Abstract
Objectives
To describe a collaborative undertaking between a private school of pharmacy (Bernard J. Dunn School of Pharmacy) and a public high school (John Handley High School) in the development, and implementation of a partnership utilizing high school theater students as standardized patients.
Methods
High school theater students were trained to portray patients within the Standardized Patient Assessment Laboratory. The patient encounters were videotaped and evaluated by both peer and faculty members. Quantitative and qualitative analyses of semi-structured interviews, focus groups, post-encounter surveys of students and faculty members, and encounter grades were used to evaluate the outcomes.
Results
Pharmacy students exhibited competence in clinical assessment skills as evidenced by high encounter grades (91.5% ± 6.8%) and 100% positive faculty feedback. The high school theater students self-reported that their improvisational skills improved through learning patient conditions and behaviors. Both schools met their mission statement and accreditation goals, including increased collaboration with the community.
Conclusion
This model for collaboration between a school of pharmacy and a high school using adolescents as simulated patients was successful in creating a beneficial learning experience for both the theater and pharmacy students.
Keywords: simulated patients, standardized patients, community collaboration, patient counseling, assessment
INTRODUCTION
The Standardized Patient Assessment Laboratory (SPAL) at the Bernard J. Dunn School of Pharmacy introduces pharmacy students to the basic skills of physical assessment necessary for monitoring drug therapy. SPAL is designed to enable students to become proficient in patient assessment and evaluation, interpersonal communication, and problem resolution. This laboratory and teaching methodology allows the application and refinement of interpersonal communication skills and provides an opportunity for the students to incorporate their didactic knowledge from previous curriculum courses in the setting of a simulated patient care encounter. SPAL serves to assist in preparing the pharmacy student for entry into the patient care environment.
In order for SPAL experience to provide as rich a learning experience as possible, highly trained standardized patients must be available and reliable. It is this need that led Shenandoah University Bernard J. Dunn School of Pharmacy to collaborate with the theater program at John Handley High School. The innovative collaboration with the Theatre Department at Winchester City Public Schools produced an extremely successful pharmacy simulated patient encounter as evidenced by outcomes from the pharmacy students, high school theater students, and faculty members from both the public high school and pharmacy school.
This collaborative effort called for the integration of education, health, and human service systems to create an effective learning environment, a concept fundamental to the improvement of educational instruction and quality. Each party to such a collaboration realized specific benefits of their own while helping group partners as a whole to achieve their goals.1-2
It was mutually recognized by faculty members in both schools that no single profession possessed the full compliment of resources and technical insight to create the most viable and effective learning arena for SPAL. As a team, however, both schools provided their respective students with new opportunities to exercise their skills in real-world settings with measurable effective outcomes for students and faculty members alike. This innovative approach addressed the need for well-trained simulated patients and helped to narrow an observable shortage of trained adolescents in that role.3-5 Both the pharmacy and public high schools accomplished the goal of their individual mission statements for increasing collaborative educational efforts with one another.
Bernard J. Dunn School of Pharmacy: To stimulate excellence, innovation, and collaboration in a professional environment that fosters the development of lifelong learners committed to advancing pharmacy's role in health care and serving the community with integrity and compassion.6
John Handley High School, Winchester City Public Schools: To develop and implement regional services in cooperation with other school divisions and institutions of higher education.7
Prior to the fall of 2004, the role of simulated patient was most often filled by pharmacy faculty members and/or first-professional year students. Many students expressed an inability to embody a role of expertise or authority knowing that the simulated patient was a professor who silently critiqued their every word, action, or omission. Additionally, dialogue with a pharmacy professor or student often lacked the conversational qualities normally encountered with actual patients.
Partnership with the local high school theater department provided a group of actors who brought not only dramatic skill but youthful enthusiasm and a wealth of contemporary jargon that added genuine realism to the exercise. The idea for partnering with the local high school theater students arose from the need and commitment to:
(1) Provide more objective and realistic patient encounters for the pharmacy students.
(2) Establish an ongoing collaboration between the school of pharmacy and high school.
(3) Provide real life opportunities for improvisation for the high school students which extended beyond the classroom.
