Of Britain's recent wars, the Falklands campaign of 1982 was anomalous in many respects, fought to defend a colony with a small but a loyal population, 8000 miles away, but it was also relatively straightforward. It involved high-level diplomacy and consultations at the United Nations, but it was decided on the battlefield in a series of short, but intense engagements conducted by elite units, starting at sea, with civilians at risk only towards the end. The politics were uncomplicated: the British territory had been taken in a clear act of aggression by an unsavoury military junta. The British forces were sent into action on a patriotic mission without having to worry about allies. Domestic public opinion was largely in favour of a robust response, and gave enthusiastic backing to the forces, while international opinion was also generally supportive, although anxious, when the response looked over robust.
As it is well known, the campaign was a military success. Furthermore, in the aftermath of the war, there was little debate or controversy concerning any long-term impact on health. Only the possible impact of the conflict on the mental health of service personnel became a cause of concern, and this did not surface for some years. The initial impression was of only a very few acute psychiatric casualties, which was not surprising, since the cause was clear-cut, morale was high, engagements were few, civilian massacres were absent, and the campaign was successful. It was also thought that the long sea voyages to and from the conflict made adjusting both to the prospects of combat and then its aftermath easier. It took time before concerns developed about the appearance of post-traumatic stress disorder (PTSD) in veterans of the campaign, as more began to report symptoms blamed on the conflict. Claims were made about the distressed state of many veterans' lives, not just PTSD, but also alcoholism and crime. By 2000, allegations were being made that increasing numbers of veterans were committing suicide, although the absence of any systematic monitoring made it impossible to determine the true rate of PTSD and/or suicide. In 2002, a group action with which some 2000 veterans were associated, including a number of veterans from the Falklands (notably Welsh Guardsmen who had been aboard Sir Galahad), reached the High Court. The claimants argued that the Ministry of Defence had not given them adequate support to cope with PTSD; the Ministry insisted that treatment was ‘in line with contemporary best practice’ and the Judge ruled that there had not been any systematic negligence (Freedman 2005).
Less than a decade later, the British forces were in action again, but in the Persian Gulf. This time the cause was less national, but domestic support was strong and international support was far less tentative. Iraq had committed clear aggression against Kuwait and had been given every diplomatic opportunity to avoid war by backing down. Prior to the war, there had been considerable apprehension about its likely course and costs. This was going to be the Americans' first major action since Vietnam, and there were grim warnings of the preparation of Iraqi killing fields in which coalition troops were bound to get caught (Freedman & Karsh 1993). In the event, the fighting itself was even more one sided. The British casualties were far fewer than in the Falklands: indeed, after the initial Royal Air Force bombing missions against Iraqi airfields, actual engagements were few and far between with the enemy. So successful were the military operations that there was talk of a revolution in military affairs, suggesting that by combining the new information technologies with precision guidance, firepower could become far more efficiently deployed and the numbers of casualties on all sides much reduced.
Yet not longer after the end of hostilities, and in marked contrast to the experiences after the Falklands campaign, this optimistic assessment began to be questioned as reports started to emerge from the United States of unusual clusters of illness in Gulf War veterans. These were either hard to pin down, or, where specific claims were made, as for example of an increase in particular birth defects, were not confirmed (see Doyle et al. 2006). But by 1993, the concerns were growing, and the word ‘Gulf War Syndrome’ was starting to be heard, first in the United States, then in Canada and in the United Kingdom and finally in Australia.
1. Getting our terminologies right
As both Gray & Kang (2006) and Ismail & Lewis (2006) show, the term ‘Gulf War Syndrome’ is a misnomer, since no new illness or symptom cluster unique to Gulf War veterans has been identified. Instead, it is more accurate to talk about ‘Gulf War illness’, or ‘Gulf War illnesses’, or even the ‘Gulf War health effect’. Having said that, it is likely that it is ‘Gulf War Syndrome’ which will continue to be the label used to describe the medical legacy of the war, a fait accompli belatedly accepted by the UK Ministry of Defence in a recent War Pension Tribunal ruling. And it is a definite and by no means minor legacy. 21% of the US Gulf veterans now receive some form of disability support from the Veterans' Administration. In 1998, 17% of the British Gulf veterans believed they were suffering from ‘Gulf War Syndrome’ (Chalder et al. 2001). At the time of writing, 10% of the British Gulf War veterans are in receipt of either war pensions or gratuities.
Putting aside arguments about terminology, syndrome or no syndrome, it is incontrovertible that rates of ill health are greater in Gulf War veterans than in members of the Armed Forces who did not serve in the Gulf. This applies to the United States, Canada, the United Kingdom and Australia, but not, as far as we can gather, Saudi Arabia (Gackstetter et al. 2005).
Note that we are careful to use the term ‘ill health’. So far, there has been no evidence of an increase in mortality in Gulf veterans neither from the United States or the United Kingdom, with the exception of deaths from injuries (Gray & Kang 2006). Nor has convincing evidence been presented for an increase in any well-defined medical condition. The United States Gulf War veterans are more likely to be admitted to hospital than appropriately chosen controls, but the increased risk is for mental health diagnoses, multi-symptom conditions and musculoskeletal disorders. The only disease-based outcome which has been reported to be elevated in Gulf War veterans is motor neuron disease (MND), and this is neither definitive, nor able to explain ill health in anything other than a fraction of sick Gulf veterans (see below).
If we follow the helpful approach suggested by Arthur Kleinman (1988) and others of making a distinction between disease—in which there is pathological evidence of dysfunction—and illness, in which a person reports symptomatic distress and suffering, but no pathological condition can be found to explain this as yet—then at the moment Gulf veterans are suffering from illness, but not disease. Note once again the need to be careful with terminology—this time the phrase ‘as yet’. The history of medicine gives many examples of illnesses that are subsequently associated with distinct pathologies that are then recognized as diseases, and so it may prove with Gulf War illness. But, it is not all unidirectional—the history of medicine also gives examples of illnesses that are never found to have a basis in pathological changes, and gradually fade away. Now, few talk about Soldier's Heart or Effort Syndrome, but these were the Gulf War Syndromes of their day (see Jones 2006). We cannot predict the direction that Gulf War illness will take.
2. Causes—plenty of villains, but no convictions
War is always a risky business, and there was no shortage of possible hazards to health that accompanied the Gulf War. It was not just the usual dangers—the risk to life and limb from the various munitions and explosives that are part and parcel of modern war, to which we must also add the dangers to the psyche as well. Other unexpected, but not novel hazards included the smoke from the oil fires deliberately started by the Iraqis as they retreated from Kuwait.
But there were also other hazards that were more recent additions to the ways in which mankind has harnessed technology to deadly ends. Back in 1991, as opposed to 2003, Saddam Hussein possessed large stocks of chemical and biological weapons (CBW), and had used the former both in the Iran–Iraq war and against the Kurds. To counter this threat, it was necessary to provide at least some measure of protection, which ranged from giving vaccinations against biological agents such as plague and anthrax, or taking pyridostigmine bromide tables to protect against exposure to organophosphate (OP) nerve agents. No intervention, even a preventive one, is risk-free, and all of these must have had some side effects.
