eye | Left eye | |||
| Refractive error | 269 (85.4) | 262 (85.1) | 343 (87.3) | 6.13 |
| Amblyopia | 27 (8.6) | 34 (11.0) | 52 (13.2) | 0.91 |
| Corneal opacity | 3 (1.0) | 1 (0.3) | 3 (0.8) | 0.09 |
| Cataract | 2 (0.6) | – | 2 (0.5) | 0.02 |
| Retinal condition | 2 (0.6) | 1 (0.3) | 2 (0.5) | 0.04 |
| Other | 6 (1.9) | 6 (1.9) | 9 (2.3) | 0.17 |
| Undefined | 6 (1.9) | 4 (1.3) | 8 (2.0) | 0.30 |
| Total | 315 (100) | 308 (100) | 393 (100) | 7.24 |
*Standardised for age and grade level
†These figures refer to one or both eyes, thus their totals outnumber total causes.
Refractive error
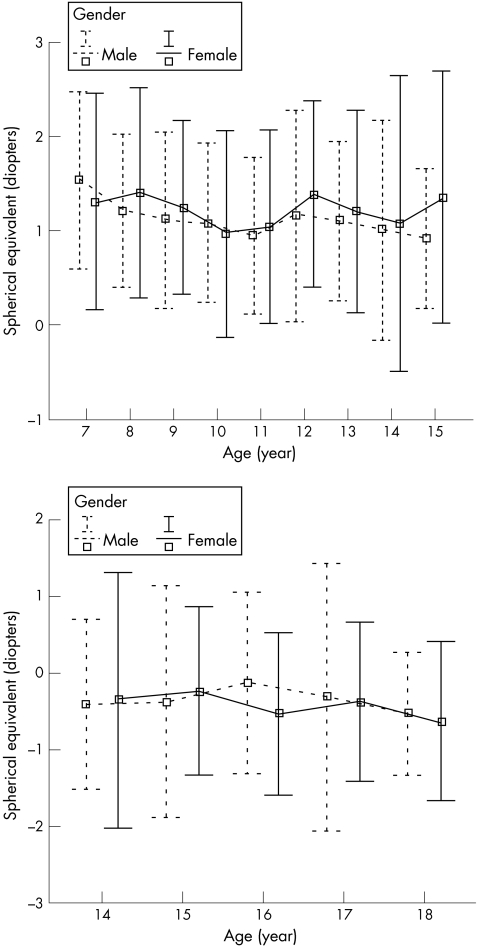
As mentioned earlier, unlike high school students, refraction tests for first to eighth graders were done under cycloplegia. Therefore, refractive results in these two groups are presented separately. The mean spherical equivalent cycloplegic refraction in the right eyes of primary and middle school students was 1.17 D (95% CI, 1.09 to 1.26) and the mean spherical equivalent non‐cycloplegic refraction in the right eyes of high school students was −0.35 D (95% CI, −0.45 to −0.26). Fig 2 demonstrates the differences in the mean spherical equivalent refraction based on the gender and age of primary and middle school students (top) and high school students (bottom). It can be noted that refractive changes in both genders followed a similar trend and were not statistically different. The refraction in first to eighth graders showed a statistically significant decrease with age (p = 0.033). Non‐cycloplegic refraction in high school students was not significantly different among different age groups. Same observations were made on the left eyes, and therefore the data is not presented here. The rate of myopia, hyperopia, and astigmatism in these two student groups are presented in tables 4 and 5, by age, gender and area of residence.
Figure 2 Distribution of spherical equivalent refraction with cycloplegia in primary and middle school students (top) and without cycloplegia in high school students (bottom) by age and gender.