The literature is replete with the efficacy of standardized patients in formative and summative assessments in health care.8-11 Medical schools have employed paid actors with dramatic skills to train their students in patient assessment.12-13 The use of adolescent and pediatric simulated patients is rare among medical schools, but in instances where they have been thus employed, both students and faculty members have responded favorably regarding the benefits of such encounters.3-5 This exercise is novel in that high school students with a theater course requirement were utilized to interact with pharmacy students in a professional patient encounter.
DESIGN
Shenandoah University Bernard J. Dunn School of Pharmacy has a simulated ambulatory clinic comprised of 6 patient rooms that are each monitored by a video camera. Each room contains a blood pressure monitor, sink, gurney, and counseling area. A control room, separate from the clinic rooms, consists of video cassette recorders and television sets. Each pharmacy student and simulated patient is given a room and time assignment, with the goal that 75 pharmacy students each complete 1 encounter within 20 minutes over a period of 6 hours divided into 2 days. Faculty members observe and evaluate the students during the live encounters using a consistent form.
Prior to beginning our research, this study was approved by the Institutional Review Board of Shenandoah University. For 2 consecutive years, trained high school theater students served as simulated patients for third- and fourth-professional year pharmacy students in patient encounter interviews. A large investment in time (approximately 4 months) was necessary for pharmacy faculty members to coordinate with the high school theater instructor and students to plan and train for the collaboration. Pharmacy faculty members visited the high school students 4 different times for a 1-hour block during drama class to distribute the case scenarios, present sample encounters, and explain the disease state from the patient's perspective prior to each set of encounters. The high school students were prepared for each encounter through detailed descriptions of the patient, role playing with pharmacy faculty members, and observation of previous encounters on video. In 2004, the high school students were given latitude to develop the patient, in terms of emotional state, age, and severity of the situation. In 2005, the cases were made more specific and included a chief complaint, possible pharmacist questions, the problem, and possible suggestions the pharmacist may relay. The high school students were given specific directions and were more restricted in their presentation of the patient. This change was made to better prepare the high school students so that their improvisation would be perceived as realistic by the pharmacy students.
The cases were developed by pharmacy faculty members who are practicing pharmacists and the design required the pharmacy students to ask numerous questions of the patient. In the fall, the first encounter, patient triage, was used for practice and the evaluation score was not recorded but shared with the student for feedback and suggestions for improvement. The triage encounters in 2004 consisted of ambulatory care cases including: cough and cold, infected wood splinter, suspected pregnancy, dog bite, medication adverse event, minor burn, and poison ivy. Special-effects make-up was actually applied to some of the high school students in an attempt to make the encounter more realistic. In 2005, the triage encounters were adjusted to include solely dermatologic cases, since an ambulatory care pharmacist in a retail setting would be more likely to counsel in this type of situation, and some of the earlier triage cases were too severe for a pharmacist to handle (ie, dog bite, infected wood splinter). The cases included atopic dermatitis, poison ivy, psoriasis, fungal skin infection, minor burn, and medication allergic reaction (Appendix 1). In 2005, make up was not applied to the patients. Instead, a card with an image of the specific skin reaction was presented by the patient to the pharmacist.
The second encounter, smoking cessation, was evaluated for an actual grade and comprised a third of the total course grade. The smoking cessation encounter involved a realistic scenario in which a patient is considering quitting smoking and wants advice on nonprescription and prescription nicotine products (Appendix 2). The pharmacy student was expected to ask questions to determine the patient's motivation and commitment, as well as to discern contraindications to nicotine products in order to select the most appropriate plan for the patient. The evaluation form for this encounter was modified to identify 5 specific competencies that were necessary to effectively counsel a smoking cessation patient.
(1) Uses appropriate communication skills.
(2) Seeks and uses patient-provided information to gather evidence or to provide direction.
(3) Assesses any actual and/or potential concerns or problems of importance to or about the patient.
(4) Uses language the patient is likely to understand.
(5) Conveys complete information to the patient where appropriate.
Both the pharmacy and high school students had the opportunity to view the videotaped encounters later in the semester. The pharmacy students evaluated each other in groups of 6, using the same evaluation forms that the faculty member used. The high school students viewed each of the encounters as a group with their theater instructor. Peers provided verbal feedback in each situation.
Prior to and after the simulated patient encounters, the authors conducted semi-structured interviews with the director of the theater program at the high school in order to gain an understanding of expectations, perceived purpose of participation, and self-reported outcomes. A randomly selected group of 10 students who participated as simulated patients in 2004 and/or 2005 responded to the following questions:
(1) How did you feel before your first encounter?