So, when we start looking for culprits to explain the increased reporting of ill health that is observed in Gulf veterans, it makes sense to start with these well-defined potential hazards.
3. Toxicological explanations for Gulf War illness
There was no shortage of exposures to potentially harmful substances during the course of the war. For example, Doyle et al. (2006) cite the report by the US General Accounting Office in 1994 that identified 21 potential reproductive toxicants and teratogens that were present during the 1990/91 Gulf War (US GAO 1994). These included arsenic, benzene, benzopyrene, cadmium, lead, mercury, nickel, toluene, xylene, di-n-butyl phthalate, hexachlorobenzene, hexachloroethane, pentachlorophenol, hexachlorocyclopentadiene pesticides (carbaryl, diazinon, dichlorvos, ethanol, lindane, warfarin), and decontaminating agents (ethylene glycol, monomethyl ether), and that is just dealing with potential teratogens. To this list numerous other potential hazards must be added. Attention, however, has tended to focus on a smaller range—chief among which are exposure to depleted uranium (DU) munitions, OP chemicals, and the side effects of what are known as ‘medical counter measures’ (MCMs), which covers the vaccinations and drugs given to protect personnel against the threat from CBWs.
All of the above are potential hazards to health. The question is not whether compound A is toxic to health—the answer is that it depends on when, where, how and in what quantity the person has been exposed to that chemical. Thus, OP pesticides can cause severe neurological damage and death—OP pesticide ingestion is a common method for suicide in many countries. The question is whether sufficient Gulf personnel were exposed to such compounds to account for the epidemiology of Gulf ill health, and if so, was it at a dose likely to cause long-term health effects?
Turning to those interventions that were deliberately used to provide protection against other dangers, the MCMs, here we know that a sufficient number of personnel were exposed to the putative risk factor to account for most, but not all, of the observed health effects (the experience of some Canadian and Danish forces who did not receive such prophylaxis yet still developed symptoms being exceptions). The question then is not whether considerable numbers of personnel had such exposures—they did—but whether or not they were indeed associated with long-term health effects. That some will have experienced short-term side effects is a given—the intervention that provides only benefits, and no risks, has yet to be discovered. Instead, we need to ask whether such side effects persisted, or did new adverse effects develop over time, and what was the overall balance between risk and benefit?
So, there is no doubt that most of the agents that have been listed as causes of Gulf War ill health can be toxic or cause side effects. They are all plausible culprits, but did exposure actually occur in sufficient quantities and at sufficient dosage to account for a substantial proportion of the changes in ill health that have been documented? These are the questions that take up the third section of this issue. And the answers seem to be generally in the negative.
For example, DU munitions were used in the Gulf War, but are a most unlikely cause of the Gulf War health effect. Squibb & McDiarmid (2006) discuss the toxic effects of DU in detail, drawing heavily on the close monitoring that they have carried out of Gulf War veterans with indisputable exposure to DU, namely those who were victims of so called ‘friendly fire’ incidents. These individuals are excreting uranium, confirming their exposure, and are, therefore, at risk from the known toxic effects of DU, which relate to its heavy metal properties (and not its radiological hazard, as is often stated in the media). Intense surveillance of these individuals has failed to find an evidence of renal impairment, the most likely consequence of significant DU exposure. Overall, the reported health changes have been subtle, and not as yet associated with any particular disease outcome. Given that this group is indisputably with the highest exposure, it is implausible that substantial or indeed any health effects will be seen in those with much less chance of exposure and at much lower doses. The epidemiology of DU exposure is also not the epidemiology of the Gulf health effect (see Ismail & Lewis 2006). DU is overall not a likely candidate to explain any of the observed health changes.
Looking at the role of MCMs, Peakman et al. (2006) have focussed on possible side effects of the vaccinations given to protect personnel against biological weapons. Here, the epidemiology is more persuasive, since large number of the Coalition forces were definitely exposed to these measures, unlike the case for DU. Using the King's military cohort, they reported an association between receipt of multiple vaccinations and ill health (Hotopf et al. 2000), although this was not accepted by all. The authors themselves were careful not to ascribe direct causality to this relationship, since the possibility of hidden bias remains present, echoing the views of the Institute of Medicine as well as subsequent correspondence in the journals.
It is also true that there is no particular accepted mechanism which might explain such a link—Peakman et al. 2006 also present some new evidence that has failed to confirm the theoretical case made by Rook & Zumla (1997) in the Lancet that Gulf War illness might be the result of a Th2 cytokine shift induced by the combination of multiple vaccination, stress and the use of the pertussis vaccine as adjuvant. Such a model also suffers from the fact that it relates only to the vaccination policy used by the British Armed Forces; it cannot explain the ill health experienced by other forces, who did not use the same regime. Nor can it explain the ill health experienced by Danish Gulf veterans, who only entered the theatre after the end of hostilities, and used no medical interventions to protect against chemical or biological agents (Ishoy et al. 1999; Bregenhol et al. 2001).
As with other putative risk factors for Gulf War ill health, it is difficult now to see how further research on Gulf Veterans will provide much more in the way of relevant information concerning aetiology, as opposed to treatment and prognosis. However, researching other populations may still shed some light. For example, the multiple vaccination hypothesis is currently being tested in a randomized controlled trial of different vaccine regimes being pursued by the US Navy at the time of writing.
Another much debated question is whether or not Gulf War illness can be attributed to the exposure to OP agents, if used as pesticides or in the form of nerve agents such as sarin and cyclosarin. But here we face even more difficulties. When considering the possible involvement of vaccinations, Hotopf et al. (2000) used exposure data as the starting point of looking for a relationship with later ill health. However, because no nation had accurate electronic data based on exactly who received what vaccines and when, this was a less than perfect undertaking, but better than nothing.
Unfortunately, when it comes to exposures to other potentially toxic agents, nothing is what we have. Glass & Sim (2006) explore the problems in greater depth, but it is reasonable to say that we lack virtually any credible exposure data on e.g. OP agents, just as we lack credible exposure data on the use of pyridostigmine bromide. Self report made by service personnel many years after the conflict is unreliable for many reasons, and particularly is likely to lead to false estimations of association because of insuperable issues around recall bias (Spencer et al. 2001; Wessely et al. 2003).
Instead, it is more profitable and less prone to error to look at the occurrence of disorders that might be related to exposure—in other words to concentrate on the outcome, not on the exposure. For the OP agents this translated into studies of neurological and neuropsychological dysfunction, since these agents are par excellence neurotoxic in nature.
Two contributions in particular address this issue. Rose & Brix (2006) review the prevalence of neurological disorders in Gulf veterans. Despite the early reports of damage to the peripheral nervous system, later large controlled studies have failed to replicate these (Amato et al. 1997; Sharief et al. 2002; Davis et al. 2004), with the large epidemiologically based controlled study undertaken by the Department of Veterans' Affairs coming as close as possible to providing definitive negative data (Davis et al. 2004).