Table 4 Prevalence (95% CI) of myopia, hyperopia, and astigmatism, according to cycloplegic refraction, among primary and middle school students and their distribution in groups of age, gender and area of residence*.
| Number | Myopia | Hyperopia | Astigmatism | |
|---|---|---|---|---|
| Age (years) | ||||
| 7 | 366 | 2.5 (0.7–4.4) | 28.9 (22.6–35.2) | 20.9 (15.5–26.3) |
| 8 | 398 | 2.6 (0.1–5.0) | 22.7 (16.4–28.9) | 20.1 (13.3–26.9) |
| 9 | 348 | 2.6 (0.6–4.7) | 16.7 (12.0–21.4) | 20.4 (14.7–26.0) |
| 10 | 439 | 2.4 (0.5–4.3) | 12.4 (7.9–17.0) | 18.6 (14.0–23.3) |
| 11 | 489 | 4.0 (1.9–6.1) | 12.9 (8.3–17.5) | 19.8 (16.2–23.4) |
| 12 | 459 | 3.5 (1.9–5.2) | 16.9 (12.3–21.5) | 16.9 (11.6–22.2) |
| 13 | 502 | 3.8 (2.2–5.3) | 14.1 (10.6–17.6) | 16.4 (12.3–20.6) |
| 14 | 308 | 5.1 (1.8–8.3) | 13.0 (9.8–16.1) | 18.0 (11.7–24.2) |
| 15 | 120 | 4.9 (0.8–9.0) | 10.3 (1.5–19.1) | 20.2 (12.8–27.6) |
| Gender | ||||
| Male | 1604 | 3.1 (1.9–4.3) | 16.1 (11.0–21.1) | 18.5 (15.5–21.5) |
| Female | 1886 | 3.7 (2.3–5.2) | 17.3 (14.3–20.4) | 18.9 (14.6–23.2) |
| Area of residence | ||||
| Urban | 2341 | 3.7 (2.7–4.7) | 13.8 (10.9–16.8) | 21.0 (18.5–23.5) |
| Rural | 1149 | 2.9 (1.1–4.8) | 21.4 (16.8–25.9) | 14.8 (10.6–19.0) |
| Total | 3490 | 3.4 (2.5–4.4) | 16.6 (13.6–19.7) | 18.7 (16.1–21.2) |
* Percentage (95% CI) standardised for age and grade level.
The design effect was 0.84 to 5.7.
Table 5 Prevalence (95% CI) of myopia, hyperopia, and astigmatism, according to non‐cycloplegic refraction, among high school students and their distribution in groups of age, gender and area of residence*.
| Number | Myopia | Hyperopia | Astigmatism | |
|---|---|---|---|---|
| Age (years) | ||||
| 14 | 352 | 34.4 (27.0–41.8) | 1.6 (0.4–2.8) | 18.8 (15.9–21.7) |
| 15 | 619 | 33.2 (28.4–38.1) | 0.9 (0.2–3.5)† | 17.3 (13.7–21.0) |
| 16 | 505 | 32.6 (18.3–46.9) | 3.2 (0.1–6.3) | 16.9 (12.4–21.4) |
| 17 | 271 | 30.4 (19.7–41.0) | 3.4 (1.1–10.2)† | 19.6 (15.5–23.7) |
| 18 | 88 | 39.8 (24.7–55.0) | 0.6 (0.1–4.0)† | 20.7 (12.1–29.4) |
| Gender | ||||
| Male | 811 | 26.8 (21.0–32.6) | 2.7 (0.8–4.6) | 17.6 (16.4–18.7) |
| Female | 1050 | 39.5 (33.7–45.3) | 1.4 (0.5–2.4) | 18.5 (12.0–24.9) |
| Area of residence | ||||
| Urban | 1361 | 33.7 (23.9–43.4) | 2.3 (0.8–3.8) | 18.3 (14.7–21.9) |
| Rural | 500 | 29.4 (20.3–38.5) | 0.9 (0.5–1.4) | 16.3 (10.8–21.9) |
| Total | 1861 | 33.0 (24.9–41.1) | 2.1 (0.7–3.5) | 18.0 (14.9–21.2) |
*Percentage (95% CI) standardised for age and grade level.
†The 95% confidence interval was calculated using binominal distribution.
The design effect was 0.6 to 9.9.
The overall rate of myopia in students 15 years of age and younger was 3.4%, tested under cycloplegia. This has been presented separately for every year of age between 7 and 15 in table 4. In the multivariate logistic regression model, age was the only variable found to be significantly correlated with the rate of myopia (OR = 1.12 per year; 95% CI, 1.01 to 1.24; p = 0.030).