(2) How did you feel after the first encounter?
(3) What did you like about the encounters?
(4) What did you dislike about the encounters?
(5) Was enough instruction given before the encounters?
(6) What would have made you feel more prepared for the encounters?
(7) Did the traits of pharmacy students affect your improvisation and behavior?
(8) How did the pharmacy students react to you?
(9) Did you feel you were taken seriously by the pharmacy students?
(10) What would have made the encounters more useful?
(11) If applicable, did you feel that the make-up for the first encounters helped your improvisation?
(12) How did the pharmacy students react to the make-up?
(13) What did you learn from the encounters?
(14) Do you feel that you can apply the things you learned from this experience to your life in general?
In order to establish a solid explanation and understanding of the data collected from the responses to the above questions, the qualitative research approach was that of coding and creating categories in an open coding system. This method is a systematic and precise analysis of data in which initial categories of information of subject matter are formed. Open coding allows for general or initial categories to be identified. The data of the student responses were considered in minute detail.14-15 Within each category, the authors discovered several properties or subcategories. This approach allowed the researchers to form theoretical ideas and interrelated hypotheses as described in the Results section.
The 14 questions were posed to the high school theater students in order to discover their perceived experience as simulated patients, their reported level of preparation, their interactions with the pharmacy students, and what they learned from the experience. From their responses, 3 themes were generated. The authors verified the findings with the high school students as well as the theater director.
Quantitative Analysis: Pharmacy School
Third- (N = 75) and fourth-professional year (N = 68) pharmacy students used Survey Monkey to complete a post-questionnaire using a Likert-like scale. Pearson Chi-square (computed for a 2x2 table) and Fisher's exact test statistics were analyzed to examine students' perceptions regarding the patient encounter environment and its effect on the following clinical skills: interpersonal communications, professionalism, patient counseling, clinical problem-solving process, evaluation of drug-related problems, and collection of pertinent patient information.
The 75 grades for the 2005 smoking cessation encounter were compiled and a mean competency in assessed clinical skills was calculated. For reasons of confidentiality, the actual faculty and peer evaluations were returned to the students at the end of each academic year. Therefore, a detailed accounting of each of the clinical skills in these assessments could not be completed. Also, the encounter grades for 2004 were unavailable.
A survey instrument with the same questions that were asked of the students was completed by all 3 of the faculty members who actually evaluated the patient encounters. Two additional questions were included to determine whether the encounter grades were adversely affected by the use of high school students and whether they accurately reflected students' competence in the assessed clinical skills.
ASSESSMENT
Qualitative: High School
The qualitative research utilizing the analysis and process described in the methods section revealed 3 major themes:
(1) A commitment and eagerness on the part of the participants from the high school theater department to continue with the partnership between the pharmacy school and the high school.
(2) The educational experience and growth of the theater students who participated was rich with new and real-life improvisational opportunities.
(3) The desire on the part of the theater students to be creative needed to be tempered with study and focus on the disease states and conditions of the patient they were to portray.
The director of the theater program at the high school expressed that the simulated patient encounters provided a community service opportunity for the drama students. Both the director and the high school students stated that they gained a real appreciation for the amount of material pharmacy students must learn and how they are assessed. The high school students self-reported increased confidence in their acting abilities in being able to immerse themselves into their roles to create a real situation. The pharmacy students (82.4%) and faculty (100%) corroborated the realism of the encounter in their survey responses. The director graded the high school students on their level of participation and research into the disease state prior to the encounter. The high school students honed their improvisational skills and willingly gave their time to the pharmacy students. The one obstacle mentioned was convincing the non-theater instructors at the high school that taking time away from their courses was worth the experience with the pharmacy school. Once these students participated in the simulated patient encounters, they self-reported that this was a valuable experience which they would want to repeat.