However, this does not totally close the door on any link between Gulf War service and neurological outcomes. Two possibilities still remain. The first is that, although there now seems little doubt that neurological disorders cannot explain the vast majority of Gulf-related ill health, small occupational groups might still be found with increased risks of disease. For example, there are anecdotal reports that environmental health technicians charged with spraying pesticides to remove the threat from insect-borne disease might have had local high-level exposure, especially if safety procedures were lax.
The second issue is that of MND, also known as amyotrophic lateral sclerosis (ALS). After much advanced publicity, an epidemiological study was published reporting an increase in MND in US Gulf Veterans (Horner et al. 2003). Prior to publication, the Veterans' Administration had already made the decision to accept MND as ‘service related’ for the purposes of compensation. The issue is not however resolved, and as both Gray & Kang (2006) and Rose & Brix (2006) suggest, it would be premature to conclude that MND is caused by Gulf War service, not least because of the absence of evidence from mortality studies of any increase in MND, relevant since regrettably it is a progressive neurological disorder that is usually and fairly rapidly fatal. MND is, however, rare and even if the VA study is correct, such an increase in risk could never account for anything more than a tiny fraction of the burden of ill health in Gulf veterans, most of whom do not have evidence of any peripheral nervous dysfunction, let alone MND.
Looking for evidence of damage to the peripheral nervous system as a way of inferring exposure to possible neurotoxic agents has produced data more reassuring than alarming. But what about damage to the central nervous system (CNS)? Vasterling & Bremner (2006) address this in their contribution. They conclude that although many Gulf veterans do complain of cognitive problems, tests of neuropsychological function have not revealed consistent findings, and have not provided convincing evidence of what journalists might label ‘brain damage’. The situation is analogous to the findings in the civilian literature surrounding chronic fatigue syndrome, in which there is a lack of synergy between subjective symptoms of not only cognitive function but also neuromuscular function, and objective evidence of deficits from formal neuropsychological or neurological testing (Lawrie et al. 1997).
There is another strand to the narratives around exposure to nerve agents as a possible cause of Gulf War illness. Most attention has been given to the possibility that the accidental discharge of sarin nerve agents that followed the destruction of the Khamisayah arms dump is a cause of ill health, although the evidence for this continues to be unconvincing (Gray et al. 1999; McCauley et al. 2002), not least because of the absence of any contemporary evidence of adverse effects of exposure (Committee on Gulf War & Health 2004; www.mod.uk/issues/gulfwar/info/Khamisayah2005/summary.htm).
How else could that exposure have occurred? Some say that the Iraqi forces did use sarin in the theatre of war, and have been more specific, claiming that the results of studies suggest that this happened on day four of the ground war (see http://www.gulflink.org/stories/disasternews/studies.htm). At a Federal Investigator's meeting in December 2001, one prominent advocate of this theory suggested that the Khamisayah episode was a CIA smokescreen to cover up the real facts about deliberate use of sarin by the Iraqis. Overall, the claims that there was deliberate, but undetected, use of chemical agents by the Iraqis lacks any military or intelligence credibility. We should remember that not only were considerable resources devoted to detection, military health care personnel were on alert for chemical casualties during the war, and were particularly attentive to this threat because exposure of health personnel while caring for contaminated patients could cause illness and death.
4. Psychiatric explanations for gulf war illness
No compelling evidence has been provided to support straightforward toxicological explanations for Gulf War illness, and for many reasons it seems unlikely that this situation will change. So are psychiatric explanations any more successful?
Only a few would deny that war can be a stressful business, and Gifford et al. (2006) have provided an excellent narrative account of what some of those stressors were. Once the war was successfully concluded, there were no shortage of commentators telling us how it was inevitable that the Iraqi forces would crumble under the assault of the Coalition forces, and that there was never a realistic chance that Saddam Hussein would authorize the use of chemical or biological agents. But, that was not how it seemed to those personnel preparing in the desert during the weeks and months before the ground war was launched, or to the military planners themselves.
Some of those stressors have taken their toll—a series of studies have shown beyond doubt that rates of formal psychiatric disorder have increased about twofold in Gulf veterans (Stimpson et al. 2003). Future historians may be perplexed by the vociferous attempts of some of those involved in the Gulf War illness saga to deny this, including one or two politicians and lobbyists whose knowledge of the history of war and psychiatry seems to have stopped in 1914. However, while denying that war can cause psychiatric injury which can present with physical symptoms is unsustainable, a more nuanced and relevant observation is that the same studies which confirm an increase in formal psychiatric disorders, such as PTSD or depression, also show that this increase is not per se sufficient to explain the entirety of the Gulf health effect.
But formal psychiatric disorders such as depression or PTSD are not the only outcome of prolonged stress or fear. There is a firm consensus that physical symptomatology is related to stressful exposures in all sorts of circumstances, and going to war is no exception (Storzbach et al. 2000; Ford et al. 2001). In particular, many commentators are right to draw attention to the real threat posed by CBWs and its psychological consequences (Stokes & Banderet 1997; Betts 1998). Such weapons ‘engender fear out of all proportion to their threat’ (O' Brien & Payne 1993)—they are as much, if not more, weapons of psychological as physical warfare (Holloway et al. 1997). Even in training up to 20% of those who took part in exercises using simulated exposure to irritant gases showed moderate to severe psychological anxiety (Fullerton & Ursano 1990).
During the Desert Storm, there were several thousand documented chemical alarm alerts. Subsequently, the consensus of opinion is that none was a true positive, and that Iraq did not use its CBW arsenal. But at the time each alert had to be assumed to be genuine. Thus, even if traditional military stressors were not a prominent feature of the active campaign, a well-found and realistic anxiety about the threat of dread weapons could still be important. It does not take much imagination to accept the potent psychological effects of operating in an environment where one could be subject to chemical attack, or the damaging effects of believing, even erroneously, that one has been the victim of such an attack (Fullerton & Ursano 1990; Riddle et al. 2003). Believing oneself to be exposed to such weapons has been found frequently to be associated with the development of symptoms (Unwin et al. 1999; Nisenbaum et al. 2000), sometimes very strongly (Haley et al. 1997; Proctor et al. 1998; Stuart et al. 2003).
Finally, we also draw attention to the literature that suggests that media reporting of health hazards is not without consequences itself. The greater the degree of concerns around environmental hazards and other ‘modern’ health concerns, the greater the symptomatic response when people are exposed to pesticides and/or other chemicals (Winters et al. 2003; Petrie et al. 2005).
5. Illness and culture
In the third section of this issue, it is concluded that the evidence to support exposure to agents such as DU or sarin nerve agent as the cause of Gulf War illness is uncompelling, nor has any convincing data been presented to implicate MCMs. Why then did the issue become such a cause celèbre, and why, despite the authoritative reviews coming from the Institute of Medicine and other august bodies, are so many people apparently convinced that this is not so?
There are many reasons. As we have said repeatedly, these agents do damage in the wrong doses and in the wrong place. Thus, it is only prudent for people to ask whether or not such agents are the cause of ill health. However, one also needs to ask why many people show an apparent unwillingness to accept answers when they do not accord with their own convictions.