The overall prevalence rate of myopia for high school students was 33.0% without cycloplegia. The univariate analysis and the multivariate regression model for gender, age and area of residence showed no statistically significant difference between groups.
The prevalence rate of hyperopia in primary and middle school students was 16.6% and showed a marked decrease from 7 to 15 years of age (p<0.001). In the multivariate logistic regression, a significant correlation was found between hyperopia and age (OR = 1.73; 95% CI, 0.83 to 0.94; p<0.001).
The rate of hyperopia in high school students, under non‐cycloplegic conditions, was 2.1%. In the multivariate logistic regression, there was a significant association between the area of residence of high school students and hyperopia (OR = 2.0; 95% CI, 1.09 to 3.65; p = 0.029).
The astigmatism rate was 18.7% among first to eighth graders, and 18.0% among high school students. The difference between students living in rural and urban areas was statistically significant (p = 0.007).
Tropia
A total of 44 participants, accounting for 0.8% (95% CI, 0.5 to 1.0), showed tropia, the type of which was esotropia in 28 students (63.6%), exotropia in 12 (27.3%), and vertical tropia in 4 (9.1%).
Anisometropia
The rate of anisometropia of 1.0 D or more was 3.6% (95% CI, 2.8 to 5.7) in primary and middle school students with cycloplegia, and 4.2% (95% CI, 2.8 to 5.7) in high school students with non‐cycloplegic refraction.
Discussion
The reported rate of refractive errors vary in different areas of the world, and studies concerning the distribution of refractive errors, especially in age, gender, and ethnic groups have been recommended.22 Several studies have been carried out according to the protocol by “Refractive Error Study in Children”2 (RESC) in countries such as China, Nepal, Chile, India, South Africa, and Malaysia.4,5,6,7,8,9,10,11 In the eastern Mediterranean area, few reports have been published in this regard.14,21 The present study on Dezful County schoolchildren was prepared based on the RESC protocol, although major differences exist. One of these differences is that the target population was the schoolchildren in Dezful County. This can greatly decrease the generalisability of the results, because it fails to cover school‐age children not attending school. Although accurate statistics are not available, it seems that the majority of Dezful primary and middle school‐age children are in school. The other difference of the present study lies in the age of the studied children, which unlike the RESC protocol, is 7 to 15 years for cycloplegic refraction, and 14 to 18 for non‐cycloplegic refraction tests. The children included in the RESC protocol were 5 to 15 years of age.
The participation in this study was a high rate of 96.8%, and a considerable percentage (95%) of first to eighth graders, aged 7 to 15 years, had their refraction tested under cycloplegia. This is one of the strong points of the study.
Overall, the visual acuity was 20/40 or worse in both eyes in 3.8% when tested without correction, in 1.7% with their presenting vision, and in only 0.3% with best correction. These figures show that the visual impairment rate in the present study (UCVA of 20/40 or worse in both eyes) is lower in comparison to results of studies in Malaysia11 (17.1%), Chile6 (15.8%), China4 (12.8%), urban areas in India8 (9.0%), and to some extent, the rural areas in India7 (5.0%). This difference can partly be attributed to the sampling methods, yet the prevalence of visual impairment in this study was higher than in studies in Nepal5 (2.9%) and South Africa9 (2.7%).
Table 6 contains the prevalence rates of refractive errors and the met need for proper correction according to eight studies based on the RESC protocol. In addition to the present study, results of studies in Oman14 and Tehran,21 previously carried out in the Middle East, are included. The data presented in this table reflects the outstanding geographical differences in the prevalence of refractive errors, and further highlights the importance of basing interventional health programs on results of local studies.