From their statements during the focus group, all of the high school students were very concerned about responding in a realistic manner and reported being more nervous for the pharmacy students, since the pharmacy students were being graded for the encounters. Half of the high school students were concerned that the first encounter with a pharmacy student was a rehearsal and that the first few pharmacy students did not get a complete experience. All of the high school students were cognizant of the fact that they could not deviate too far from the guidelines that were given to them to prevent supplying incorrect information to the pharmacy students. They wanted to be realistic and provide the correct symptoms, since they were actually portraying people with real illnesses and legitimate problems. Before the first encounter, all of the high school students stated they did not know what to expect, so they were apprehensive about the types of questions that would be asked by the pharmacy students. After the first encounter, all of the theater students self-reported during the debriefing interview that they felt much more confident in their abilities to communicate and interact in a serious manner. The high school director of the theater program verified this finding as he reviewed SPA scenarios with the students in subsequent high school classes.
All of the high school students stated that they enjoyed the experience and looked forward to the encounters. They reported that their improvisational skills were greatly improved, which was corroborated by the director, and learned useful tips from watching their classmates play their roles on video. Prior to the establishment of the collaboration, the high school students normally only interacted with their classmates, who they knew well, and therefore could predict their responses. The encounters introduced new areas that were true to life as opposed to classroom improvisation exercises, which became routine and predictable. The students reported they learned useful tips from watching their classmates perform their characters on video, and shared strategies and techniques with one another after the encounters. The high school students practiced their patient roles with each other, which brought them closer together as a group. They reported that the directed case description and guidelines for the patient role assisted in focusing them to make their presentations more realistic and believable and that the clinic rooms made the encounters more realistic, similar to a setting in a play.
Twenty percent of the high school students who participated in 2004 reported that their preparation was not sufficient to feel confident in their presentation and would have liked more practice with pharmacy faculty members. In contrast, the pharmacy students (82.4%) and faculty members (100%) responded that the high school students were well-trained and prepared. The case description and guidelines for the patient helped to focus them to make their presentations more complete and believable, but the students suggested including major and minor symptoms, how the patient feels and appears, along with any other useful information applicable to the disease state. The students stayed in character and acted through the symptoms of their disease state when they had to create an answer to an unfamiliar question. The high school students reported that some of the encounters were too simple and one-sided, especially those in which the interaction was limited, such as when the pharmacy student simply gave instructions regarding a medication or knew the disease state immediately.
All of the high school students expressed that the pharmacy students seemed very nervous throughout the encounters, primarily due to the videotaping and grading, which made them take their roles seriously. They reported that the pharmacy students took them more seriously when they used make-up and displayed intense emotions. For example, one high school student actually cried during the encounter, which made the pharmacy student fumble for questions and show true concern for the high school student's welfare.
Quantitative-Pharmacy Students
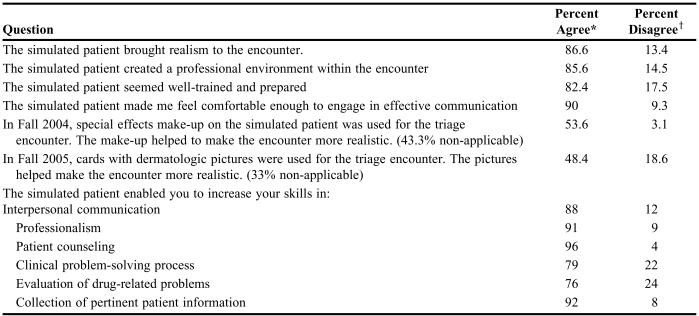
The response rate to the survey was 68% (97/143) and the results are presented in Table 1. The majority of pharmacy students responded that the simulated patient brought realism to the encounter (86.6%). The pharmacy students reported that the high school students were well-trained and prepared (82.4%), despite the fact that some high school students would have liked more time for training.
Table 1.
Survey Responses Reflecting Pharmacy Student Feedback Regarding Use of High School Students as Simulated Patients (N = 97)
*The Likert scale responses of strongly agree and agree were combined
†The Likert scale responses of strongly disagree and disagree were combined
Although the high school students enjoyed using the special-effects make-up for the triage encounter, only half of the pharmacy students reported that this feature helped to make the encounter more realistic (53.6%). One pharmacy student commented, “When they [high school students] used the stage make up to simulate burns and cuts, it was very realistic. It is obvious that the students enjoy the roll-playing [sic]. They were always very professional.”