The DU controversy offers some insights into these processes. The main toxic hazard from DU is chemical, not radiological (see Squibb & McDiarmid 2006). It is now well-established that popular perceptions of risks from environmental hazards are very different from scientific calculations of the same risks (Slovic et al. 1995). Study after study confirms that radioactive hazards are associated with particular fear and dread. It is likely that the high public and media attention given to DU may not come from its properties as a heavy metal, but its lexical links to radiation, conjuring up images of Hiroshima and Chernobyl, and thus scoring as high as one can get on measures of risk perception.
There is also a political dimension. The only two countries that use DU munitions are the United States and the UK. Some of those who campaign against US or UK policy in e.g. the Balkans or Iraq use alleged health effects of DU as part of their arguments. In 2000, the European media was full of reports of an epidemic of cancer among the Italian military personnel involved in peacekeeping duties in the Former Yugoslavia, blamed on exposure to DU munitions used by the US Forces. DU would not have been a likely cause for such a cluster, which has never been confirmed. Subsequent media reports suggested that this was a story that had originated from the Italian pressure groups opposed to their nation's involvement in Balkans peacekeeping.
Both Kilshaw (2006) and Durodié (2006) extend these arguments further. They see links between well-voiced health concerns from the civilian sector and those that surfaced in the aftermath of the Gulf War. Kilshaw uses her experience of fieldwork with Gulf veteran groups in the UK to conclude that ‘there were other things happening in the lives of these men and women other than the war that they are trying to explain’. She is suggesting that we should look beyond the events of the 1991 war to the wider social and cultural context from which these explanations emerged. She quotes philosopher Ian Hacking to the effect that an illness movement will gain attention and hence legitimacy ‘only if there is a larger social setting that will receive it’.
Thus, it is important, as Durodié notes, that we view the Gulf War illness debate in that wider context. Both authors draw attention to the increased anxieties that surround health and the environment over the last decades, and it is difficult to conclude there are no links between e.g. the ecology movement that began with Rachel Carson's indictment of the environmental consequences of pesticide exposure and the similar anxieties expressed over pesticide use in the Gulf War, even if it is unlikely that these have caused long-term ill health in anything other than a tiny minority (see Brown 2006; Rose & Brix 2006). Likewise, fears about long-term adverse effects of vaccination have been expressed with increasing regularity and vehemence, culminating in the MMR crisis in the United Kingdom. There is no reason to believe that service personnel are immune to the same concerns as have surfaced in civilian life. When links can be made between concerns that surface in a military context and wider issues of public debate, media coverage is also far more likely.
This is not the first time that veterans of a foreign war have voiced health concerns. Back in 1945 Australian veterans of the campaign against the Japanese in Papua New Guinea believed that malarial prophylaxis had caused both problems with infertility and an increased rate of congenital handicap in their offspring. However, it was the Vietnam War, and more specifically the legacy of Agent Orange, that triggered a major political crisis on a scale that equalled or even surpassed that associated with Gulf War illness.
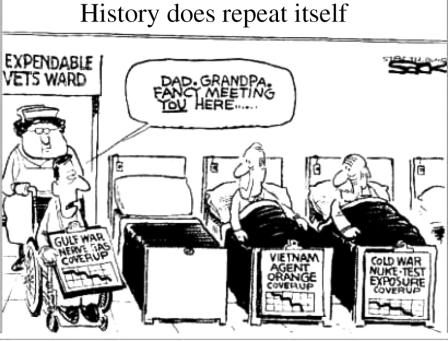
Zavestoski et al. (2002, 2004) has shown how some of the Gulf War veterans made direct parallels between their experiences and those of Vietnam veterans, and drew on the Agent Orange protest movement as a basis for their own efforts. The perceived legacy of government misinformation or even betrayal around Agent Orange was used to claim similar cover-ups and conspiracies, as was the Cold War legacy of experiments carried out on service personnel, often without consent (figure 1). The governments on either side of the Atlantic have made misinformed statements on the Gulf issues—the US government misjudged the Khamisayah incident, while the UK government made an inaccurate statement to the Parliament about the use of OP pesticides. For many, these seemed most likely to represent bureaucratic failures in understanding the scientific information, but the benefit of doubt was not given to the authorities. Instead, both the episodes fuelled further suspicion and an occasional paranoia. Given that the risk communication and management is critically dependent upon a trust between the community that feels exposed and those responsible for managing that risk (Slovic 1999), these misjudgements may have been integral to the further development and shaping of ‘Gulf War Syndrome’ after the conflict (Engel et al. 2002).
Figure 1.
Cartoon from “History Does repeat Itself” by Steve Sack. Copyright (©) 2006 Tribune Media Services. Reprinted with permission.
6. ‘Friendly fire’
Most members of the professional, volunteer Armed Forces accept that the job entails a certain exposure to physical danger. This is the nature of the ‘military contract’ (Dandeker 2001). It is fortunate that in most conflicts launched by small, modern militaries such as the British the statistical chances of this happening are relatively small, at least in comparison to the casualty lists of the World Wars. If, however, a serviceman is wounded, we have already alluded to the powerful evidence that in addition to their physical injuries, they are also at increased risk of psychological injury. This risk is, however, reduced by various factors. These include morale, leadership and, most of all, training. The professionalism of the modern soldier is one defence against the high levels of psychiatric injury sustained by conscript armies during the First and Second World Wars.
But, the risk of developing psychiatric disorder after physical injury can also be increased as well as decreased. The psychological consequences of being wounded by your own side are far greater than when it occurs as a result of enemy action. The latter is part of the military contract—the former is not. This is the problem of ‘friendly fire’.
Why is this relevant to the question of Gulf War illness? There were indeed isolated cases of both the British and the American personnel being wounded by the Coalition forces, and anecdotal evidence suggests that these personnel have indeed experienced greater psychological problems than others. But, while disturbing, the numbers are very small, and certainly do not contribute to the burden of ill health of Gulf veterans.
‘Friendly fire’ traditionally refers to those injured by inadvertently targeted munitions from their own side. But the Gulf conflict, or more accurately its aftermath, has extended this further. Some of the alleged ‘toxic’ hazards that have been blamed for ill health are extensions of the ‘friendly fire’ concept, since they also originated from ‘our side’ (Kilshaw 2004). Among the key exposures most frequently implicated in theories of ‘Gulf War Syndrome’, only one, smoke from the burning oil wells, was explicitly the result of enemy action, and it is interesting to note that this is the exposure that has attracted the least coverage and controversy. Perhaps it is because even while the fires were burning, numerous environmental measurements were taken, and those generally reassuring results were soon disseminated. Or perhaps it was because the pollution from the oil fires was clearly the result of Iraqi hostile action, and not a sin of commission or omission by our own side.