Table 6 Reported prevalence of myopia, hyperopia, astigmatism, and an unmet need for refractive error correction by several studies of children.
| Country | Sample size | Age (years) | Method | Myopia (%) | Hyperopia (%) | Astigmatism (%) | Unmet need (%) |
|---|---|---|---|---|---|---|---|
| China4 | 6134 | 5–15 | Cycloplegic refraction | 14.9 | 2.6 | 10 | 73 |
| Nepal5 | 5526 | 5–15 | Cycloplegic refraction | 0.3 | 1.1 | 3.5 | 93 |
| Chile6 | 5303 | 5–15 | Cycloplegic refraction | 5.8 | 14.5 | 27 | 76 |
| India7 (rural) | 4074 | 7–15 | Cycloplegic refraction | 4.1 | 0.8 | 9.7 | 72 |
| India8 (urban) | 6447 | 5–15 | Cycloplegic refraction | 7.4 | 7.7 | 14.6 | 92 |
| South Africa9 | 4890 | 5–15 | Cycloplegic refraction | 4.0 | 2.6 | 14.6 | 83 |
| China10 (Southern) | 4364 | 5–15 | Cycloplegic refraction | 38.1 | 4.6 | 42.7 | 45 |
| Malaysia11 | 4622 | 7–15 | Cycloplegic refraction | 20.7 | 1.6 | 21.3 | 55 |
| Iran21 (Tehran) | 1020* | 5–15 | Cycloplegic refraction | 7.2 | 6.5 | 23.9 | 37 |
| Oman14 | 6292 | 6 | Cycloplegic retinoscopy | 0.6 | Not reported | Not reported | Not reported |
| 12 | 5.2 | ||||||
| Present study | 5726 | 7–15 | Cycloplegic refraction | 3.4 | 16.6 | 18.7 | 70 |
| 14–18 | Non‐cycloplegic refraction | 33.0 | 2.1 | 18.0 |
Myopia = spherical equivalent of ⩽0.5 D; hyperopia = spherical equivalent of ⩾+2.0 D, astigmatism = cylinder refraction of ⩾0.75 D; unmet need for refractive error correction = lack of proper corrective spectacles in the presence of a visual acuity of 20/40 or worse in both eyes that can be improved to 20/40 or better with appropriate correction.
*This study concerned 4565 participants 1 year of age and over. Here, only results of the 5 to 15 year old age group are presented.
Myopia is less prevalent among 7 to 15 year olds in Dezful than countries that are experiencing a myopic epidemic. In contrast, a prevalence of 16.6% shows a higher rate for hyperopia in this very group, compared to results of all previous studies. The prevalence of astigmatism was also high and deserves attention.
We have reported the prevalence of the refractive errors based on both manifest and cycloplegic refractions. This makes the comparison of the results with other studies possible. In our study, the differences in prevalence rates between cycloplegic and manifest refraction are marked for children with the same age (tables 4 and 5). Cycloplegic refraction is important in younger age groups, as they have strong accommodative responses, which may lead to pseudomyopia. The Tehran Eye Study observed such a discrepancy in Tehran population. However, Junghans et al23 reviewed briefly the effect of cycloplegic agents on the prevalence of refractive errors and suggested that the effect is arguable. Although cycloplegia could be considered a reason, the observed discrepancies cannot be fully addressed by its effects.
The unmet need for appropriate corrective spectacles was 69.6% in this study which is comparable to results of the eight RESC studies in table 6. This is important, especially in schoolchildren, because the need can easily be met by providing proper corrective glasses. This finding also reveals that such a high rate of unmet need exists in Dezful County despite performing vision tests in the beginning of every school year. To further investigate this fact, the accuracy of the performed vision tests as well as people's access or willingness to resolve such problems must be studied.
Conclusion
The present study provides data on the prevalence rates of refractive errors in Dezful County schoolchildren. Myopia may not be very prevalent, but the high rates for hyperopia and astigmatism are worthy of consideration.
Acknowledgements
This study was a research project by the Institute of Public Health Researches of Tehran University of Medical Sciences and partially supported by Noor Vision Correction Center, Tehran.
Abbreviations
BCVA - best corrected visual acuity
RESC - Refractive Error Study in Children
UCVA - uncorrected visual acuity
Footnotes
Competing interests: none.