In the survey, the pharmacy students responded that the high school simulated patients enabled them to increase their clinical skills in communication, professionalism, patient counseling, problem-solving, evaluation of drug-related problems, and collection of patient information. Encounter grades for the 2005 smoking cessation were 91.5% ± 6.8%. Pharmacy faculty members agreed that the encounter grades accurately reflected the students' level of competence in the clinical skills assessed during the encounters (100%). Additionally, pharmacy faculty members responded that the high school students did not adversely affect the encounter grades (100%).
Pharmacy students felt that the high school students created a comfortable environment which allowed them to engage in effective communication (90.7%), which they believed specifically increased their skills in interpersonal communications (p = 0.001) and collection of pertinent patient information (p = 0.025). Open comments from the students that related to the patient encounter environment were:
“I reported as though I was actually interacting with a patient. After, I reported encouraged to do further research on treating the patient's condition. I reported the encounter was realistic.”
“It brought reality to the classroom setting. It was very similar to a real life experience and increase communication skills. I even think more encounters would be beneficial.”
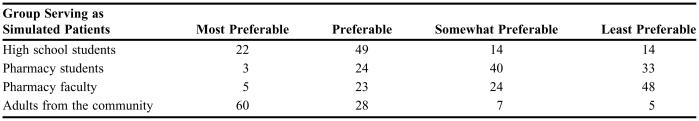
The pharmacy students voiced a preference in terms of the types of groups used as simulated patients (Table 2). Pharmacy faculty members ranked their preference for the types of groups in the same order as the students (100%). When asked if high school students, pharmacy students, pharmacy faculty members, and adults from the community are equally preferable for use as simulated patients, the pharmacy students overwhelmingly responded in the negative (90.7%). By ranking most preferable to least preferable, the pharmacy students chose adults from the community, high school students, pharmacy students, and pharmacy faculty members, respectively. Some of the insightful open comments that related to this preference were:
Table 2.
Pharmacy Students' Preferences for Who Should Serves as Simulated Patients (N = 97)
“I believe the students from high school made it more realistic than having students counsel fellow students in pharmacy school.”
“I was less nervous because I knew it would not be a fellow student or a professor.”
“When a classmate was a simulated patient, it was hard to take the scenario seriously. It also added to my nervousness. Faculty significantly increase the nervousness potential. I think the students from Handley High School were the best.”
“It was a good experience but I would rather counsel an adult.”
DISCUSSION
The American Association of Colleges of Pharmacy's Center for the Advancement of Pharmaceutical Education (CAPE) Educational Outcomes dictates that pharmacy graduate competencies include providing patient-centered care through communication and collaboration with patients, professionalism, critical thinking, and problem-solving.16 Trained standardized patients provide students with the opportunity to practice these clinical skills in a controlled environment prior to interacting with the general public during clinical rotations. Pharmacy students have expressed a clear preference for non-pharmacy participants, both to decrease the anxiety level and to provide a more realistic patient encounter. Although the use of standardized patients has increased throughout pharmacy education, the employment of adolescents in this role is still limited despite a clear professional requirement to provide counseling to youthful patients in actual practice.
An open and effective partnership between the school of pharmacy and high school ensured the success of using adolescents as simulated patients. Participating faculty members from both schools reported that the time dedicated to defining expectations, obligations, and goals was well-spent and contributed significantly to the success of the exercise. It is imperative that adequate time be budgeted prior to, during, and after the simulated patient encounters.
Live viewing of each simulated patient encounter by the high school students and pharmacy faculty members allowed for immediate feedback and discussion of effective encounters, including strategies for improvement. Both pharmacy and high school students self-reported that they learned by watching their peers and were able to incorporate effective behaviors into subsequent encounters. High encounter grades supported the students' self-report that they learned from their peers. Encounter sessions were scheduled over intervals of several weeks, allowing students significant windows of time to review session videotapes and improve their performances through instruction, group analysis, critique, and practice. One additional evaluation that is necessary to the success of both groups of students is to schedule extra time after each encounter to allow the pharmacy student and high school patients to assess one another. High school students were extremely concerned regarding the realism of their performance and immediate feedback from the pharmacy students would have been a useful formative tool.
In the true spirit of collaboration, the public high school and private pharmacy school jointly committed to the development of an interprofessional partnership that led to a richer curriculum for both systems, a feeling of clinical competence by the pharmacy students, a greater understanding by high school students and faculty members of the roles of pharmacists in patient counseling, and an increased commitment on the part of theater students to pursue more opportunities for training in patient encounters. In the course of the exercise, both pharmacy students and adolescent simulated patients alike played professional roles within their respective disciplines, realizing parallel benefits common to the encounter. Both parties were motivated to perform as realistically as possible for their own review, creating superior environments for their counterparts.