In contrast, any health risks to the Coalition forces from DU munitions, for example, can only come from either the British or the US Armed Forces, since these are the only militaries that use DU. Vaccinations to protect against biological weapons are given by one's own side, and thus, any side effects are self inflicted, even if for a ‘good cause’. Anti-cholinesterase tablets to protect against the permanent and fatal blockade of acetyl cholinesterase, the result of exposure to nerve agents such as sarin and cyclosarin, come into the same category, as do the pesticides used to protect against the threat of insect borne disease. Sarin nerve agent was possessed by the Iraqis, not the Coalition forces, and the continuing controversy over its role in Gulf ill health seems to be an exception, unless one considers that the cause of exposure, albeit in amounts unlikely to pose any threat to human health, came from the destruction of sarin-containing munitions at the Khamisayah site by the US forces after the end of hostilities. Similarly, we draw attention to the attempts to sue US contractors who are alleged to have supplied the Iraqi regime with the precursors needed to create sarin and cyclosarin, on which basis they are held to be responsible for ill health in US veterans.
7. The future
When a future Official Historian addresses the 1991 Gulf War, he or she will most likely have to record confusion and uncertainty in summing up its medical legacy.
It is also likely that it is a subject which will not enhance many collective reputations. At the launch of the official history of the Falklands War written by one of the current authors (L. Freedman), it was amusing for the other author (S. Wessely) to observe the number of the good and the great who moved purposefully towards the pile of copies, and then immediately consulted the index to see how they had been treated. Most seemed not displeased with the result. We doubt that there will be a similar rush from those involved in the Gulf War Syndrome saga to discover the historian's verdict.
However, not all consequences have been adverse. As the contribution from Engel et al. (2006) demonstrates, numerous lessons have been learnt about post-deployment health issues. Not least has come a commitment to improved health surveillance to give early warning of any future health crises. Other much needed and welcome changes have been a recognition of the importance of health complaints and symptomatic distress, even in the absence of formal physical or psychological disorders, the importance of primary care and a true population-based approach to health care, and perhaps most of all, the need for better communication around risk.
8. From the Gulf to Iraq
This issue is concerned with the health problems experienced by the Gulf War veterans. But this has not been a unique experience. In the decade after the 1991 Gulf War, newspaper reports have appeared concerning e.g. the ‘horrendous range of symptoms’ experienced by the Canadian UN peacekeepers in Croatia (Gilmour 1999) and Dutch peacekeepers in Cambodia (Soetekouw et al. 1999; De Vries et al. 2000). Similar reports have emerged in the German and Belgian press concerning their soldiers in Kosovo. Concerns include exposure to DU munitions, contaminated sandbags (Kondro 1999) or pollutants released from the destruction of factories during the NATO bombing campaign against Serbia. The outcome of the 1992 El Al crash in Amsterdam reproduced many of the features of Gulf War Syndrome (Yzermans & Gersons 2002), including the same rise in symptoms, concerns about exposures to DU and chemical weapons, allegations of conspiracies and cover up, but an absence of evidence of a change in objective outcome measures (Slottje et al. 2005).
There are many reasons to think that this situation will not change for the better. The current uncertainty over the chronic health effects of low-level exposure to chemical and nuclear materials that so dominated the discourse around Gulf War illness will no doubt continue. Since health officials cannot provide blanket assurances that harm will not result from acute, non-symptom producing exposure, distrust of medical experts and government officials is likely to continue. The potential effects of low-level chemical and radiation exposure is a longstanding controversy (Birchard 1999). A recent United Kingdom Royal Commission report on pesticide exposure is unlikely to resolve concerns over their use—indeed some believe that it will only serve to increase anxiety.
The perceived health risks of modern wars cannot also be divorced from their political context. For the two decades after the Falklands War, there was a growing tolerance of the use of force by the western countries. The purposes for which force had been used seemed appropriate—in addition to the reversing acts of crude aggression, there were also operations designed to address developing humanitarian catastrophes (Sierra Leone, Kosovo) as well as to deny terrorists sanctuary (Afghanistan). Yet, there was also a sense that these operations had a discretionary aspect, as so-called ‘wars of choice’, so that if the rationale became unclear or the costs too high, then public support might evaporate and the position of the service men and women taking part be subject to more questioning. To some extent, this has begun to happen with Iraq and there have been suggestions that any association with war crimes, or the risk of being accused of such crimes, could put stress on troops operating in difficult conditions where insurgents mingle with the local population. So in addition to the changing social attitudes to risk and illness, there may also be changing attitudes to the military profession, from a population which will generally have little experience or understanding of how the armed forces go about their business.
We do not anticipate that many of these complex scientific and political issues will be resolved in the near future. Improved research capability and a more rapid response to health concerns will assist, but the difficulties in conducting research in the military context in general, and the emotionally charged atmosphere that continues to exist around unexplained illnesses in particular, will remain (Neutra 1985; Roht et al. 1985; David & Wessely 1995; Hotopf & Wessely 2005). As a result, numerous unconfirmed and controversial hypotheses about the effects of low-level exposures will flourish, just as they did after the Gulf campaign. The ‘Gulf War Syndrome’ was but one of many ‘contested diagnoses’—it is unlikely to be the last (Shriver et al. 2002; Engel 2004; Aceves-Avila et al. 2004).
Finally, as we write, the American and the UK forces remain engaged in Iraq. There have been a handful of reports starting to emerge that describe many of the same concerns that began to appear soon after the end of the 1991 Gulf War. So far, however, we have not seen anything emerging on the scale of the problems witnessed in the aftermath of the 1991 conflict. One of the lessons that was definitely learnt after the Gulf War was the need to have large-scale systematic health surveillance and research in place at the earliest opportunity, and this has indeed taken place, either via the US Millennium Cohort (Gray et al. 2002; www.millenniumcohort.org) or the King's Military Health cohort (www.kcl.ac.uk/kcmhr). Preliminary analysis of the data from the UK study designed to specifically monitor rates of multi-symptom ill health has not so far given a cause for concern. Instead, most of the focus has been on more classic and formal psychiatric injuries, suggesting that the health effects of the Iraq War come more to resemble those observed after Vietnam rather than those observed after the Gulf War (Hoge et al. 2004). If this picture persists, and no multi-symptom illness emerges, then we may have to reconsider at least some of the assumptions that have been made on the nature of Gulf War illness.
9. Last word
Despite the best endeavours of the contributors to this issue, the reader who has persevered to the end of this final chapter will still not be in possession of a simple answer to the question—‘what was the medical legacy of the 1991 Gulf War?’, or even simply ‘what is the cause of Gulf War Syndrome?’ We hope the reader is now reassured that, albeit belatedly, serious efforts have been made in many of the countries that took part in the campaign to try and unravel the problem and address the concerns of veterans. Even if we clearly do not have answers to all the questions, at least some of the possible causes for long-term ill health have been investigated, and found not to account for anything more than a small proportion of observed ill health. The reader may, however, be more reassured that many lessons have been learnt.