References
- 1.Dandona R, Dandona L. Refractive error blindness. Bull World Health Organ 200179237–243. [PMC free article] [PubMed] [Google Scholar]
- 2.Negrel A D, Maul E, Pokharel G P.et al Refractive error study in children: sampling and measurement methods for a multi‐country survey. Am J Ophthalmol 2000129421–426. [DOI] [PubMed] [Google Scholar]
- 3.Gilbert C, Foster A. Childhood blindness in the context of VISION 2020—the right to sight. Bull World Health Organ 200179227–232. [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao J, Pan X, Sui R.et al Refractive error study in children: results from Shunyi District, China. Am J Opthalmol 2000129427–435. [DOI] [PubMed] [Google Scholar]
- 5.Pokharel G P, Negrel A D, Munoz S R.et al Refractive error study in children: results from Mechi Zone, Nepal. Am J Ophthalmol 2000129436–444. [DOI] [PubMed] [Google Scholar]
- 6.Maul E, Barroso S, Munoz S R.et al Refractive error study in children: results from La Florida, Chile. Am J Ophthalmol 200029445–454. [DOI] [PubMed] [Google Scholar]
- 7.Dandona R, Dandona L, Srinivas M.et al Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci 200243615–622. [PubMed] [Google Scholar]
- 8.Murthy G V, Gupta S K, Ellwein L B.et al Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci 200243623–631. [PubMed] [Google Scholar]
- 9.Naidoo K S, Raghunandan A, Mashige K P.et al Refractive Error and Visual Impairment in African Children in South Africa. Invest Ophthalmol Vis Sci 2003443764–3770. [DOI] [PubMed] [Google Scholar]
- 10.He M, Zeng J, Liu Y, Xu J.et al Refractive error and visual impairment in urban children in southern China. Invest Ophthalmol Vis Sci 200445793–799. [DOI] [PubMed] [Google Scholar]
- 11.Goh P, Abqariyah Y, Pokharel G P.et al Refractive Error and Visual Impairment in School‐Age Children in Gombak District, Malaysia. Ophthalmology 2005112678–685. [DOI] [PubMed] [Google Scholar]
- 12.Junghans B M, Crewther S G. Prevalence of myopia among primary school children in eastern Sydney. Clin Exp Optom 200386339–345. [DOI] [PubMed] [Google Scholar]
- 13.Wedner S H, Ross D A, Todd J.et al Myopia in secondary school students in Mwanza City, Tanzania: the need for a national screening programme. Br J Ophthalmol 2002861200–1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lithander J. Prevalence of myopia in school children in the Sultanate of Oman: a nation‐wide study of 6292 randomly selected children. Acta Ophthalmol Scand 199977306–309. [DOI] [PubMed] [Google Scholar]
- 15.Khandekar R B, Abdu‐Helmi S. Magnitude and determinants of refractive error in Omani school children. Saudi Med J 2004251388–1393. [PubMed] [Google Scholar]
- 16.Lin L L K, Shih Y F, Hsiao C K.et al Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singapore 20043327–33. [PubMed] [Google Scholar]
- 17.Villarreal M G, Ohlsson J, Abrahamsson M.et al Myopisation: the refractive tendency in teenagers. Prevalence of myopia among young teenagers in Sweden. Acta Ophthalmol Scand 200078177–181. [DOI] [PubMed] [Google Scholar]
- 18.Mavracanas T A, Mandalos A, Peios D.et al Prevalence of myopia in a sample of Greek students. Acta Ophthalmol Scand 200078656–659. [DOI] [PubMed] [Google Scholar]
- 19.Robaei D, Rose K, Ojaimi E.et al Visual acuity and the causes of visual loss in a population‐based sample of 6‐year‐old Australian children. Ophthalmology 20051121275–1282. [DOI] [PubMed] [Google Scholar]
- 20.Hashemi H, Fotouhi A, Mohammad K. Tehran Eye Study: research design and eye examination protocol. BMC Ophthalmology 200338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hashemi H, Fotouhi A, Mohammad K. The age and gender specific prevalences of refractive errors in Tehran: the Tehran Eye Study. Ophthalmic Epidemiology 200411213–225. [DOI] [PubMed] [Google Scholar]
- 22.Negrel A, Ellwein L B. More research needed to assess the magnitude of refractive errors world‐wide. Community Eye Health 20001311–12. [PMC free article] [PubMed] [Google Scholar]
- 23.Junghans B M, Crewther S G. Little evidence for an epidemic of myopia in Australian primary school children over the last 30 years. BMC Ophthalmology 200551. [DOI] [PMC free article] [PubMed] [Google Scholar]