CONCLUSION
Both the theater and pharmacy students who experienced the simulated patient encounters had the opportunity to participate in realistic improvisation and patient-centered care. This was accomplished through communication and collaboration with each other, professionalism, critical thinking, and problem-solving. The collaboration between Shenandoah University, Bernard J. Dunn School of Pharmacy and Winchester City Schools Theatre Department at John Handley High school is successful and ongoing. The commitment by both institutions to allow adequate time for the faculty to devote to this partnership is critical for the continuation and growth of this project.
ACKNOWLEDGEMENTS
Several faculty members from each institution were actively involved in the planning, implementation, and evaluation of this collaborative endeavor. The investment of time and effort from the following individuals is greatly appreciated: at Handley High School: Larry Lovelady and his theater students; at Bernard J. Dunn School of Pharmacy: Renee Thomas, PharmD, MBA, Sarah Parnapy, PharmD, Denise Blake, MLS, and Wallace Marsh, PhD, MBA.
Appendix 1. Triage Case
PATIENT (Given to high school student)
Chief Complaint
I have these itchy scaly red rings all over my upper body and they are getting worse and nothing is working to get rid of them.
Pharmacist Questions
What is your name?
Use your own name.
How old are you?
Give your age.
Do you have any allergies?
Not that I know of.
How long have you had the rings?
About a week
Have you ever had these rings before?
I remember last summer I got a few, but they went away. I've never had so many at one time and they itch a lot more.
Have you noticed if anything specific makes the rings worse?
I notice that I get more after working out at the gym, especially if I sweat a lot.
Do you use the gym shower right after working out?
No, those showers are gross. I wait and shower at home.
Have you been under more stress lately?
Yes, I have a bunch of mid-terms and projects.
What makes the rings go away?
If I take a shower and really dry myself off well and stay cool, I don't feel as itchy.
Have you tried anything over-the-counter to treat yourself?
No, I have no idea what medicine would help.
How many hours do you sleep at night?
About 7-8.
Are you taking any medications?
No
Your Problem
You appear to have a fungal infection called tinea corporis, probably from being sweaty for a longer period of time and being under more stress.
Pharmacist Suggestions
Recommend self-care with a nonprescription antifungal (patient education sheet)
Recommend non-drug measures (patient education sheet)
If above treatments don't improve rings within a month, see your doctor
Appendix 2. Tobacco Cessation Case
PATIENT (Given to high school student)
STAGE: Ready to Quit
You are an 18-year old who would like some advice on quitting smoking. You never thought it would happen to you, but you are hooked. The first thing you think about in the morning is how fast you can get out of the house to light up a cigarette. You are at the community pharmacy to get some assistance with quitting.
You had your first cigarette in 7th grade but didn't start smoking regularly until 10th grade. You now smoke about 10 cigarettes a day and have never tried to quit before. You are uncomfortable with feeling hooked and hate the way it makes you smell. Your boyfriend/girlfriend doesn't smoke and is constantly nagging you to stop smoking. He/she would be a good support. You do have another boyfriend/girlfriend who smokes and with whom you drive to school each day. You both smoke about 2 cigarettes on the way to school each morning. You've been able to keep it a secret from your parents, but your mom smelled smoke on your clothes last week, so you told her that you had been around some smokers. You feel uncomfortable about lying to your family.
You are confident that you can quit. You have been feeling short of breath during your swim team practices, so you know it is the best thing to do. You are afraid of gaining weight when you quit, since you have to keep in shape for swimming.
One of your friends quit smoking by using the nicotine patch. You would like to try the patch, since it worked for her. You are planning to quit for your New Year's resolution, since you don't think you can quit during the holidays. You are willing to work with the pharmacist, since you do not want your family to know you are doing this.
PHARMACIST (Given to faculty evaluators)
You are a retail pharmacist and have been approached by a teenager who would like your advice on how he/she can quit smoking. He/she wants to quit, but doesn't know how.
STAGE: Ready to Quit
Step 1: ASK
Not applicable. The patient has asked the pharmacist for assistance with quitting.