This issue began with a historical contribution to understanding post-conflict ill health, and it is fitting that we end with a similar observation. In the aftermath of the First World War, doctors were confronted with a large number of ex-service personnel who reported strange physical symptoms, chief among them being easy physical and mental fatigue and fatigability, and widespread body pains. For them, everything had become an effort, and sleep was both non-refreshing and frequently interrupted by nightmares (Wheelwright 2001). There were no shortage of theories concerning what might be the cause of their problems, but no single viewpoint ever proved conclusive. Among the many physicians who gave their services to the cause of veterans' health was Sir Thomas Lewis (see Jones 2006). His inquiries concerning what he described as the ‘effort syndrome’, previously known as the Soldier's Heart, spanned two decades (Lewis 1940) and demonstrated not only his scholarship, but also his willingness to embrace new concepts and ideas.
Said Lewis (1940), ‘It is the apparent diversity of cause which makes the syndrome so extraordinarily difficult to investigate’, sentiments with which we can only agree. Armed with the tools of modern medicine we can perhaps congratulate ourselves that we have been able to address some issues with a little more rigour that was possible for Lewis and his contemporaries, but humility remains the order of the day, since we have not solved the problem either.
Footnotes
One contribution of 17 to a Theme Issue ‘The health of Gulf War veterans’.
References
- Aceves-Avila F, Ferrari R, Ramos-Remus C. New insights into culture driven disorders. Best Pract. Res. Clin. Rheumatol. 2004;18:155–171. doi: 10.1016/j.berh.2004.02.004. doi:10.1016/j.berh.2004.02.004 [DOI] [PubMed] [Google Scholar]
- Amato A, McVey A, Cha C, Matthews M.D, Jackson C.E, Kleingunther R, Worley L, Cornman E, Kagan-Hallet K. Evaluation of neuromuscular symptoms in veterans of the Persian Gulf War. Neurology. 1997;48:4–12. doi: 10.1212/wnl.48.1.4. [DOI] [PubMed] [Google Scholar]
- Betts R. The new threat of mass destruction. Foreign Aff. 1998;77:26–41. [Google Scholar]
- Birchard K. Experts still arguing over radiation doses. Lancet. 1999;354:400. doi:10.1016/S0140-6736(05)75821-9 [Google Scholar]
- Bregenhol S, Ishoy T, Skovgaard L.T, Suadicani P, Appleyard M, Guldager B, Malte L, Gyntelberg F, Claesson M.H. No evidence for altered cellular immune functions in personnel deployed in the Persian Gulf during and after the Gulf War—The Danish Gulf War study. APMIS. 2001;109:517–524. doi: 10.1111/j.1600-0463.2001.apm090705.x. doi:10.1111/j.1600-0463.2001.apm090705.x [DOI] [PubMed] [Google Scholar]
- Brown M. Toxicological assessments of Gulf War veterans. Phil. Trans. R. Soc. B. 2006;361:649–679. doi: 10.1098/rstb.2006.1825. doi:10.1098/rstb.2006.1825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalder T, Hotopf M, Hull L, Ismail K, David A, Wessely S. Prevalence of Gulf war veterans who believe they have Gulf war syndrone: questionnaire study. BMJ. 2001;323:473–476. doi: 10.1136/bmj.323.7311.473. doi:10.1136/bmj.323.7311.473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Gulf War and Health. National Academy of Science; Washington, DC: 2004. Gulf War and health: updated literature review of Sarin. [PubMed] [Google Scholar]
- Dandeker C. On the need to be different: military uniqueness and civil–military relations in modern society. RUSI J. 2001;146:4–9. [Google Scholar]
- David A, Wessely S. The legend of Camelford: medical consequences of a water pollution accident. J. Psychosom. Res. 1995;39:1–10. doi: 10.1016/0022-3999(94)00085-j. doi:10.1016/0022-3999(94)00085-J [DOI] [PubMed] [Google Scholar]
- Davis L, et al. Clinical and laboratory assessment of distal peripheral nerves in Gulf War veterans and spouses. Neurology. 2004;63:1070–1077. doi: 10.1212/01.wnl.0000138426.88460.cb. [DOI] [PubMed] [Google Scholar]
- De Vries M, Soetekouw P.M.M.B, van der Meer J.W.M, Bleijenberg G. Fatigue in Cambodia veterans. Q. J. Med. 2000;93:283–289. doi: 10.1093/qjmed/93.5.283. [DOI] [PubMed] [Google Scholar]
- Doyle P, Maconochie N, Ryan M. Reproductive health of Gulf War veterans. Phil. Trans. R. Soc. B. 2006;361:571–584. doi: 10.1098/rstb.2006.1817. doi:10.1098/rstb.2006.1817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durodié B. Risk and the social construction of ‘Gulf War Syndrome’. Phil. Trans. R. Soc. B. 2006;361:689–695. doi: 10.1098/rstb.2006.1827. doi:10.1098/rstb.2006.1827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel C. Post-war syndromes: illustrating the impact of the social psyche on notions of risk, responsibility, reason, and remedy. J. Am. Acad. Psychoanal. Dyn. Psychiatry. 2004;32:321–334. doi: 10.1521/jaap.32.2.321.35275. doi:10.1521/jaap.32.2.321.35275 [DOI] [PubMed] [Google Scholar]
- Engel C, Adkins J, Cowan D. Caring for medically unexplained symptoms after toxic environmental exposure: the effect of contested causation. Environ. Health Persp. 2002;110(Suppl. 4):641–647. doi: 10.1289/ehp.02110s4641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel C.C, Hyams K.C, Scott K. Managing future Gulf War Syndromes: international lessons and new models of care. Phil. Trans. R. Soc. B. 2006;361:707–720. doi: 10.1098/rstb.2006.1829. doi:10.1098/rstb.2006.1829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford J, Campbell K, Storzbach D, Binder L, Anger W.K, Rohlman D. Postraumatic stress symptomatology is associated with unexplained illness attributed to Persian Gulf War military service. Psychosom. Med. 2001;63:842–849. doi: 10.1097/00006842-200109000-00019. [DOI] [PubMed] [Google Scholar]
- Freedman L. The official history of the Falklands campaign: war and diplomacy. vol. II. Frank Cass; London: 2005. [Google Scholar]
- Freedman L, Karsh E. Faber and Faber; London, UK: 1993. The Gulf conflict, 1990–91: diplomacy and war in the new world order. [Google Scholar]
- Fullerton C, Ursano R. Behavioral and psychological responses to chemical and biological warfare. Mil. Med. 1990;155:54–59. [PubMed] [Google Scholar]
- Gackstetter G, et al. Assessing the potential health impact of the 1991 Gulf War on Saudi Arabian National Guard Soldiers. Int. J. Epidemiol. 2005;34:801–808. doi: 10.1093/ije/dyi008. doi:10.1093/ije/dyi008 [DOI] [PubMed] [Google Scholar]
- Gifford R.K, Ursano R.J, Stuart J.A, Engel C.C. Stress and stressors of the early phases of the Persian Gulf War. Phil. Trans. R. Soc. B. 2006;361:585–591. doi: 10.1098/rstb.2006.1818. doi:10.1098/rstb.2006.1818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmour B. Edmonton Journal. 1999. Hazardous duty. 9 September 1999. [Google Scholar]
- Glass D.C, Sim M.R. The challenges of exposure assessment in health studies of Gulf War veterans. Phil. Trans. R. Soc. B. 2006;361:627–637. doi: 10.1098/rstb.2006.1822. doi:10.1098/rstb.2006.1822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray G.C, Kang H.K. Healthcare utilization and mortality among veterans of the Gulf War. Phil. Trans. R. Soc. B. 2006;361:553–569. doi: 10.1098/rstb.2006.1816. doi:10.1098/rstb.2006.1816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray G, Smith T.C, Knoke J.D, Heller J.M. The postwar hospitalization experience of gulf war veterans possibly exposed to chemical munitions destruction at Khamisiyah, Iraq. Am. J. Epidemiol. 1999;150:532–540. doi: 10.1093/oxfordjournals.aje.a010043. [DOI] [PubMed] [Google Scholar]
- Gray G, Chesbrough K, Ryan M, Amoroso P, Boyko E, Gackstetter G, Hooper T, Riddle J. Millennium cohort study group. The Millennium Cohort Study: a 21-year prospective cohort study of 140,000 military personnel. Mil. Med. 2002;167:483–488. [PubMed] [Google Scholar]
- Haley R, Kurt T, Hom J. Is there a Gulf War syndrome? Searching for syndromes by factor analysis of symptoms. J. Am. Med. Assoc. 1997;277:215–222. doi:10.1001/jama.277.3.215 [PubMed] [Google Scholar]
- Hoge C, Castro C, Messer C, McGurk D, Cotting D, Koffman R. Combat duty in Iraq and Afganistan, mental health problems, and barriers to care. N. Engl. J. Med. 2004;351:13–22. doi: 10.1056/NEJMoa040603. doi:10.1056/NEJMoa040603 [DOI] [PubMed] [Google Scholar]
- Holloway H, Norwood A.E, Fullerton C.S, Engel C.C, Jr, Ursano R.J. The threat of biological weapons: prophylaxis and mitigation of psychological and social consequences. J. Am. Med. Assoc. 1997;278:425–427. doi:10.1001/jama.278.5.425 [PubMed] [Google Scholar]
- Horner R, et al. Occurence of amyotrophic lateral sclerosis among Gulf War veterans. Neurology. 2003;61:742–749. doi: 10.1212/01.wnl.0000069922.32557.ca. [DOI] [PubMed] [Google Scholar]
- Hotopf M, Wessely S. Can epidemiology clear the fog of war? Lessons from the first Gulf War. Int. J. Epidemiol. 2005;34:791–800. doi: 10.1093/ije/dyi102. doi:10.1093/ije/dyi102 [DOI] [PubMed] [Google Scholar]
- Hotopf M, David A, Hull L, Ismail K, Unwin C.E, Wessely S. The role of vaccinations as risk factors for ill-health in veterans of the Persian Gulf War. BMJ. 2000;320:1363–1367. doi: 10.1136/bmj.320.7246.1363. doi:10.1136/bmj.320.7246.1363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishoy T, Suadicani P, Guldager B, Appleyard M, Hein H.O, Gyntelberg F. State of health after deployment in the Persian Gulf: the Danish Gulf War study. Dan. Med. Bull. 1999;46:416–419. [PubMed] [Google Scholar]
- Ismail K, Lewis G. Multi-symptom illnesses, unexplained illness and Gulf War Syndrome. Phil. Trans. R. Soc. B. 2006;361:543–551. doi: 10.1098/rstb.2006.1815. doi:10.1098/rstb.2006.1815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones E. Historical approaches to post-combat disorders. Phil. Trans. R. Soc. B. 2006;361:533–542. doi: 10.1098/rstb.2006.1814. doi:10.1098/rstb.2006.1814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilshaw S. Friendly fire. Anthropol. Med. 2004;11:149–160. doi: 10.1080/13648470410001678659. doi:10.1080/13648470410001678659 [DOI] [PubMed] [Google Scholar]
- Kilshaw S. On being a Gulf veteran: an anthropological perspective. Phil. Trans. R. Soc. B. 2006;361:697–706. doi: 10.1098/rstb.2006.1828. doi:10.1098/rstb.2006.1828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinman A. University of California Press; Berkeley, CA: 1988. Patients and healers in the context of culture: an exploration of the borderland between anthropology, medicine, and psychiatry. [Google Scholar]
- Kondro W. Soldiers claim ill health after contact with contaminated soil in Croatia. Lancet. 1999;354:494. doi: 10.1016/S0140-6736(05)75529-X. doi:10.1016/S0140-6736(05)75529-X [DOI] [PubMed] [Google Scholar]
- Lawrie S, MacHale S, Power M, Goodwin G. Is the chronic fatigue syndrome best understood as a primary disturbance of the sense of effort? Psychol. Med. 1997;27:995–999. doi: 10.1017/s0033291797005370. doi:10.1017/S0033291797005370 [DOI] [PubMed] [Google Scholar]
- Lewis T. 2nd edn. Shaw; London: 1940. The soldier's heart and the effort syndrome. [Google Scholar]
- McCauley L, Lasarev M, Sticker D, Rischitelli D.G, Spencer P.S. Illness experience of Gulf War veterans possibly exposed to chemical warfare agents. Am. J. Prev. Med. 2002;23:200–206. doi: 10.1016/s0749-3797(02)00497-x. doi:10.1016/S0749-3797(02)00497-X [DOI] [PubMed] [Google Scholar]
- Neutra R. Epidemiology for and with a distrustful community. Environ. Health Perspect. 1985;62:393–397. doi: 10.1289/ehp.8562393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nisenbaum R, Barrett D.H, Reyes M, Reeves W.C. Deployment stressors and a chronic multisymptom illness among Gulf War veterans. J. Nerv. Ment. Dis. 2000;188:259–266. doi: 10.1097/00005053-200005000-00002. doi:10.1097/00005053-200005000-00002 [DOI] [PubMed] [Google Scholar]
- O’ Brien L, Payne R.G. Prevention and management of panic in personnel facing a chemical threat—lessons from the Gulf. J. R. Army Med. Corps. 1993;139:41–45. doi: 10.1136/jramc-139-02-02. [DOI] [PubMed] [Google Scholar]
- Peakman M, Skowera A, Hotopf M. Immunological dysfunction, vaccination and Gulf War illness. Phil. Trans. R. Soc. B. 2006;361:681–687. doi: 10.1098/rstb.2006.1826. doi:10.1098/rstb.2006.1826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrie K.J, Broadbent E, Kley N, Moss-Morris R, Horne R, Rief W. Worries about modernity predict symptom complaints following environmental spraying. Psychosom. Med. 2005;67:778–782. doi: 10.1097/01.psy.0000181277.48575.a4. [DOI] [PubMed] [Google Scholar]