Step 2: ADVISE
Not applicable. The patient has asked the pharmacist for assistance with quitting.
Step 3: ASSESS
The patient has told you that he/she is ready to quit.
Step 4: ASSIST
Tobacco use history: current use, past use
Reasons/motivation for wanting to quit
Confidence in ability to quit
Social support for quitting
Concerns about weight gain
Routines and situations associated with tobacco use
Facilitate quitting process: recommend tobacco use log, discuss coping strategies, discuss methods for quitting (Patient wants nicotine patch, so instruct on its use and side effects)
Step 5: ARRANGE
Suggest having the patient come back to purchase the patch before Jan 1, when she is ready to quit, so you can reinforce your instructions.
PHARMACIST (Given to pharmacy student)
You are a retail pharmacist and have been approached by a teenager who would like your advice on how he/she can quit smoking. He/she wants to quit, but doesn't know how.
REFERENCES
- 1.Corrigan D. The changing role of schools and higher education institutions with respect to community-based interagency collaboration and interprofessional partnerships. Peabody J Educ. 2000;75:176–95. [Google Scholar]
- 2.Kochan FK, Kunkel RC. The learning coalition: professional development of schools in partnership. J Teacher Educ. 1998;49:325. [Google Scholar]
- 3.Brown R, Doonan S, Shellenberger S. Using children as simulated patients in communication training for residents and medical students: a pilot program. Acad Med. 2005;80:1114–20. doi: 10.1097/00001888-200512000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Hardoff D, Schonmann S. Training physicians in communication skills with adolescents using teenage actors as simulated patients. Med Educ. 2001;35:206–10. doi: 10.1046/j.1365-2923.2001.00764.x. [DOI] [PubMed] [Google Scholar]
- 5.Lane JL, Ziv A, Boulet JR. A pediatric clinical skills assessment using children as standardized patients. Arch Pediatr Adolesc Med. 1999;153:637–44. doi: 10.1001/archpedi.153.6.637. [DOI] [PubMed] [Google Scholar]
- 6. Bernard J. Dunn School of Pharmacy Mission Statement. Available at: http://pharmacy.su.edu/PharmWeb/indexmenu/NavIndex.cfm?fuseaction+MissionSt. Accessed October 15, 2006.
- 7. Winchester Public Schools Plan. Available at: www.wps.k12.va.us/sysinfo/comffplan.pdf. Accessed October 15, 2006.
- 8.Austin A, Tabak D. Design of a new professional practice laboratory course using standardized patients. Am J Pharm Educ. 1998;62:271–9. [Google Scholar]
- 9.Becker KL, Rose LE, Berg JB, et al. The teaching effectiveness of standardized patients. J Nursing Educ. 2006;45:103–11. doi: 10.3928/01484834-20060401-03. [DOI] [PubMed] [Google Scholar]
- 10.Westberg SM, Adams J, Thiede K, et al. An interprofessional activity using standardized patients. Am J Pharm Educ. 2006;70(2) doi: 10.5688/aj700234. Article 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clay MC, Lane H, Willis SE, et al. Using a standardized family to teach clinical skills to medical students. Teach Learn Med. 2000;12:145–9. doi: 10.1207/S15328015TLM1203_5. [DOI] [PubMed] [Google Scholar]
- 12.Fortin QH, Haeseler FD, Angoff N, et al. Teaching pre-clinical medical students an integrated approach to medical interviewing. J Gen Intern Med. 2002;17:704–8. doi: 10.1046/j.1525-1497.2002.00628.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shapiro J, Hunt L. All the world's a stage: the use of theatrical performance in medical education. Med Educ. 2003;37:922–7. doi: 10.1046/j.1365-2923.2003.01634.x. [DOI] [PubMed] [Google Scholar]
- 14.Creswell JW. Thousand Oaks, Calif: Sage Publications, Inc; 1998. Qualitative inquiry and research design: choosing among five traditions. [Google Scholar]
- 15.Glaser BG, Strauss AL. Hawthorne, NY: Aldine de Gruyter; 1999. The discovery of grounded theory: strategies for qualitative research. [Google Scholar]
- 16. Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Standards for Curriculum, Standard 12: Professional Competencies and Outcome Expectations. Adopted January 15, 2006. Available at: http//www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.DOC. Accessed July 18, 2006.