- Proctor S, et al. Health status of Persian Gulf War veterans: self-reported symptoms, environmental exposures, and the effect of stress. Int. J. Epidemiol. 1998;27:1000–1010. doi: 10.1093/ije/27.6.1000. doi:10.1093/ije/27.6.1000 [DOI] [PubMed] [Google Scholar]
- Riddle J.R, Brown M, Smith T, Ritchie E.C, Brix K.A, Romano J. Chemical warfare and the Gulf War: a review of the impact on gulf veterans' health. Mil. Med. 2003;168:600–605. [PubMed] [Google Scholar]
- Roht L, Vernon S.W, Weir F.W, Pier S.M, Sullivan P, Reed L.J. Community exposure to hazardous waste disposal sites: assessing reporting bias. Am. J. Epidemiol. 1985;122:418–433. doi: 10.1093/oxfordjournals.aje.a114123. [DOI] [PubMed] [Google Scholar]
- Rook G, Zumla A. Gulf war syndrome: is it due to a systemic shift in cytokine balance towards a Th2 profile? Lancet. 1997;349:1831–1833. doi: 10.1016/S0140-6736(97)01164-1. doi:10.1016/S0140-6736(97)01164-1 [DOI] [PubMed] [Google Scholar]
- Rose M.R, Brix K.A. Neurological disorders in Gulf War veterans. Phil. Trans. R. Soc. B. 2006;361:605–618. doi: 10.1098/rstb.2006.1820. doi:10.1098/rstb.2006.1820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharief M, Pridden J, Delamont R, Rose M, Unwin C, Hull L, David A. Neurophysiologic evaluation of neuromuscular symptoms in UK Gulf War veterans. A controlled study. Neurology. 2002;59:1518–1525. doi: 10.1212/01.wnl.0000032755.27372.fc. [DOI] [PubMed] [Google Scholar]
- Shriver T, Webb G, Adams B. Environmental exposures, contested illness, and collective action: the controversy over Gulf War illness. Humboldt J. Soc. Relat. 2002;27:73–105. [Google Scholar]
- Slottje P, et al. Epidemiologic study of the autoimmune health effects of a cargo aircraft disaster. Arch. Intern. Med. 2005;165:2278–2285. doi: 10.1001/archinte.165.19.2278. doi:10.1001/archinte.165.19.2278 [DOI] [PubMed] [Google Scholar]
- Slovic P. Trust, emotion, sex, politics, and science: surveying the risk assessment battlefield. Risk Anal. 1999;19:689–702. doi: 10.1023/a:1007041821623. doi:10.1023/A:1007041821623 [DOI] [PubMed] [Google Scholar]
- Slovic P, Malmfors T, Krewski D, Mertz C.K, Neil N, Bartlett S. Intuitive toxicology. II. Expert and lay judgements of chemical risks in Canada. Risk Anal. 1995;15:661–675. [Google Scholar]
- Soetekouw P, De Vries M, Preijers F.W, Van Crevel R, Bleijenberg G, Van Der Meer J.W. Persistent symptoms in former UNTAC soldiers are not associated with shifted cytokine balance. Eur. J. Clin. Invest. 1999;29:960–963. doi: 10.1046/j.1365-2362.1999.00545.x. doi:10.1046/j.1365-2362.1999.00545.x [DOI] [PubMed] [Google Scholar]
- Spencer P, McCauley L.A, Lapidus J.A, Lasarev M, Joos S.K, Storbach D. Self-reported exposures and their association with unexplained illness in a population based case-control study of Gulf War veterans. J. Occup. Environ. Med. 2001;43:1041–1056. doi: 10.1097/00043764-200112000-00006. [DOI] [PubMed] [Google Scholar]
- Squibb K.S, McDiarmid M.A. Depleted uranium exposure and health effects in Gulf War veterans. Phil. Trans. R. Soc. B. 2006;361:639–648. doi: 10.1098/rstb.2006.1823. doi:10.1098/rstb.2006.1823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stimpson N.J, Thomas H.V, Weightman A.L, Dunstan F, Lewis G. Psychiatric disorders in veterans of the Persian Gulf War of 1991. Systematic review. Br. J. Psychiatry. 2003;182:391–403. doi:10.1192/bjp.182.5.391 [PubMed] [Google Scholar]
- Stokes J, Banderet L. Psychological aspects of chemical defense and warfare. Mil. Psychol. 1997;9:395–415. doi:10.1207/s15327876mp0904_8 [Google Scholar]
- Storzbach D, Campbell K.A, Binder L.M, McCauley L, Anger W.K, Rohlman D.S, Kovera C.A. Psychological differences between veterans with and without Gulf War unexplained symptoms. Psychosom. Med. 2000;62:726–735. doi: 10.1097/00006842-200009000-00017. [DOI] [PubMed] [Google Scholar]
- Stuart J, Ursano R.J, Fullerton C.S, Norwood A.E, Murray K. Belief in exposure to terrorist agents: reported exposure to nerve or mustard gas by Gulf War veterans. J. Nerv. Ment. Dis. 2003;191:431–436. doi: 10.1097/01.NMD.0000081634.28356.6B. [DOI] [PubMed] [Google Scholar]
- Unwin C, et al. The health of United Kingdom Servicemen who served in the Persian Gulf War. Lancet. 1999;353:169–178. doi: 10.1016/S0140-6736(98)11338-7. doi:10.1016/S0140-6736(98)11338-7 [DOI] [PubMed] [Google Scholar]
- Vasterling J.J, Bremner J.D. The impact of the 1991 Gulf War on the mind and brain: findings from neuropsychological and neuroimaging research. Phil. Trans. R. Soc. B. 2006;361:593–604. doi: 10.1098/rstb.2006.1819. doi:10.1098/rstb.2006.1819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wessely S, Unwin C, Hotopf M, Hull L, Ismail K, Nicolaou V, David A. Is recall of military hazards stable over time? Evidence from the Gulf War. Br. J. Psychiatry. 2003;183:314–322. doi: 10.1192/bjp.183.4.314. doi:10.1192/bjp.183.4.314 [DOI] [PubMed] [Google Scholar]
- Wheelwright J. Norton; New York: 2001. The irritable heart. [Google Scholar]
- Winters W.D, et al. Media warnings about environmental pollution facilitate the acquisition of symptoms In response to chemical substances. Psychosom. Med. 2003;65:332–338. doi: 10.1097/01.psy.0000041468.75064.be. doi:10.1097/01.PSY.0000041468.75064.BE [DOI] [PubMed] [Google Scholar]
- Yzermans J, Gersons B. The chaotic aftermath of an airplane crash in Amsterdam: a second disaster. In: Havenaar C.J, Bromet E.J, editors. Toxic turmoil: psychological and societal consequences of ecological disasters. Plenum Press; New York: 2002. pp. 85–99. [Google Scholar]
- Zavestoski S, Brown P, Linder M, McCormick S, Mayer B. Science, policy, activism, and war: defining the health of Gulf war veterans. Sci. Technol. Human Values. 2002;27:171–205. [Google Scholar]
- Zavestoski S, Brown P, McCormick S, Mayer B, Ottavi M, Lucove J. Patient activism and the struggle for diagnosis: Gulf War illness and other medically unexplained physical symptoms in the US. Social Sci. Med. 2004;58:161–175. doi: 10.1016/s0277-9536(03)00157-6. doi:10.1016/S0277-9536(03)00157-6 [DOI] [PubMed] [Google Scholar]